Assessment and management of pain in the adult patient with advanced cancer
One of our expert writers has created this bespoke sample nursing exam revision that shows the quality that is guaranteed with every nursing paper ordered. Secure your academic success and place an order today or view our services.
Introduction
- In the UK, approximately 350,000 individuals develop cancer each year.
- Around 160,000 of those diagnosed will die of the disease.
- The diagnosis of advanced cancer often causes feelings of despondency, futility and fear in cancer patients and their loved ones.
- Advanced stage cancer may be diagnosed at the onset of the disease, may arise because of ongoing disease progression, or may develop following a recurrence after a period of remission.
- In patients with advanced cancer, pain is frequently the most common, and most feared symptom.
- Pain due to advanced cancer is the most under-treated symptom related to the end-of-life; it is thought that pain is under-treated in approximately 50% of cancer patients, despite clear local, national, and international guidelines related to its management.
- Comprehensive holistic assessment is essential for the effective management of cancer pain in the adult patient.
Cancer pain – what causes it, and how does it affect patients?
- Pain due to advanced cancer is complex – it can be both acute and chronic
- Cancer pain can be a direct consequence of the primary pathology – e.g. distant metastases or nerve compression.
- It can also be caused by cancer treatment - e.g. surgery, chemotherapy, radiotherapy.
-
Cancer pain commonly exists as a combination of various mechanisms:
- Somatic – a nociceptive pain arising from skin, tissue, or muscle
- Visceral – a nociceptive pain arising from internal organs
- Nociceptive – chronic pain caused by damage to tissues
- Neuropathic – pain from damage or disease affecting the somatosensory nervous system.
- Uncontrolled pain affects an individual’s response to illness, limits their self-caring ability, and reduces their overall quality of life.
Assessment of cancer pain
- Given the significant impact of poorly managed or uncontrolled pain on patients with advanced cancer, it is essential to undertake an accurate and holistic assessment of the patient’s pain.
-
In assessing the pain of an advanced cancer patient, the nurse should:
- Get a description of the pain from the patient - most cancer patients will have more than one type of pain.
- Assess each pain individually, and identifying the mostly likely cause of the pain (if possible).
-
Ask the patient about:
- the site and radiation of the pain
- the character of the pain
- the severity and intensity of the pain
- the timing and duration of the pain
- whether there are any exacerbating factors
- what the patient feels are the relieving factors (e.g. medication)
- the effect of the pain on the patient’s function, sleep, and mood
- what response the patient has had to previous medication and treatment.
- Use an approved structured pain assessment tool to record the patient’s pain – e.g. the visual analogue scale.
- In addition, any psychological, social, and/or spiritual factors affecting or impacting upon the patient’s pain should be considered as part of the assessment.
Management of cancer pain
- Left untreated, pain from advanced cancer is distressing, and has numerous associations with poor patient outcomes.
- Adequate holistic pain and symptom management is an essential component of palliative and end-of-life care.
- Within palliative care, drug therapy is an incredibly important tool to manage pain in the patient with advanced cancer.
- The World Health Organization (WHO) pain ladder is the most commonly used treatment pathway for pain; many of the principles of pain management are based on this ladder.
- The severity of the pain experienced by the patient will determine the strength of analgesic required, and the type and cause of the pain will influence the choice of adjuvant analgesic used, if required.
The WHO pain ladder
- Step 1 – Non-opioid medication ± an adjuvant (e.g. paracetamol, NSAID)
- Step 2 – Opioids for mild to moderate pain, ± non-opioid medication, ± adjuvant (e.g. codeine, dihydrocodeine, NSAID)
- Step 3 – Opioids for moderate to severe pain, ± non-opioid, ± adjuvant (e.g. morphine, oxycodone, ± paracetamol, ± NSAID) (Figure 1, and Table 1).
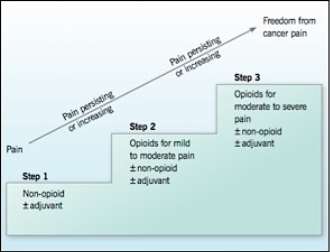
Fig 1. WHO pain ladder (reproduced with permission from Hughes, 2012, p.26).
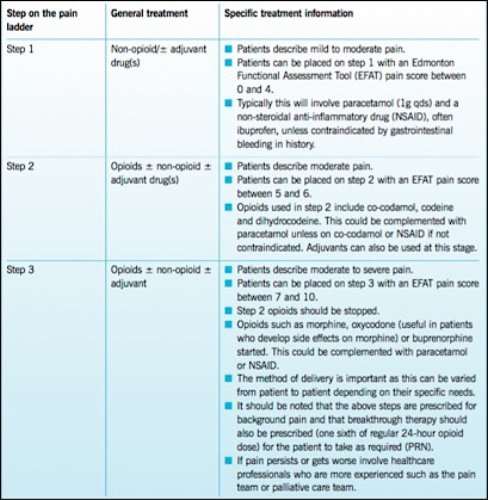
Table 1. WHO pain ladder (reproduced with permission from Hughes, 2012, p.27).
Choosing an appropriate opioid medication for a patient on Step 3 of the WHO pain ladder
First-line opioids
-
Morphine
- There is a range of oral preparations available; subcutaneous (SC) injection, and via a syringe pump.
- Morphine is renally excreted, as such it must be titrated slowly and monitored carefully in patients with stage 1 to 3 chronic kidney disease (CKD).
- Consider other opioids in stage 4 to 5 CKD, and dialysis patients.
- Consider low doses and slow titration in liver impairment.
-
Diamorphine
- Highly soluble opioid used for SC injection and in a syringe pump.
- Use for high-dose SC breakthrough injections (above 180mg SC morphine/24 hours). Powder preparation is diluted in a small volume of water for injections.
- As with morphine, cautious use in renal and liver impairment.
Second-line opioids
-
Oxycodone
- Indicated in moderate to severe pain where morphine/diamorphine are not tolerated.
- Immediate and modified release oral preparations; SC injection; syringe pump.
- Lower concentration preparation limits dose for SC injection to 20mg (2ml).
- Avoid use in patients with moderate to severe liver impairment – clearance of oxycodone is greatly reduced.
- Reduced clearance is also seen in mild/moderate renal impairment; must be titrated slowly and monitored carefully. Avoid use in patients with stage 4–5 CKD.
-
Fentanyl
- Administered via a 72hr transdermal patch; to be considered for use if oral and SC routes for analgesia are not suitable.
- For stable pain, as the dose cannot be changed quickly.
- No initial dose reduction in renal impairment but may accumulate over time.
- Dose reduction may be needed in severe liver disease.
Third-line opioids (requires specialist advice)
-
Alfentanil
- Alfentanil is a short-acting, injectable opioid for SC injection and in a syringe pump.
- In episodic pain, alfentanil can be given subcutaneously.
- The dose does not need to be reduced in renal disease (including stage 4–5 CKD)
- Clearance may be reduced in liver impairment; requires a reduced dose with careful titration.
-
Fentanyl sublingual/intranasal
- In episodic/incident pain, fentanyl can be given sublingually or intra-nasally.
Fourth-line opioid (specialist use only)
-
Methadone
- Oral methadone is used by specialists for complex pain; dosing is difficult due to the long half-life.
- Methadone is not excreted renally, so no dose reduction is required in CKD.
- The half-life of methadone is prolonged in severe liver disease.
Opioid toxicity
- There is a wide variation in the dose of opioid that causes symptoms of toxicity.
-
Rapid recognition and treatment of opioid toxicity are needed. Symptoms of toxicity include:
- Persistent sedation
- Vivid dreams and/or hallucinations; shadows at the edge of visual field
- Delirium
- Muscle twitching/myoclonus/jerking
- Abnormal skin sensitivity to touch.
-
Management of opioid toxicity:
- Reduce the dose of the opioid by one-third, if pain is suitably controlled. Ensure the patient is well hydrated. Seek specialist advice.
- Consider adjuvant analgesics, alternative opioids, or both if the patient remains in pain.
Table 2. Example nursing care plan for the patient with acute/chronic pain due to advanced cancer
Problem |
Identification |
Goal |
Intervention/s |
Rationale |
|
Patient is experiencing acute/chronic pain, which may be related to:
|
Autonomic responses
|
|
|
|
Sources and recommended reading
Cancer Research UK, (2016). Cancer statistics for the UK [Internet]. Available at: http://www.cancerresearchuk.org/health-professional/cancer-statistics [Accessed 15 January 2017].
Deandrea, S., Montanari, M., Moja, L., et al., (2008). Prevalence of undertreatment in cancer pain. A review of the published literature. Annals of Oncology, 19(2), 1985-1991.
Doenges, M. E., Moorhouse, M. F., Murr, A. C., (2010). Nursing care plans: Guidelines for individualizing client care across the life span 8th Ed. Philadelphia: F. A. Davis Company.
Dubenkse, L. L., Mayer, D., Gustafson, D. H., (2016). Advanced cancer: Palliative, End of Life, and Bereavement Care. In: Hesse, B. W., Ahern, D., Beckjord, E., (2016). Oncology Informatics: Using health information technology to improve processes and outcomes in cancer. London: Elsevier.
Hughes, L., (2012). Assessment and management of pain in older adults receiving palliative care. Nursing Older People, 24(6), 23-29.
Joshi, M., Chambers, W. A., (2010). Pain relief in palliative care: a focus on interventional pain management. Expert Reviews in Neurotherapeutics, 10(5), 747-756.
NHS Scotland, (2014). Scottish Palliative Care Guidelines [Internet]. Available at: http://www.palliativecareguidelines.scot.nhs.uk [Accessed 15 January 2017].
Nursing and Midwifery Council, (2015). The Code: Professional standards of practice and behaviour for nurses and midwives [Online]. Available at: https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf [Accessed 15 January 2017].
Porter, L. S., Keefe, F. J., (2011). Psychosocial issues in cancer pain. Current Pain and Headache Reports, 15(4), 263-270.
Wilkie, D. J., Ezenwa, M. O., (2012). Pain and symptom management in palliative care and at end of life. Nursing Outlook, 60(6), 357-364.
Cite This Work
To export a reference to this article please select a referencing stye below: