Introduction
As with the cardiovascular system, which you studied in the previous chapter of this module, the respiratory system is one of the body's fundamental life-sustaining systems; therefore, it is essential that nurses are able to accurately and comprehensively assess this system. This chapter introduces the fundamental knowledge and skills nurses require to do so. It begins with an overview of the fundamental anatomy and physiology of the respiratory system. The chapter then explains the processes involved in collecting a general health history for the respiratory system, and in performing a physical examination of the respiratory system. Finally, this chapter considers a number of special observation and assessment techniques which may be used in the physical examination of the respiratory system, and about performing differential diagnosis relevant to the respiratory system.
Learning objectives for this chapter
By the end of this chapter, we would like you:
- To describe the basic anatomy and physiology of the respiratory system.
- To explain how to collect a focused health history related to the respiratory system.
- To describe how to assess dyspnoea, a key symptom of respiratory dysfunction.
- To identify smoking as a key cause of respiratory disease in the United Kingdom (UK), and to explain how nurses should respond to a patient who smokes.
- To explain how to undertake a physical examination of the respiratory system.
- To discuss the age-related differences to be considered when assessing the respiratory system.
- To understand how to auscultate a patient's anterior and posterior thorax in a systematic way. -To list abnormalities which may be identified in a patient's breathing pattern and breath sounds.
- To explain how to document respiratory system assessment findings.
- To recognise the common respiratory problems / conditions, and their typical clinical findings, to enable differential diagnosis
- To describe the variety of special assessment techniques which may be used in the physical examination of the respiratory system.
Important note
This section of the chapter assumes a basic knowledge of human anatomy and physiology. If you feel you need to revise these concepts, you are encouraged to consult a quality nursing textbook.
If you need assistance with writing your essay, our professional nursing essay writing service is here to help!
Find out moreFundamental anatomy and physiology of the respiratory system
The respiratory system consists of the lungs, airways and associated structures. It has two key roles: (1) to supply oxygen to the body's cells, and (2) to remove carbon dioxide and other gaseous waste products from the body's cells. It does this via processes including: (1) ventilation (the movement of gases into and out of the lungs, by inspiration and expiration), and (2) diffusion (the movement of gasses over the respiratory membrane, from an area of high concentration to an area of low concentration).
The main organs of the respiratory system are the lungs. The right lung has three lobes, and the left lung has two lobes (to make room for the heart). It is important for nurses to bear in mind that the lungs are very large organs; indeed, each lung extends anteriorly about 4 centimetres above the top rib, and on deep inspiration they may expand down to about the twelfth thoracic vertebrae (T12).
The lungs are surrounded by tissue called pleura, which is well-lubricated to prevent friction during inspiration and expiration. The lungs sit within the thorax, a bony cage consisting of the 12 thoracic vertebrae, 12 pairs of ribs and the sternum ('breastbone'). The thorax acts to protect the respiratory structures (and the heart), and also helps to facilitate breathing.
Breathing is controlled by the diaphragm (a band of muscle at the base of the lungs) and the intercostal muscles (those around the ribs). During inspiration ('breathing in'), the diaphragm contracts downwards, while the intercostal muscles pull the chest wall outwards. This creates a negative pressure in the lungs (when compared with the pressure outside the lungs), resulting in the lungs filling with air. During expiration ('breathing out'), the diaphragm and intercostal muscles relax and air is expelled from the lungs.
During inspiration, air travels into the lungs via the airways. The upper airways include structures such as the mouth / nose, the pharynx, the larynx and the upper trachea, a flexible tube which, in adults, is approximately 10 centimetres long. These upper airway structures have three key roles: (1) to assist with the movement of air into the lower airways, (2) to protect the lower airway from foreign matter which may be inhaled, and (3) to warm, filter and humidify inspired air. The lower airways consist of structures including the lower trachea, the bronchi, the bronchioles and the alveoli. Essentially, the lower airways are branching tubes which become progressively smaller, until they terminate in the alveoli, a series of balloon-like structures. It is at the level of the alveoli that gas exchange - essentially, oxygen in and carbon dioxide out - occurs.
Respiratory system - focused health history
As you have seen in previous chapters of this module, health observation and assessment involves three concurrent steps:
When assessing a patient's respiratory system, the nurse must commence by collecting a health history. This involves collecting data about:
|
Component |
Rationale |
|
Present health status |
Chronic illnesses, even if they are not related directly to dysfunction in the respiratory system, can cause damage to this system (e.g. renal disease may result in pulmonary oedema). Allergies, particularly those which affect the respiratory system (e.g. which result in a runny nose, nasal congestion, cough, wheeze, dyspnoea, etc.). Shortness of breath, because this is a key symptom of dysfunction in the respiratory (and / or the cardiovascular) systems. Nurses should assess shortness of breath: (1) when the patient is completing activities of daily living, and (2) when the patient is sleeping. Medications, including those aimed at managing respiratory dysfunction (e.g. inhalers, oxygen, etc.), including details such as dose, frequency and effect, etc. Tobacco smoking (past and current), as this is a leading cause of respiratory disease in the UK. Nurses should assess:
|
|
Past medical history |
Previous respiratory diseases, including asthma, bronchitis, bronchiectasis, emphysema, cystic fibrosis, lung cancer, tuberculosis, pneumonia and chronic obstructive pulmonary disease. This can give a nurse important information about how to structure their physical examination. Injuries and / or surgeries to the chest, as these can affect the function of the lungs and associated structures. |
|
Family history |
Family history of respiratory conditions, especially among first-degree relatives, as this can provide important information about the types of heart disease for which a person may have a congenital risk. |
|
Living and occupational environments |
Environmental conditions - including exposure to air pollution (e.g. living near a factory, on a busy street, in a new construction area, etc.), allergens (e.g. pets), certain heating / air-conditioning / ventilation systems, toxins associated with chemical plants / mines, some substances such as asbestos, and vapours / fumes - can impact significantly on a person's respiratory health. |
|
Recent international travel |
Recent international travel - this information can help a nurse to determine whether a patient may have been exposed to a serious respiratory disease, such as Sudden Acute Respiratory Syndrome (SARS) or pandemic influenzas which are known to be present in some parts the world (e.g. in regions of Asia). |
In some cases, a person will present with a specific problem related to their respiratory system (e.g. cough,
dyspnoea, chest pain on inspiration / expiration, etc.). Remember, nurses assess a patient's symptoms using the
strategy remembered by the 'OLD CARTS' mnemonic (introduced in a previous chapter of this module).
Dyspnoea - or 'shortness of breath' - is a particularly common symptom associated with the respiratory
symptom. It may be due to a variety of causes - including those which impair pulmonary ventilation, circulation
and / or gas exchange. For example:
- Obstructed ventilation (e.g. asthma, lower airway inflammation, etc.).
- Restricted ventilation (e.g. muscle weakness due to neuromuscular disease, reduced pulmonary compliance due to pulmonary fibrosis, compression / replacement of the lung tissue, reduced elasticity of the lung tissue, etc.).
- Reduced perfusion (e.g. due to pulmonary embolism / hypertension, cardiac failure, etc.).
- Interstitial disease (e.g. pulmonary fibrosis, pneumonitis, oedema, emphysema, etc.).
During assessment, dyspnoea is measured by recording a person's respiratory rate (as described in detail in an earlier chapter of this module). Dyspnoea can also be assessed in other ways; for example, when taking the health history, a nurse may assess the number of words a person can say before needing to pause to take a breath. A healthy adult can say between 10 and 14 words before taking a breath, however a person with severe dyspnoea may only be able to take 3 or 4 words.
When assessing a patient with dyspnoea, it is important for nurses to remember that this is a very distressing symptom, and one which (if sufficiently severe) may place the person's life at immediate risk. If a nurse identifies that a patient is severely dyspnoeic, the assessment should cease while this symptom is addressed.
As you collect a general health history from a patient, it is important that you assess and identify risk factors for respiratory disease. As noted in a previous section of this chapter, tobacco smoking is a leading cause of respiratory disease in the UK. Importantly, this is a modifiable risk factor - that is, one in relation to which a person is capable of making changes to reduce their risk. As part of their fundamental health promotion role, it is important that nurses are able to provide patients with advice about how to address the respiratory disease risk factors identified during assessment.
Activity
You are encouraged to explore the information on the National Health Service's (NHS) Smokefree website. This website can be accessed online, by searching for its title.
Respiratory system - physical examination
Once a respiratory health history has been obtained, as described in the previous section of this chapter, a nurse may commence a physical examination of the patient's respiratory system. A stepwise process of physically examining the patient's respiratory system, with normal (expected) and common abnormal findings, is presented in the following table:
|
Component |
Normal (Expected) Findings |
Abnormal Findings |
|
Inspect the patient for general appearance, posture, breathing effort, etc. |
The patient should be relaxed, upright, and breathing effortlessly at a rate appropriate for their age. |
Apprehension; restlessness; nasal flaring; retractions (e.g. of the tissues into the supraclavicular or intercostal spaces); use of accessory muscles; asymmetrical (or 'paradoxical) movement of the chest wall; tripod positioning (leaning forward with the arms braced against the knees), etc. |
|
Observe the respirations for rate, quality, pattern and chest expansion. |
The person should breathe at a rate of 10 to 16 breaths per minute; breathing should be smooth, with an even depth (though some variation, particularly when taking, is normal). |
Abnormal breathing patterns (refer to the description later in this section of the chapter). |
|
Inspect the patient's nails, skin and lips for colour. |
The colour observed should be consistent with the skin colour for the individual. |
Cyanosis or pallor of the nails, skin or lips (this is a key indicator of hypoxia). |
|
Measure the oxygen saturation (SpO2). |
SpO2 is within the normal range of 98-100%. |
SpO2 is <98%. |
|
Inspect the anterior and posterior thorax for shape and symmetry. |
The thorax should be symmetric; the ribs slope downwards at 45 to the spine; the bony structures (e.g. spine, scapulae) should be straight and symmetric. |
Asymmetry; skeletal deformities (particularly those which limit the expansion of the chest); deformities of the anterior thorax (e.g. pectus carinatum, pectus excavatum). |
|
Auscultate the anterior and posterior thorax (as described in greater detail in a following section of this chapter), and the lateral thorax. |
Breath sounds should be high-pitched and clear. |
Adventitious (added or unexpected) sounds (refer to the description later in this section of the chapter); diminished breath sounds. |
|
Palpate the anterior and posterior thorax for tenderness, bulges, symmetry, fremitus, etc. |
The rib cage should be symmetric and firm; there should be no tenderness or bulges; fremitus is palpable, etc. |
Tenderness; bulges; crepitus; absent or enhanced fremitus, etc. |
|
Percuss the anterior, posterior and lateral thorax for tone (using the techniques described following). |
The sound should be resonant (i.e. loud in intensity, low in pitch, long in duration, hollow in quality). |
Hyperresoance (i.e. very low resonance, indicating over-inflation of the lungs); dull tones. |
|
Palpate the trachea for position. |
The trachea should be palpable, midline and slightly moveable. |
The trachea is not midline (e.g. due to a mass, mediastinal shift, pneumothorax, etc.). |
When physically assessing a client's respiratory system, it is important for a nurse to note that there are a number of important age-related differences. You will study age-related differences in assessment in detail in a later chapter of this module; however, for now, consider these age-related differences specific to the assessment of the respiratory system:
- The respiratory assessment of an infant or a young child who is crying is very difficult, and is likely to produce inaccurate data. It is important that young children are calm before a respiratory assessment is commenced. Developing rapport with the child can assist with this; again, this will be explored in greater detail in a later chapter of this module.
- When undertaking a respiratory assessment with an older adult, it is important for nurses to be aware that age-related structural problems - including stooping and kyphosis, etc. - may make the expansion of the thorax more difficult, and lead to respiratory problems.
|
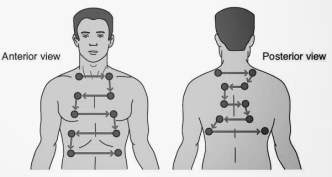
As you saw in the above table, assessing a patient's respirations and respiratory effort is a key part of the physical examination of the respiratory system. When auscultating a patient's chest, it is essential that a nurse uses a systematic process to ensure that all areas of the chest are heard. One strategy is illustrated here, in relation to both the anterior and the posterior chest: |
|
When auscultating the chest, a nurse may identify a number of abnormalities in the patient's breathing pattern or rhythm. Read the information in the following table:
|
Abnormality |
Description |
|
Bradypnoea |
A respiratory rate of <10 breaths per minute; the respiratory rhythm and depth remain smooth and even. |
|
Tachypnoea |
A respiratory rate of >16 breaths per minute; the respiratory rhythm and depth remain smooth and even. |
|
Hyperventilation |
A very rapid respiratory rate; the respiratory rhythm and depth are increased. When hyperventilation occurs due to ketoacidosis, and is very deep and laborious, it is termed Kussmaul breathing. |
|
Biot |
Breathing characterised by intermittent periods of apnoea (no breathing), with a disorganised pattern, rate and depth. |
|
Cheyne stokes |
Intervals of apnoea interspersed with deep, rapid breathing. This is seen in severely ill patients, often those who are nearing death. |
|
Air trapping |
Breathing characterised by rapid inspirations with prolonged, forced expirations where the air in the lungs is not fully exhaled. This is most often seen in patients with chronic obstructive pulmonary disease and similar conditions. |
When auscultating the chest, a nurse may identify a number of abnormalities in the patient's breath sounds. Read the information in the following table:
|
Abnormality |
Description |
|
Stridor |
A harsh, high-pitched sound, often associated with inflammation or obstruction in the laryngeal or tracheal regions. |
|
Fine crackles |
A fine, high-pitched crackling / popping noise, usually heard at the end of inspiration. It cannot be cleared by coughing. It is often evident in mild pneumonia, heart failure, asthma and restrictive pulmonary disease. |
|
Medium crackles |
A moist, medium-pitched sound, usually heard midway through inspiration. It cannot be cleared by coughing. It is often evident in more severe pneumonia, heart failure, asthma and restrictive pulmonary disease. |
|
Coarse crackles |
A low-pitched bubbling / gurgling sound, usually heart at the beginning of inspiration. It cannot be cleared by coughing. It is often evident in very severe pneumonia, heart failure, asthma and restrictive pulmonary disease. It may also be heard in pulmonary oedema and pulmonary fibrosis. |
|
Wheeze |
A high-pitched, squeaking sound which may occur on inspiration and / or expiration. Often heard in diseases which result in narrowing of the airways, such as asthma. |
|
Rhonchi |
A low-pitched, coarse, loud 'snoring' or 'moaning' noise, which occurs primarily during inspiration. It may be cleared by coughing. Caused in disorders which result in obstruction of the trachea or bronchi, such as chronic bronchitis. |
|
Pleural friction rub |
A low-pitched, coarse rubbing or grating sound, heard continuously throughout inspiration and expiration. It cannot be cleared by coughing. It is heard in diseases which result in inflammation of the pleural surfaces (e.g. pleurisy). |
Abnormal breath sounds are divided into two categories:
- Adventitious sounds, as described in the above table, are those which are added / unexpected.
- Diminished sounds, where the breath sounds are hard to hear or are even absent. This is common in patients whose alveoli are collapsed / have been destroyed, where there is atelectasis or in a severe asthma attack, etc.
It is important for nurses to remember that a number of errors in auscultation may result in adventitious sounds, including:
- The stethoscope (either the diaphragm / bell or the tubing) is bumped or touched.
- The client is shivering because they are cold, feverish or afraid, etc.
- The stethoscope rubs against the client's skin or hair.
- There are extraneous environmental noises (e.g. rustling of a gown or curtain, etc.).
If a nurse identifies a possible adventitious sound, they should check to confirm that none of these errors are occurring, ask the patient to cough, reposition the stethoscope and listen again. If the adventitious sound is heard again, the nurse can be confident that they are hearing it correctly.
As you saw in a previous section of this unit, once a health history and physical examination have been completed, they should be documented so that the data collected can be used to: (1) assess the patient's condition, and (2) inform the care which is appropriate for that patient. Review the following example of how the findings from a physical examination of the respiratory system are documented (in this case, all the assessment findings are normal):
Example
15/11/2016 - NURSING ASSESSMENT: Mrs Zhou's breathing is quiet and effortless, as a rate of 14 breaths per minute. There is no pallor or cyanosis evident in the skin, nails or lips. Thorax is symmetric, with the ribs sloping downward at approximately 45° relative to the spine. Thoracic expansion is symmetric bilaterally. The trachea is midline. Breath sounds are clear in all lung fields. J SMITH (RN) _________________________________________
Special assessment techniques for the respiratory system
There are a number of special assessment techniques particular to the respiratory system:
- Palpating the posterior chest wall for thoracic expansion. Palpation involves a nurse using their hands to feel the texture, size, shape, consistency and pulsations, etc., of different parts of a patient's body. The nurse should stand behind the patient, and place their thumbs on either side of the client's spine (at about the level of the T9 / T10 vertebrae). The fingers of each hand should be extended outwards across the patient's posterior chest wall. The patient should be instructed to take a number of deep breaths. The lateral movement of the thumbs as the client breathes in should be equal. Unequal movement is indicative of a number of problems with the respiratory system - including injury to the ribs and / or chest wall, pneumonia and atelectasis - and further investigation is required.
Note: this assessment technique may also be performed on the anterior chest.
- Percussion, including of the posterior and lateral thorax. This involves a nurse striking a finger directly against the client's chest wall, and listening to the sound that is created. Nurses should percuss a patient's thorax using the same reverse-Z pattern used when auscultating the thorax, as described earlier in this chapter.
- Palpating the posterior thorax. When using palpation as a technique to assess the respiratory system at the level of the thorax, a nurse usually asks a patient to verbalise (e.g. reciting 'one-two-three' or 'ninety-nine'), and assesses for vibrations occurring in the chest wall. Vibrations which result from verbalisations are referred to as fremitus, and these are a normal assessment finding. Decreased or absent fremitus is often seen in patients who have emphysema, pleural effusion, pulmonary oedema or bronchial obstruction. Enhanced fremitus is often seen in patients whose lungs are congested or consolidated (e.g. due to pneumonia, a tumour, etc.).
Differential diagnosis in the respiratory system
When assessing a patient's respiratory system, there are a number of common problems and conditions a nurse may identify. Consider the conditions and their key clinical findings, outlined in the following table. This information can be useful in assisting a nurse to make a differential diagnosis of a respiratory condition:
|
Respiratory Problem or Condition |
Typical Clinical Findings |
|
Acute bronchitis - an inflammation of the mucous membranes of the bronchi, often due to infection. |
Cough (initially non-productive, then productive); substernal chest pain (often aggravated by coughing); fever; malaise; tachypnoea; rhonchi (often on auscultation); wheezing (often during / after coughing). |
|
Pneumonia - an infection of the terminal bronchioles and / or alveoli, which may be bacterial, viral or fungal in origin. |
In viral pneumonia, a non-productive cough (e.g. clear sputum); in bacterial / fungal pneumonia, a productive cough (e.g. white, yellow or green sputum); fever; malaise; pleuritic chest pain; pulmonary consolidation (e.g. crackles, increased fremitus, etc.). |
|
Tuberculosis - an infection of the lung tissue (and, possibly, other body tissue) with the bacteria Mycobacterium tuberculosis. |
The early stages of the disease may be asymptomatic. Progresses to frequent, productive cough; fatigue; anorexia; weight loss; night sweats; fever. |
|
Pleural effusion - an accumulation of serous fluid in the pleural space. |
The manifestation depends on the amount of fluid accumulated. In severe cases, there is dyspnoea; intercostal bulging; decreased chest wall movement. |
|
Asthma - a disease characterised by bronchoconstriction, inflammation and airway obstruction in response to the inhalation of allergens or irritants. |
Increased respiratory rate with prolonged expiration; severe dyspnoea; audible wheeze (especially on expiration); tachycardia; anxiety; accessory muscle use; cough; diminished breath sounds. |
|
Emphysema - a disease which results from the destruction of the alveoli, and the massive enlargement of the terminal air spaces. |
Unwell general appearance (e.g. underweight, barrel chest); dyspnoea on minimal exertion; pursed-lip breathing; tripod positioning; diminished breath sounds; wheezing and crackles (particularly on auscultation). |
|
Chronic bronchitis - a disease characterised by hypersecretion of mucous in the trachea and bronchi. |
Productive cough; increased mucous production; dyspnoea; rhonchi (sometimes cleared by coughing); crackles (when mucous is present in the alveoli). |
|
Pneumothorax - where there is air in the pleural space, and one or both lungs 'collapses' or deflates (either spontaneously, or as a result of trauma). |
The manifestation depends on the extent of the lung collapse. Dyspnoea; anxiety; chest pain; tachypnoea; cyanosis; hyperresonant breath sounds (on the side affected); decreased chest wall movement (on the side affected); tracheal displacement, etc. |
|
Haemothorax - where there is blood in the pleural space, and one or both lungs 'collapses' or deflates. |
The manifestation depends on the extent of the lung collapse. Dyspnoea; anxiety; chest pain; tachypnoea; cyanosis; muffled breath sounds (on the side affected); decreased chest wall movement (on the side affected); tracheal displacement; dullness with percussion (on the side affected), etc. |
|
Atelectasis - this is a condition involving the collapse of the alveoli (e.g. due to a tumour, fluid or air in the pleural space, secretions in the alveoli, etc.). |
Diminished or absent breath sounds; decreased oxygen saturation. |
|
Lung cancer - the uncontrolled growth of cells (i.e. a 'cancer') in the lung tissue. |
Persistent cough; weight loss; congestion; wheezing; haemoptysis; dyspnoea; diminished breath sounds (on the side affected); wheezes (if a tumour obstructs the airways); dullness with percussion (over the tumour site/s), etc. |
If you need assistance with writing your essay, our professional nursing essay writing service is here to help!
Find out moreConclusion
As you have seen throughout this chapter, it is essential that nurses are able to accurately and comprehensively assess the respiratory system. This chapter has introduced the fundamental knowledge and skills nurses require to do so. It began with an overview of the fundamental anatomy and physiology of the respiratory system. The chapter then explained the processes involved in collecting a general health history for the respiratory system, and in performing a physical examination of the respiratory system. Finally, this chapter considered a number of special observation and assessment techniques which may be used in the physical examination of the respiratory system.
Reflection
Now we have reached the end of this chapter, you should be able:
- To describe the basic anatomy and physiology of the respiratory system.
- To explain how to collect a focused health history related to the respiratory system.
- To describe how to assess dyspnoea, a key symptom of respiratory dysfunction.
- To identify smoking as a key cause of respiratory disease in the United Kingdom (UK), and to explain how nurses should respond to a patient who smokes.
- To explain how to undertake a physical examination of the respiratory system.
- To discuss the age-related differences to be considered when assessing the respiratory system.
- To understand how to auscultate a patient's anterior and posterior thorax in a systematic way.
- To list abnormalities which may be identified in a patient's breathing pattern and breath sounds.
- To explain how to document respiratory system assessment findings.
- To recognise the common respiratory problems / conditions, and their typical clinical findings, to enable differential diagnosis
- To describe the variety of special assessment techniques which may be used in the physical examination of the respiratory system.
Reference list
Cox, C. (2009). Physical Assessment for Nurses (2nd edn.). West Sussex, UK: Blackwell Publishing, Ltd.
Howard, P.K. & Steinmann, R.A. (Eds.). (2010). Sheehy's Emergency Nursing: Principles and Practice. Naperville, IL: Mosby Elsevier.
Jensen, S. (2014). Nursing Health Assessment: A Best Practice Approach. London, UK: Wolters Kluwer Publishing.
National Health Service. (2016). Smokefree. Retrieved from: https://quitnow.smokefree.nhs.uk/
Wilson, S.F. & Giddens, J.F. (2005). Health Assessment for Nursing Practice (4th edn.). St Louis, MI: Mosby Elsevier.
Cite This Work
To export a reference to this article please select a referencing style below: