Graduating from a nursing program and accomplishing the long cherished journey to become Registered Nurse gives the sense of pride to many new graduate nurses. However, most nurses face challenges while separating from student life to professional life. According to Evans (2001) transition is a period of separation that causes uncertainty, insecurity and anxiety among new graduates. Moreover, Evans (2001) also identified that new graduates also expressed feelings of excitement, achievement, pride and motivation for the new role. Nevertheless, initial anxiety and happiness both the feelings are important for adapting the new role while facing the realities of professional life. The journey of transition for new graduates often remains challenging, stressful and frustrating. Most of the new graduates’ transition to the ward in the hospital environment often complains of an inability to perform their tasks within the time frame of their shift. The primary factors include increase nurse patient ratio, acuity of patients, paper documentation and complex electronic documentation, collaboration with multidisciplinary team etc. In addition, the beginning year for the new graduates usually overwhelming in terms of leaning new work environment, skills, policies and procedures, interacting with management and other healthcare professionals. It has been also observed that despite having intense clinical practicum and extensive orientation program, new graduates still feel lack of confidence while working independently in the hospital environment during transition phase. If this is a case for novice nurses working in wards, then critical care areas are even more complex and high tech skilled specialty to accommodate them.
Defining Critical Care Nursing
Critical care nursing requires licensed professional nurses to be able to provide competent care with confidence in the dynamic and critical environment where patient’s condition changes rapidly and unpredictably. Moreover, these rapid changes lead to life threatening situations which have to be dealt vigilantly. Freiburger (2002) stated that confidence in nursing practice is an important concern for the nurses working in critical care areas (intensive care units, cardiac care units, emergency departments, post anesthesia care rooms and so forth) as it is directly associated to competency. Critical care nursing is one of the most difficult, hectic, demanding and stressful specialty considered beyond the level of new graduates. Any complex practice depends on both extensive acquisition of set theoretical knowledge into practice (Benner, Sutphen, Leonard & Day, 2009). Critical Care Nurse (CCN) are the ones who depend on the specific body of knowledge, skills and expertise to provide optimal care, create healing and caring environment for not only patients but for the families or caregivers also. CCN perform clinical practice in a setting, where, patients necessitate complex assessment, high-intensity therapies, interventions, and continuous nursing observations. In addition, they should have expertise to be autonomous in making right decisions and clinical judgments to support patients and families (Vance, Koczen, Mcgee, Kuzma, & Butler, 2010). However, new graduates lack these skills, knowledge and experience to ensure patient safety, manage high-tech expertise and cope with work pressure under stressful environment (Carayon & Gurses, 2005). Moreover, the early and sudden entry of new graduates into the real world of high skilled specialty causes reality shock and often burn out. Therefore in my judgment I believe that new graduates should not assign in critical care areas right after the graduation.
Significance
According to Konvner, Brewer, Fairchild, Poornima, Kim and Djukic (2007) that 30% to 40% of new graduate nurses leave their first job within the first year due to facing a lot of challenges in critical care areas which includes lack of confidence, anxiety, critical thinking, monitoring hemodynamics and cardiovascular support and fear of managing life threatening situation. This attrition not only increases the nursing shortage but also will be costly for the hospital and other healthcare organization. New graduates often are stressful about lack of experience; lack of organizational skills, nursing procedures, clinical skills (assessing patients and administrating medications) and non-clinical skills (communicating with physicians, coordinating care and patient and family education) which ultimately lead to stressful transition or reality shock. Marlene Kramer (1979) was the first one who called this feeling which resulted from such a situation as reality shock and noted that the new graduate nurses often experience psychological stress and are less able to perceive the entire situation and to solve problems. As a result, the consequences of stress will lead to increase clinical errors which do not support safe patient care. Pellico, Brewer and Kovner (2009) investigated the experiences of newly licensed nurses’ stress which resulted from conflicting demands of practice realities, including compromised quality of patient care, time and workload pressures, staffing shortages, and the ideals of patient-centered, evidence-based, quality, and safe patient care.
Critical care units require nurses who are area specific qualified and experienced. The importance of specific knowledge practice gap and its impact in the initial phase of working in wards or critical care areas always has been a major challenge for the graduate nurses, senior nurses who provide mentorship and definitely the healthcare organization as whole. They feel unprepared to be accountable and responsible in taking care of critical patients and collaborate with healthcare professionals due to lack of knowledge and experience. In the academia, although student nurses are given intense education and skill practices under sheltered and secure environment. On the other hand, things are entirely different in the real practice settings to work independently especially in high-tech skilled clinical environment which creates anxiety and uncertainty among new nurses. Duchscher and Cowin (2004) supported the idea that the new graduates may experience inherent value discrepancies between the academic environment in which they have been raised and the real practice into which they are being initiated. However, Whitehead (2001) highlighted that the initial anxiety and feelings of uncertainty is a normal part of transition and it diminishes with experience only.
Novice nurses also feel uncomfortable in communicating and collaborating with physicians and other healthcare professionals at the entry level in the wards or critical areas. A study done by Hemani (1996) in Pakistan emphasized that due to nurse’s lack of technical and professional knowledge; doctors treated them as their handmaidens rather than as their colleagues. Critical care units comprises of multidisciplinary team where strong and effective communication skills and collaboration are the basic requirement in planning patient care. Lalani and Dias (2005) in their study found out the response of study participants who were new graduates that communicating with physicians is frightening and intimidating during the initial adjustment phase for them. Moreover, similar findings have been also reported by Duchscher (2001) in her study that the new graduates shared the fear of physicians and therefore he suggested that nurse-physician communication should be clear and effective as it directly affects the patient’s care. In addition, Boswell, Lowry and Wilhoit (2004) suggested that improvement of nurse-physician communication is essential as it enhances the ability of the new nurses to serve as an advocate for the patient.
Scenario
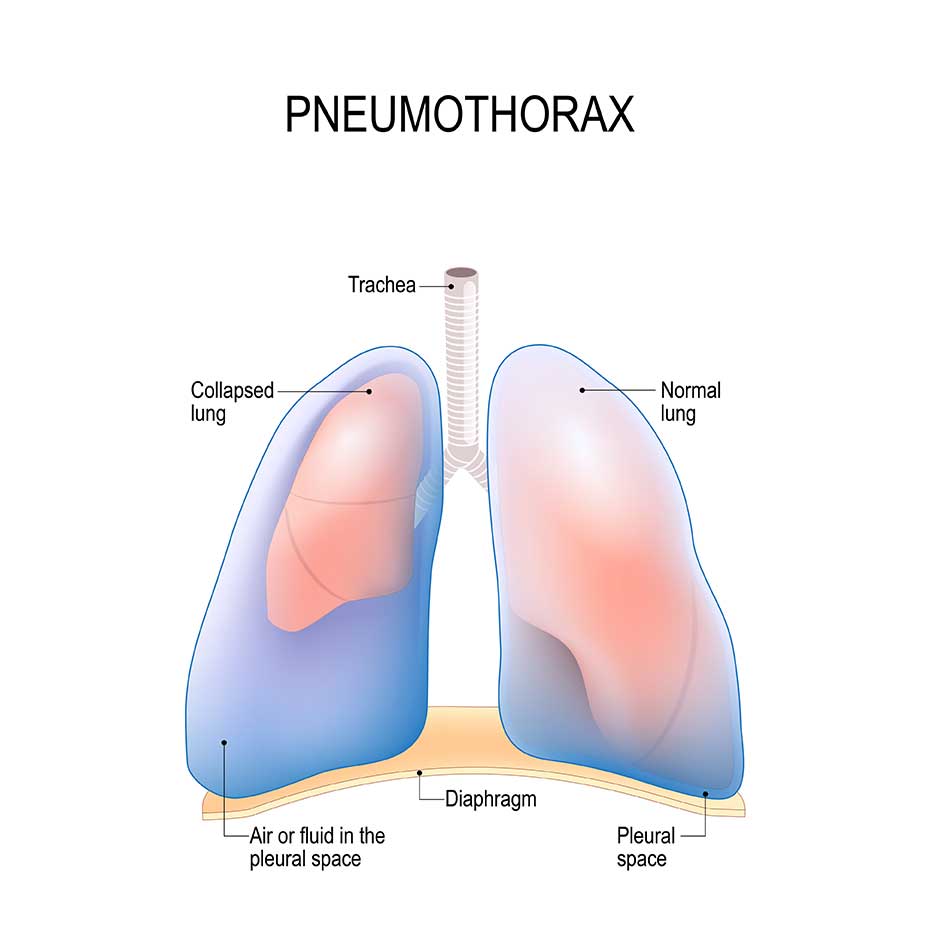
A novice nurse was working in ICU since 5 months and was assigned on one of a patient who was 20 years old, stable and about to transfer to the ward after having extensive treatment of acute respiratory distress syndrome (ARDS) and pneumonia. He was also inserted a chest tube due to pneumothorax and planned for the CT scan lungs before shifting to the ward. Doctor called the nurse to get ready the patient for the CT scan and then patient will be transferred to the ward directly after the scan. Nurse prepared everything and asked senior nurse to recheck her preparation. The senior nurse verified everything and signed off. But unfortunately when the senior nurse left, the novice nurse put the chest tube bottle on the bed and clamped it without asking from anyone as according to her she had learned somewhere that whenever patient goes for the scan or any procedure with chest tube, it has to be clamped. After clamping the chest tube the nurse was waiting for the doctor to accompany patient to the CT scan. It was observed that within 15 minutes of clamping, patient was gradually desaturating (spo2 from 97% to 80%), tachycardic (HR 120/min), hypotensive (BP 83/60mmhg) and the primary novice nurse was unable to assess the instability of hemodynamic. Eventually, at that time patient had a rush call having Pulseless electrical activity (HR 40/min) and code blue was announced. During CPR it was identified by the team leader that the chest tube which was inserted for the pneumothorax was clamped. It should not be clamped as air accumulated in the lungs and compressed the heart to function. Then the doctor unclamped chest tube and after 5 minutes of resuscitation, patient revived. The doctor investigated the whole situation and was very annoyed with the novice nurse. The whole situation was devastating for all of us at that moment as the patient life was at risk. This seems that even working on the stable patient, new graduates do not aware of the basic knowledge and practices. Moreover, they are also not prepared how to respond such life threatening condition and making the right clinical judgment for the patient.
Analysis & Conceptual Framework
Transition Shock in New Graduates’ Working in Critical Care Areas
The journey of new graduates is usually stressful, frustrating and discouraging also when they experience conflict role ambiguity and overwhelmed work environment. Duchscher (2007) viewed the transition shock in new graduates when they enter in the process of professional role adaptation. Especially nurses who work in intensive care areas are more prone to experience transition shock because of the complex and high skilled care setting where patient’s condition changes rapidly. Duchscher (2007) presented a transition shock model which highlights the journey of the students from the known role to less familiar role as a professional nurse. New graduates often experience contrast between the roles, responsibilities, knowledge and performance expectations which is required by the less familiar specific patient care settings such as critical care areas (refer appendix A). These areas require quick reflexes of the nurse to respond to critical situations of the patients, collaboration with physicians based on their specialized care knowledge, intuitions and experience which the new graduates are usually deprived of. In the scenario the novice nurse was having lack of knowledge that how to deal with the patient having chest tube for pneumothorax and she clamped it without knowing the consequences of it. Moreover, she did not even know how to relate the instability of hemodynamics of the patient which was caused because of the clamped chest tube. How can we ensure patient safety here or how can we say that our patients are in the safe hands? However, I believe that although the novice nurse was responsible for the patient at that time but who should be blame for? A novice nurse who has just finished her 5 months only in critical care area and still in transition phase and learning things or the healthcare institution who hire new graduates in critical care areas where patient collapse in minutes and requires experienced nurses only? The new graduates lack the depth and breadth that comes with experience (Roberts & Farrell 2003). The expectations from nurses in critical care areas are usually high and demanding which entail confidence in dealing crises situation and clinical judgment, administrating high alerts and life saving medications, and managing extensive clinical and non clinical interventions. The initial 3-4 months for the new graduates are crucial to overcome transition shock and get adjusted with the less critical area like wards where they can practice skills and learn routine work and also the processes in responding efficiently to life threatening conditions.
Stages of New Graduates’ Transition in Critical Care Areas
The newly graduates nurses when entering into professional practice; go through the process of adjustment at the beginning of initial 12 months. This initial period of work experience includes a complex but also a group of emotional, physical, intellectual, sociocultural and developmental concerns in adjustment phase. The sudden thrush of new nurses into the world of high technical or critical care area would be challenging, stress causing, and depressing while working with critical, death and dying patients. Therefore, new graduates should evolve through the stages of doing, being and knowing in the wards initially where they can have the grip of clinical expertise gradually and prepare themselves to manage patients in complex care settings (refer appendix B). The stage of “doing” involves learning, performing, concealing, adjusting, and accommodating. The stage of “being” includes searching, examining, doubting, questioning, and revealing. And the last stage is “knowing” which includes separating, exploring, recovering, critiquing and accepting the working environment (Duchscher, 2008).
Doing
The first stage doing encompasses 3 to 4 months for the new graduates in clinical area. In this stage new graduates entry marked by the instability of emotions and feeling of anxiety though the process of learning, and subsequently performing skills. They are at the primary level of understanding that what is expected from them and doing it well to complete their tasks on timely basis. However, in complex clinical context, advanced knowledge and application of skills become challenging because of lack of confidence, knowledge, experience, critical thinking, and unfamiliarity with the environment. As I mentioned in the scenario that the novice nurse was having lack of knowledge and experience of handling chest tube for the pneumothorax. Moreover, she was also not confident in assessing the instability of hemodynamics of the patient in order to take safe action on time and finally the patient was collapsed. Nevertheless, in the probation period they are budded for 3 months initially with preceptors and are given training in handling life threatening situation but 3 months are not enough to learn this complex task. Besides this, new graduates are also expected to do multi-tasking like managing unstable or dying patients, dealing with family issues, collaborate with physicians, administrating high alert medications which also require enough knowledge about the drugs, performing routine tasks and so forth. These all tasks for new graduates create stress and may lead to increase chances of errors where patients’ safety remains questionable.
Being
The second stage being encompasses next 4 to 5 months for the new graduates post orientation. This stage consists of rapid advancement in thinking, knowledge and skills as this stage advances the transition in searching, examining and revealing further knowledge and practices. In this stages novice nurses are confirming and clarifying their thoughts and actions. This motivates them in making clinical decisions to some extent and intervene nursing skills that are safe for the patients. Similarly, in relation to the scenario if the novice nurse had some previous experience of handling patients in critical situation in less complex clinical setting such as in wards, she will able to make clinical judgment at that time to act immediately to the crises situation. New graduates are also given further challenging task gradually such as unit assignments, managing stock medications, handling crash cart, and presenting case studies etc. to perform additional tasks beside nursing care. As time evolves with growing confidence, graduates feel more comfortable in adjusting with working environment. In addition, eventually they will require less physical, mental and emotional energy to manage with familiar nursing skills and clinical situations.
Knowing
The final Stage of transition “knowing” involves the initial 12 months post orientation for new graduates. This stage allows them to move from learning phase to the perceived phase with greater expectation where they can explore, recover and accept the work environment. They will be able to manage with roles, responsibilities and routine at more comfortable level. Furthermore, the critical thinking, clinical judgment and decision making skills will be more enhanced in order to respond quickly in life threatening situations and plan patient care accordingly. After going through with all three stages and completing the 12 months of transition period, these graduate nurses can be promoted to assign in critical care areas where they can utilized their learned knowledge and skills independently with more confidence. Moreover, later they can be enrolled in the specialty course (critical care certification program) gradually to be expert in their relative field.
Recommendations/Strategies
The demand of the critical care specialty can lead to frustration and burnout at very high rates among new graduates due to role transition anxiety. Therefore, to have a realistic view of smooth transition and to achieve job satisfaction among new graduates is crucial to retain nurses and overcome nursing shortage globally. Managing transition shock, assigning preceptors and coaches, making nursing peer support group and enrolling nurses in specialized critical care nursing certification program are some of the recommendations/strategies to provide safe patient care.
Solutions for Transition shock
The successful integration of new graduates in the real world of practice is a primary responsibility of the employers to accommodate them in smooth transition phase. They should be given less critical areas at the entry level to learn, understand, and adjust with the working environment. The role of clinical nurse instructor or supervisors is to arrange for experiences that would help them gaining increased competence in clinical practices. They should be given clinical responsibility and practice autonomy slowly to overcome transition shock (Roberts & Farrell, 2003). Besides this, new graduates should evaluate their own competencies, and self-appraise to analyze their own ability to function according to the expectations. If there is a lack in certain training skills, they should seek extra time to increase confidence and competency.
Preceptors and Coaches
Many new graduates are assigned to the preceptors, coaches and mentors as a part in orientation and probation period. The senior nurses’ are usually given the role of preceptor to assist novice nurses and has responsibility for supervising and evaluating the work. The preceptor-preceptee approach not only guides new nurses to become competent in practices but also develop relationship among junior and senior nurses. On the other hand, critical care areas do have preceptor-preceptee approach but the area usually gets so busy because of unstable patients almost all the time that preceptor sometimes cannot give full attention to the novice nurses which hinders their learning. Moreover, critical care areas require immediate clinical interventions and responses from experienced nurses in crises situations where novice nurses cannot respond quickly as they are still in learning and adjustment phase. Therefore, after completing the first 12 months of transition in wards, when they assign to the critical care areas they will still be given strong, supportive, prolonged preceptorship in order to understand the norms, culture and the nature of working environment of the specific area. But at that level they must have enhanced critical thinking, knowledge and experience to the extent where they can work independently and will be learning more advance technical skills on daily basis.
Nursing Peer Support
New nurses often experience more anxiety and stress after detaching from the preceptor and moving to independent practice. Therefore, peer support group plays a vital role here to provide comfort and assistance to new nurses’ in working independently. This also helps them to ask questions confidently, seek clarifications from the peer, and establish friendly relationship and environment as well. Moreover, nursing peer support group gives an environment where new nurses feel more comfortable, learn without hesitation, and feel encouragement by working together.
Specialized Orientation Program or Certifications
According to American Association of Critical Care Nurses’ (AACN), most acute care hospitals offer prolonged orientation program and almost 6-12 weeks of critical care course for the nurses to have professional knowledge and proficient in technological skills. Moreover, AACN also offers special certification course of Critical Care Registered Nurse (CCRN) – Acute/Critical Care Nursing (Adult, Pediatric & Neonatal) to deliver quality of care based on standard and specific area of knowledge and expertise. However, novice nurses in the initial stage only learn the routine tasks as well as building knowledge and experience in order to jump into the more complex expert area. This can be achieve once they complete the first 12 months of the clinical experience and can be enrolled or nominated in critical care courses to enhance further knowledge and practices. In 2006, Aga Khan university Hospital, Karachi, Pakistan had started Critical Care Diploma distance learning program of 1 year with the affiliation of George Brown university in Ontario, Canada for critical care area’s nurses’ to learn specialized course to be expert in delivering patient care in critical care units.
Limitations
One of the biggest challenge and limitation in the nursing profession is nursing shortage. The current global shortage of nurses is growing faster than the rate at which new nurses are graduating (Duchscher, 2008). Therefore, nurses are required in all the areas including critical care units. The question is that can novice nurses replace seniors nurse in critical care areas? Roberts and Farrell (2003) stated that growing rates of nurse resulting in the replacement of highly competent and experienced practitioners with newly graduated nurses who have neither the practice expertise nor the confidence to navigate a clinical environment burdened by escalating levels of patient acuity and subsequent nursing workload intensity. According to AACN (2004), in this critical situation as an option only we can assign novice nurses in critical care areas provided with intense expert mentoring, prolonged preceptorship, time and guidance to mature them as experts. Moreover, in support Proulx and Bourcier (2008) acknowledged that a specialized course program for orienting new nurses in the intensive care units should focus on helping them become technically proficient quickly and providing consistent instruction. On the other hand, AACN (2004) also stated that although new graduate nurses are needed by critical care units but they lack confidence, clinical judgment, and critical decision making and problem solving skills to respond in crises or life threatening conditions. But again, patient’s safety is at risk if they do not get enough knowledge and experience opportunity in healthcare facility.
Conclusion
The new graduates generally have limited practical nursing experience, lack social and developmental maturity and struggle with basic clinical work management skills and also balancing time with responsibilities and task. In general, they comforts with the routines of their unit and their familiarity with roles and responsibilities that have been established by the experiences gained during the initial months of their transition serve as a foundation from which they can predict and respond to presenting situations (Duchscher, 2008). On the other hand, nurse working in critical care areas have to be vigilant, competent and expert to provide quality of care to the patients. In addition, the expert level is much more flexible and skilled at integrating the elements on timely performance such as clinical grasp of an entire situation using anticipatory thinking, ethical care giving to patients and families, skillful engagement and respectful relationships with patients, families and co-workers, the management of breakdown and technical hazard, communication and negotiation skills and competency in critical thinking and clinical judgment to respond to life threatening situations.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "pneumothorax"
Patients can develop a pneumothorax from various means and either (primary or secondary) can occur spontaneously. A primary pneumothorax is reserved for those without any underlying lung pathology, while the term “secondary” pneumothorax is used clinically to indicate patients that carry an established diagnosis of lung disease.
Related Articles