Introduction
Health observation and assessment is a systematic process undertaken to collect data about a patient. This data provides nurses and other health care professionals with information about the patient's condition, and it is used to inform the care which is appropriate for that patient and to evaluate the effectiveness of that care. Nurses undertake health observation and assessment constantly, in all clinical settings; therefore, it is essential that nurses are able to complete an accurate, comprehensive and systematic health observation and assessment of a variety of different patients.
This chapter provides a broad introduction to health observation and assessment. It begins with an overview of health observation and assessment - describing its place in the nursing care cycle, the key steps involved, the application of clinical judgement to understand data collected, and the different approaches which may be used. This chapter goes on to describe the process involved in conducting a head-to-toe assessment, including a primary and secondary survey, to collect data from a patient in an accurate, comprehensive and systematic way. Finally, this chapter describes the correct documentation, or recording, of data collected during health observation and assessment. In completing this chapter, you will begin developing the knowledge and skills necessary to conduct a health observation and assessment in your nursing practice.
Learning objectives for this chapter
By the end of this chapter, we would like you:
-To explain the place of health observation and assessment in the nursing care cycle.
-To list and describe the three key steps involved in health observation and assessment.
-To explain the difference between signs (objective) and symptoms (subjective).
-To describe the application of clinical judgement to understand assessment data.
-To discuss cultural considerations related to health observation and assessment.
-To describe the processes involved in conducting a systematic head-to-toe assessment of a patient, including completing a primary survey and a secondary survey.
-To be able to accurately document health observation and assessment findings.
If you need assistance with writing your essay, our professional nursing essay writing service is here to help!
Find out moreHealth observation and assessment in nursing practice
|
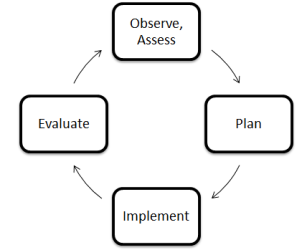
As stated in the introduction to this chapter, health observation and assessment is a systematic process to collect data about a patient. This data provides nurses and other health care professionals with information about the patient's condition, and it is used to inform the care which is appropriate for that patient. Nurses undertake health observation and assessment constantly, in all clinical settings. Health observation and assessment is the first step in the nursing care cycle, illustrated in the diagram to the right: |
|
Health assessment involves three concurrent steps:
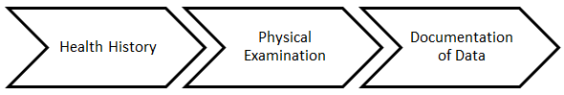
- Health History: this involves collecting subjective data - that is, data about a patient's symptoms (i.e. what the patient experiences). Data is collected via an interview with the patient and / or significant others. Data collected at this stage may be primary (i.e. obtained from the patient themselves) or secondary (i.e. obtained from another person, such as the patient's family member or carer, etc.).
- Physical Examination: this involves collecting objective data - that is, data about a patient's signs (i.e. what the nurse can observe, feel, hear or measure). Data is collected via a physical examination of the patient, using techniques such as inspection, palpation, percussion and auscultation, and measurement of the vital signs and other key physical indicators. You will study these and a variety of other physical examination skills in detail throughout later chapters in this module.
It is important for nurses to understand the difference between symptoms and signs. Remember: symptoms are what the patient subjectively experiences - for example, pain, itching, nausea, etc. Signs are what a nurse objectively observes, feels, hears or measures - for example, a rash, enlarged lymph nodes, tachycardia, etc. In some cases, data collected during health observation and assessment may be both a symptom and a sign. For example, a client may tell a nurse that she "feels sweaty" (a symptom), while at the same time a nurse observes diaphoresis (a sign).
- Documentation of Data: data collected during health observation and assessment must be documented so that it can be used to: (1) assess the patient's condition, and (2) inform the care which is appropriate for that patient (and also enable the evaluation of that care). There are a variety of ways that data can be recorded, and this generally differs between clinical settings and organisations; nurses are encouraged to familiarise themselves with the documentation strategies used in the organisation where they work. Regardless of how data is recorded, however, documentation must be complete, accurate, concise, legible and free from bias.
Once data is collected and documented, it must be used. This involves the application of clinical judgement to understand the data - specifically, a nurse should recognise normal versus abnormal data, seek to interpret that data (i.e. to determine what it means), and to use the data to identify the client's health problems and needs. The nurse then applies this understanding to make decisions about the care provided to a patient.
It is important to note that there are a number of different types of health assessment which a nurse may undertake:
- Comprehensive health assessment: this involves taking a detailed health history and physical examination of a client, with the aim of identifying all of the person's health care issues and needs. It is usually performed on admission to a care setting.
- Problem-based / focused health assessment: this involves collecting data related to a specific complaint. This type of assessment is common in outpatient settings.
- Rapid assessment: this involves collecting data required to provide immediate, life-sustaining intervention to a patient. It is often performed in emergency care settings.
- Episodic / follow-up assessment: this involves a nurse following up with a patient to collect data on a previously-identified problem. The goal is to determine how the patient has responded to care implemented to treat the problem, by identifying changes in the patient's condition from baseline.
- Screening assessment: this involves collecting data with the aim of detecting the presence of a specific disease affecting a patient. Common examples include blood glucose screening, blood pressure screening and blood cholesterol screening, etc.
The type of assessment used by a nurse depends on: (1) the context in which the nurse is working, and (2) the health care issues and needs of the patient being assessed. For example, if a nurse is working in an acute care setting where they are initiating care for a new client, a comprehensive health assessment is usually appropriate. However, if a nurse is working in an emergency care setting where a patient presents with a clear, significant problem, a comprehensive health assessment is not indicated and a rapid assessment is typically more suitable. This module will focus on teaching the knowledge and skills required to perform a comprehensive health assessment, as it is these knowledge and skills which underpin all other types of health assessment.
Cultural considerations in health observation and assessment
A person's culture is far more than simply their ethnic background; rather, it is about how they live in and perceive the world around them. People who share a culture also share values, beliefs and attitudes about various topics - including about their health. It is important for nurses working in the United Kingdom (UK) to remember that ours is a highly diverse society. Nurses will care for people of a diverse range of genders and sexual orientations, ages, ethnicities, religious beliefs, abilities and socioeconomic statuses, etc. In particular, nurses are challenged with the responsibility of providing effective care to people whose health practices, values, beliefs and attitudes may differ significantly from their own. Consider the following case study example:
Example
Claire is a graduate nurse working in a community clinic in London. One of her patients is Awet, an elderly woman from Eritrea, who is accompanied by her granddaughter. During the health history, the granddaughter tells Claire that Awet has been experiencing a frequent urge to urinate, pain on urination and fever. During the physical examination, Claire obtains a sample of Awet's urine, and when she tests this using a dipstick she finds blood and leucocytes. These are all classic symptoms and signs of a urinary tract infection.
"I think you may have a urinary tract infection," Claire tells Awet - but Awet shakes her head emphatically.
"She thinks her illness is because she didn't perform Meskel rituals this year, and God is upset," the granddaughter explains to Claire.
It is important that nurses are respectful of the diverse health practices, values, beliefs and attitudes they will encounter in practice. This involves, in part, becoming a culturally competent nurse - that is, one who is able to engage effectively with people from a variety of different cultural backgrounds. To be culturally competent, a nurse must recognise that differences do exist between people, but that we are all fundamentally striving for the same goal - wellbeing, however we may define that term. Consider the following example of culturally competent practice:
Example
Lucas is a graduate nurse working in an emergency care unit of a large metropolitan hospital. One of his patients is a local man named David. Lucas observes that David has a bandage on his arm, with green fluid seeping through. At the beginning of his health history, Lucas asks David about it.
"It's a herbal poultice to help heal a boil," David tells Lucas.
There are a number of ways Lucas could respond to this statement. He could advise David that herbal therapies are not evidence-based, and that poultices may increase the risk of infection. He could also advise that the boil would be more likely to heal if David were to wash off the poultice and apply an antibiotic cream. Instead, as a culturally competent practitioner, Lucas asks David what the boil looks and feels like, and whether the herbal poultice is helping it to get better.
"Yes," David says, "by the day after I put the poultice on, the infection had nearly gone."
Nurses are not expected to know all the health practices, values, beliefs and attitudes of all the different cultural groups they work with - indeed, this would be impossible as there is significant diversity both between and within different cultural groups. It is important that nurses avoid stereotyping the people with whom they work - that is, assuming that they follow certain health practices, values, beliefs and attitudes simply because they identify as belonging to a particular cultural group. Rather, nurses must recognise each person as an individual. During health observation and assessment, nurses are encouraged to ask questions to understand each individual patient's health practices, values, beliefs and attitudes.
Conducting a systematic head-to-toe assessment and primary / secondary survey
Important note
This section of the chapter assumes a basic knowledge of human anatomy and physiology. If you feel you need to revise these concepts, you are encouraged to consult a quality nursing textbook.
The following chapters of this module will describe the assessment of each of the major body systems in detail. However, this chapter introduces the idea of a 'head-to-toe assessment', an approach to physical examination which enables a nurse to assess a client systematically and comprehensively from the top of their body (i.e. from the 'head') downwards (i.e. to the 'toes'). When conducing a head-to-toe assessment, nurses asses each body system in turn, and then use the data they gather to develop a detailed overall understanding of the patient's condition.
It is important to highlight that each nurse's approach to completing a head-to-toe assessment is unique. As a student or a new graduate nurse, it is essential that you determine the assessment practices which best suit you. The only requirement for a head-to-toe assessment is that the process is systematic and comprehensive - that is, that the nurse examines and evaluates all parts of all the body systems, so that no data is omitted.
The head-to-toe assessment begins with the observation of a client. The nurse should observe the patient as they enter the assessment room, noting their gait, posture and ease of movement, etc. As the nurse introduces themselves to the patient, they should observe the patient's communication ability, their physical appearance and their general mental alertness / orientation / thought process. The goal of observation is to identify any obvious problems which may need to be addressed before a more comprehensive assessment can begin, or which may inform the focus of this health assessment.
Once a nurse has completed their observation of a patient, they can progress to completing the head-to-toe assessment. This is done in two parts:
- The primary survey, which involves assessing the patient's life-sustaining body systems.
- The secondary survey, which involves a more comprehensive assessment of the patient.
Remember: the primary survey involves physically assessing the patient's life-sustaining body systems to identify issues which may immediately threaten their life or wellbeing. It involves four stages, which may be remembered using the 'ABCD' mnemonic:
|
A |
Airway |
This step involves assessing the patency of the airway. A nurse should observe the patient for dyspnoea (which may also be indicated by the inability to vocalise), excessive upper respiratory secretions, respiratory problems such as coughing / choking, and airway trauma, etc. |
||||||||
|
B |
Breathing |
This step involves assessing the adequacy of the patient's breathing and gas exchange. The nurse should observe the patient for dyspnoea, paradoxic or asymmetrical movements of the chest wall, accessory muscle use, changes in the breath sounds, cyanosis, tachycardia and hypertension, etc. |
||||||||
|
C |
Circulation |
This step involves assessing the functioning of the cardiovascular system and determining whether the patient has adequate blood volume. The nurse should assess the quality and rate of the pulse, capillary refill time, and skin colour and temperature. |
||||||||
|
D |
Disability |
This step involves briefly assessing the patient's neurological system, including their level of consciousness. Another simple mnemonic - 'AVPU' - is used to prompt nurses during this step:
During this step of the primary survey, other disabilities - for example, obvious physical or psychological problems - may also be identified. These are explored further in the secondary survey. |
A crucial part of the primary survey is measuring and recording the vital signs - that is, blood pressure, pulse (heart rate), respiratory rate, temperature and blood oxygen saturation. You will study the processes involved in measuring and recording the vital signs in detail in a following chapter of this module.
Once a primary survey has been completed, as described, the nurse can progress to the secondary survey. Remember: a secondary survey involves a more comprehensive assessment of the patient. It is the core of the head-to-toe assessment, where each of the patient's body systems are examined and evaluated systematically and comprehensively, from the top of the patient's body (i.e. from the 'head') downwards (i.e. to the 'toes'). This involves using four key techniques:
- Inspection - assessing a part of the body by observing it.
- Palpation - assessing a part of the body by touch (e.g. a nurse may palpate internal organs like the liver, or external areas of the body such as joints / muscles, etc.). The nurse may use their palmar surfaces and finger pads to determine position, texture, size, consistency, masses, fluids, crepitus, pulsations, etc.
- Percussion - assessing the contents of a space in the body by tapping it with a finger (e.g. tapping the chest wall to assess for fluid in the lungs, etc.). Percussion is undertaken to evaluate the size, borders and consistency of the internal organs, to identify tenderness, and to detect the presence of fluid in a body cavity. When percussing the body, the nurse should expect to hear the following sounds:
|
Area Percussed |
Normal / Expected Sounds |
|
Lungs |
Resonant tone; loud intensity; low pitch; long duration; hollow quality. |
|
Bone, muscle |
Flat tone; soft intensity; high pitch; short duration; extremely dull quality. |
|
Viscera, liver |
Dull tone; medium intensity; medium to high pitch; medium duration; 'thud-like' quality. |
|
Stomach, gas in intestines |
Tympanic tone; loud intensity; high pitch; medium duration; 'drum-like' quality. |
|
Air trapped in lungs (e.g. in emphysema) |
Hyper-resonant tone; very loud intensity; very low pitch; longer duration; booming quality. |
- Auscultation - listening to sounds (e.g. using a stethoscope to listen to the heart, breath sounds in the lungs, or the noises of the gastrointestinal system, etc.).
The nurse should assess:
|
Body Region |
Examples of Health Observation and Assessment |
|
The head and face |
|
|
The eyes |
|
|
The ears |
|
|
The nose, mouth and oropharynx |
|
|
The neck |
|
|
The upper extremities |
|
|
The posterior chest |
|
|
The anterior chest |
|
|
The abdomen |
|
|
The lower extremities |
|
|
The neurologic system |
|
|
The genitalia and rectum (if indicated) |
|
It is important that nurses are familiar with - and that they comply with - their organisation's policies and procedures for health observation and assessment. For example, when a nurse is examining a patient's private areas (e.g. the genitalia and rectum), many organisations require a second nurse to be present. In order to perform an assessment using a particular technique, it is also important that nurses are appropriately trained in the correct use of that technique, and in the data it returns.
To support the head-to-toe assessment, there are a range of other focused assessments which may be completed - for example:
- Blood glucose levels.
- Blood laboratory studies (e.g. typing and cross-matching, coagulation profiling, haemoglobin, blood urea nitrogen, creatinine, toxicology screening, arterial blood gasses, electrolytes, liver / cardiac enzymes, etc.).
- Comprehensive neurological evaluation (e.g. using the Glasgow Coma Scale, or a similar standardised assessment tool).
- Diagnostic imaging studies (e.g. X-rays, CAT scans, MRI scans, etc.).
- Electrocardiogram (ECG) monitoring.
- Height, weight and Body Mass Index (BMI).
- Mental health assessment.
- Neurovascular function (e.g. limb colour, temperature, pulses, sensation and motor function).
- Pain assessment.
- Sensory perception (e.g. vision, hearing, touch, etc.).
- Skin assessment (e.g. colour, integrity, turgor, diaphoresis, etc.).
- Urinalysis (e.g. for blood, glucose, protein, specific gravity, etc.).
You will study the processes involved in completing many of these different types of focused assessments in a later chapter of this module.
It is important that nurses are familiar with the variety of different pieces of equipment which may be used in the assessment of a patient. This equipment may include (but is not limited to):
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Remember: as described in earlier sections of this chapter, the type of screening used by a nurse depends on: (1) the context in which the nurse is working, and (2) the health care issues and needs of the patient being assessed; additionally, each nurse has their own unique approach to conducing a head-to-toe assessment. The only requirement for a head-to-toe assessment is that the process is systematic and comprehensive - that is, that the nurse examines and evaluates all the body systems, so that no data is omitted. When assessing a patient, it is important that you are organised and prepared with the equipment you need. It is important that you develop a routine, and that you practice this so you develop confidence implementing it in practice.
NOTE: When undertaking health observation and assessment, there are a number of age-related variations. You will study the skills involved in assessing children, pregnant women and older adults in a later chapter of this module.
If you need assistance with writing your essay, our professional nursing essay writing service is here to help!
Find out moreDocumenting health observation and assessment findings
The previous section of this chapter described in detail the processes involved in completing a head-to-toe assessment of a patient, including a primary and secondary survey; you should revise this section now, if required. At each stage of the assessment, it is important that nurses document, or record in written format, the data they collect. This allows data to be: (1) used to determine the patient's clinical condition and make decisions about appropriate care, and (2) communicated between different professionals involved in the care of the patient.
As described in an earlier section of this chapter, there are a variety of different ways that data can be recorded, and this generally differs between clinical settings and organisations; nurses are encouraged to familiarise themselves with the documentation strategies used in the organisation where they work. Nursing documentation may be recorded in hard-copy (paper) or electronic (digital) form. Regardless of how data is recorded, however, documentation must:
- Be complete, accurate, concise, legible and free from bias.
- Record facts, without the use of non-committal language (e.g. 'appears', 'seems', etc.).
- Be written contemporaneously, or as close to the time of collection as possible.
- Include the name, signature and designation of the nurse who created it.
- Be unaltered; if errors are made, these must be struck through with one line and initialled.
- Be kept securely, an in a way which protects the patient's right to confidentiality.
- Avoid using acronyms, abbreviations, jargon and archaeic terms.
- Use short sentences and simple words.
- Involve the patient and their significant others, and use language they understand.
As stated by the National Health Service's (NHS, 2010: p. 2) CG2 - Record Keeping Guidelines, "[r]ecords must demonstrate a full account of the assessment made, the care planned and provided and actions taken, including information shared with other health professionals."
Activity
You are encouraged to read the National Health Service's (NHS, 2010) CG2 - Record Keeping Guidelines, or the current equivalent. This guideline can be obtained online, by searching for its title.
It is important to remember that creating and maintaining appropriate documentation, in a manner consistent with relevant legislation and policies, is a legal, ethical and professional requirement for nurses practicing in the UK. Health records provide evidence about the type of assessment and care patients receive. They are also important clinical tools, enabling continuity of care and effective decision-making about the type of care a patient receives.
Activity
You are encouraged to read the Information Governance Alliance's (2016) Records Management Code of Practice for Health and Social Care, or the current equivalent. This document can be obtained online, by searching for its title.
Conclusion
As you have seen throughout this chapter, nurses undertake health observation and assessment constantly, in all clinical settings; therefore, it is essential that nurses are able to complete an accurate, comprehensive and systematic health observation and assessment of a variety of different patients. This chapter has provided a broad introduction to health observation and assessment. It began with an overview of health observation and assessment - describing its place in the nursing care cycle, the key steps involved, the application of clinical judgement to understand data collected, and the different approaches which may be used. This chapter then went on to describe the process involved in conducting a head-to-toe assessment, including a primary and secondary survey, to collect data from a patient in an accurate, comprehensive and systematic way. Finally, this chapter described the correct documentation, or recording, of data collected during health observation and assessment. In completing this chapter, you have begun developing the knowledge and skills necessary to conduct a health observation and assessment in your nursing practice.
Reflection
Now we have reached the end of this chapter, you should be able:
-To explain the place of health observation and assessment in the nursing care cycle.
-To list and describe the three key steps involved in health observation and assessment.
-To explain the difference between signs (objective) and symptoms (subjective).
-To describe the application of clinical judgement to understand assessment data.
-To discuss cultural considerations related to health observation and assessment.
-To describe the processes involved in conducting a systematic head-to-toe assessment of a patient, including completing a primary survey and a secondary survey.
-To be able to accurately document health observation and assessment findings.
Reference list
Beach, J. & Oates, J. (2014). Maintaining best practice in record-keeping and documentation. Nursing Standard, 28(1), 45-50.
Cox, C. (2009). Physical Assessment for Nurses (2nd edn.). West Sussex, UK: Blackwell Publishing, Ltd.
Information Governance Alliance. (2016). Records Management Code of Practice for Health and Social Care. Retrieved from: http://systems.digital.nhs.uk/infogov/iga/rmcop16718.pdf
Jensen, S. (2014). Nursing Health Assessment: A Best Practice Approach. London, UK: Wolters Kluwer Publishing.
National Health Service. (2010). CG2 - Record Keeping Guidelines. Retrieved from: http://www.nhsprofessionals.nhs.uk/download/comms/cg2%20-%20record%20keeping%20clinical%20guidelines.pdf
Royal College of Nursing. (2004). Nursing Assessment of Older People. Retrieved from: https://www2.rcn.org.uk/__data/assets/pdf_file/0010/78616/002310.pdf
Wilson, S.F. & Giddens, J.F. (2005). Health Assessment for Nursing Practice (4th edn.). St Louis, MI: Mosby Elsevier.
Cite This Work
To export a reference to this article please select a referencing style below: