Talc Pleurodesis: An Overview
Introduction
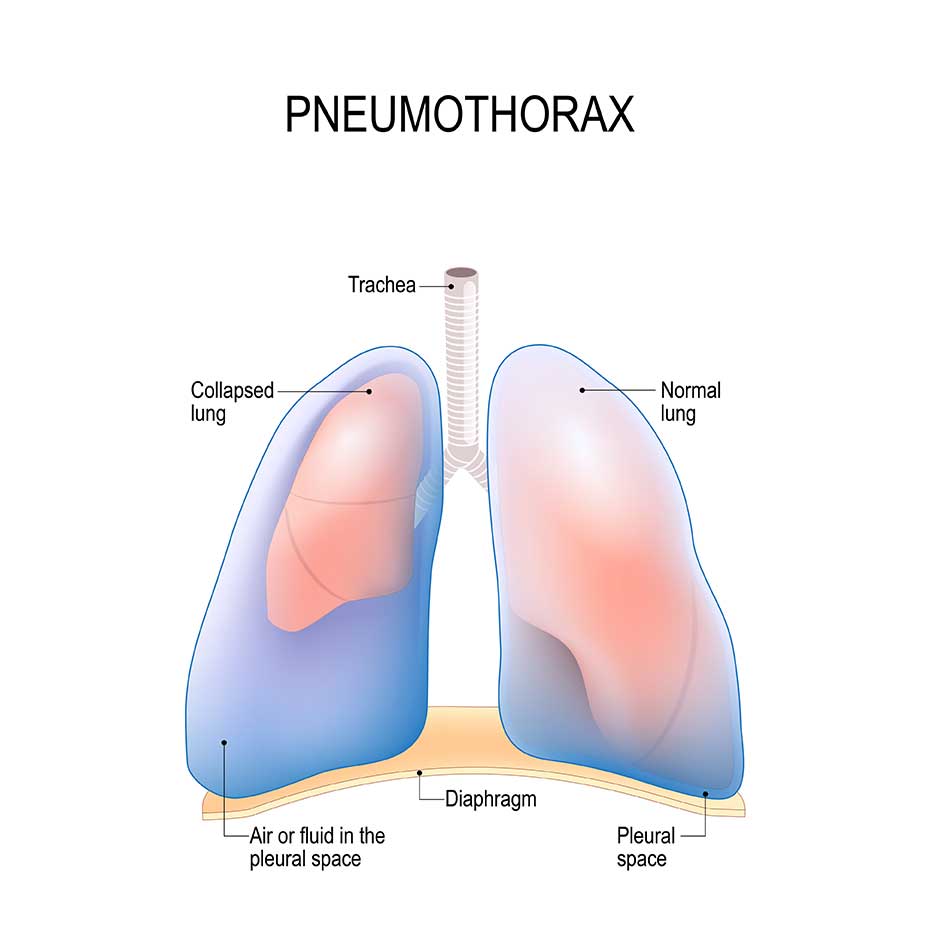
While on the pulmonary service this month I encountered several patients with recurrent pleural effusion or pneumothorax. The Pulmonary Group I worked with were consulted on lots of patients with lung cancer, along with a myriad of other etiologies. In the United States, metastatic pleural effusions affect in excess of 150, 000 people per year.1 Patients that experience a secondary pneumothorax can often times expect to have another collapsed lung at some point in their lifetime, as studies have reported recurrence rates between 17% and 49%.2 There are various approaches to the treatment of recurrent pneumothorax and pleural effusions. One procedure that is used to prevent recurrent pleural effusion or pneumothorax or in the treatment of a persistent pneumothorax, is pleurodesis. Pleurodesis is a procedure that is used to obliterate the space between the visceral and parietal that exists between the lung and chest wall.3 Pleurodesis can be achieved by video-assisted thoracoscopic surgery (VATS) or via tube thoracoscopy4. Instillation of a chemical irritant by either route can cause apposition of the lung and chest wall, thus helping to prevent recurrent pneumothorax or pleural effusion5. The effectiveness of chemical pleurodesis using talc will be discussed in this paper6.
Mechanism of Action and Indications
A variety of chemical sclerosing agents that can be used for pleurodesis currently exist and include bleomycin, tetracycline, and autologous blood patch to name a few2. Talc used for pleurodesis in the United States currently is available in both, sterile powder and aerosolization, and is considered the sclerosing agent of choice1. When used as a powder it is commonly mixed with saline and referred to as a “slurry”1. The talc can be instilled via VATS or tube thoracoscopy2,3. Once the slurry comes in contact with the protein-rich environment of the lung tissue, an acute inflammatory response occurs along the surface of the lung, which serves to help the actual lug tissue adhere to the chest wall itself3. As part of the inflammatory response, inflammatory mediators such as adhesion molecules, interleulin-8 (IL-8), and vascular endothelial growth factor (VEGF) to mention a few3.
Persistent or recurrent pneumothorax
Patients can develop a pneumothorax from various means and either (primary or secondary) can occur spontaneously. A primary pneumothorax is reserved for those without any underlying lung pathology, while the term “secondary” pneumothorax is used clinically to indicate patients that carry an established diagnosis of lung disease6. In patients with secondary pneumothorax or recurrent pneumothorax, talc pleurodesis is considered an excellent alternative to surgical pleurodesis2,4. This is an especially effective alternative to those who may be poor surgical candidates, secondary to their poor underlying lung function4. Pleurodesis in patients with persistent air leak secondary to a primary spontaneous pneumothorax, or for those with their first secondary pneumothorax and studies have demonstrated a reduced “in hospital” time and more cost effectiveness, and therefore should be considered as a therapeutic intervention2,5,6.
Malignant Effusions
Patients with metastatic pleural effusion (MPE) are among some of the most frequently seen on a pulmonary service for recurrent pleural effusions1,3. This can be especially true in those with advanced malignancy. Often times these oncologic patients are in need of palliative relief of their respiratory symptoms just to get through the day1. In some patients with malignancy, their pleural effusion, once drained, may reaccumulate rather quickly3. In this subset of patients, multiple thoracenteses may be needed to drain the malignant effusion, which can be costly, hazardous to the patient, and extremely taxing. Therefore, talc pleurodesis following drainage of malignant plural effusion should be a consideration as a possibility for improving the patients quality of life (QOL) and tailored to the specific needs of the patient1.
Contraindications
For pleurodesis to be successful there must be complete apposition between the visceral and parietal pleura2,3,5. If there is incomplete expansion of the lung tissue due to air or fluid, pleurodesis will not be effective2. Achieving complete apposition of the two pleural layers in a pneumothorax typically isn’t a problem, but in MPE this can sometimes be difficult3. The issue in MPE can arise when the tumor burden is high or the lung parenchyma develops a rind around its outer layer, preventing complete lung re-expansion3. This is often referred to as “trapped lung”, and as such, pleurodesis would be futile3. Therefore, patients with trapped lung secondary to MPE would benefit most from the placement of a long-term catheter that would stay in place and be used to drain the chest as needed3.
Patient Preparation
When preparing the patient for pleurodesis, it is important to make sure you have achieved optimal apposition of the visceral and parietal pleural surfaces6,7. The first step in doing so, would be ensuring the pleural space has been adequately evacuated of air or pleural fluid. A chest radiograph can aid the clinician in determining adequate apposition of the lung surfaces, however, in my experience gained while on the pulmonary rotation, a bedside ultrasound can be easily used at the bedside and is very effective in evaluating the pleural space, but without exposing the patient to any additional radiation6.
Since the purpose of the pleurodesis is to elicit an inflammatory response, thus “roughing up” the lung so it will adhere to the chest wall, it is important to make sure the patient has been free of glucocorticoids for several days prior to pleurodesis3,7. The opposite is true for non-steroidal anti-inflammatory drugs (NSAIDS), therefore the patient may continue to use NSAIDS without affecting the success of the pleurodesis procedure7. In fact, since the patient will likely experience a fever post-procedure, patients are often times pre-treated with an NSAID prior to the actual procedure7-9. Another drug class that has been called into question during pleurodesis is anticoagulants7. If the patient is having a chest tube placed or is being prepared for VATS surgery, it will be necessary to reverse any anticoagulants7. However, it is not necessary to suspend or reverse anticoagulation for the pleurodesis if an indwelling catheter or chest tube is already in place7.
Once the pleural space has been completely drained and radiographic or ultrasound evidence of full lung expansion has bee properly verified, administration of the talc slurry can be instilled into the chest tube3,7. The slurry is prepared by injecting 50mL’s of normal saline into the sterile talc powder bottle7. The saline and powder are mixed by swirling the bottle7,8. After adequate mixing, the slurry can be aspirated out of the talc bottle using a 60mL Leuer lock syringe7. Due to the painful nature of the chemical reaction that takes place during pleurodesis, these patients should be premedicated with pain medicine or an anxiolytic3,7. As another means of trying to reduce any discomfort, most providers will instill 25mL’s of one percent lidocaine into the pleural space several minutes prior to administering the talc slurry7,8.
Talc slurry, once injected into the pleural space, does a poor job of distributing equally in the pleural space7. Studies have shown that positional changes in the patient have not shown any improvement in outcomes for a successful pleurodesis3,7. However, many clinicians still ask their patients to rotate into several different positions once the full volume of slurry has been instilled, to ensure maximum distribution. Once the procedure is complete and the clinician feels that maximal slurry distribution has been achieved, the chest tube can be removed within 24 hours, so long as the lung remains up and chest tube drainage is less than 150mL’s per day7,8.
Potential Complications
As with any medical procedure, talc pleurodesis is not without possible complications7,8. The provider should be well aware of these complications and these should be adequately discussed and explained to the patient prior to the talc slurry instillation. While talc pleurodesis is by and large well tolerated, some complications that have been documented range from very minor to very severe, and even include death7-9. Some of the minor complications seen with pleurodesis include fever, cough, pain3,7. These are all described as typical responses that are commonly seen secondary to the inflammatory response that is occurring in the pleural space of the lung7,8.
Some of the more serious complications that have been reported in the literature include chest pain, hypoxemia, hypotension, and acute respiratory distress syndrome (ARDS)3,7,8. The exact pathogenesis of the acute lung injury seen in ARDS as a result of talc pleurodesis remains elusive and may be multifactorial7. In the past it was believed to be related to the administration method used for instillation, but studies have found this less likely to be the case, and may be instead, related to the talc particle size and volume7,9. To avoid potential adverse reactions, it is recommended that the volume of talc instillation be limited to five grams7. In addition to dosing, particle size has also been linked to adverse reactions7. It is therefore recommended to use medical grade talc with less than ten percent of the particles measuring five to ten microns7. It is believed these smaller particle sizes can create a systemic inflammatory response and lead to ARDS3,7,9.
Conclusion
While many options remain available for the treatment of recurring pneumothorax and pleural effusion, chemical pleurodesis should be a consideration for the provider caring for patients with diseases of the chest2. Various agents are on the market, but talc has been shown to be the sclerosing agent of choice in the United States3,7. However, clinicians need to be aware of the various preparations, as particle size varies depending on the manufacturer and vary from one country to another5,7.
Chemical pleurodesis along with VATS surgical intervention is an effective form of treatment for patients with recurrent effusions or pneumothorax2,6,7. Unfortunately, not all patients are candidates for the procedure, so proper patient selection must be exercised6,7. In addition to being effective, chemical pleurodesis using talc can be done at the bedside. The procedure is relatively safe and well-tolerated by the patient, so long as the patients is premedicated with adequate analgesia6,7,9. For patients this procedure is an excellent option if they are not a surgical candidate, need palliation, or are simply seeking resolution for their recurring pulmonary issue1,3,7. Lastly, talc pleurodesis comes as a significant time and cost saving for the patient and overall healthcare system6,9.
References:
1. Guinde J, Georges S, Bourinet V, Laroumagne S, Dutau H, Astoul P. Recent developments in pleurodesis for malignant pleural disease. Clin Respir J. 2018;12(10):2463-2468.
2. How CH, Hsu HH, Chen JS. Chemical pleurodesis for spontaneous pneumothorax. J Formos Med Assoc. 2013;112(12):749-755.
3. Rodriguez-Panadero F, Montes-Worboys A. Mechanisms of pleurodesis. Respiration. 2012;83(2):91-98.
4. Elsayed HH, Hassaballa A, Ahmed T. Is video-assisted thoracoscopic surgery talc pleurodesis superior to talc pleurodesis via tube thoracostomy in patients with secondary spontaneous pneumothorax? Interact Cardiovasc Thorac Surg. 2016;23(3):459-461.
5. Chen JS, Chan WK, Yang PC. Intrapleural minocycline pleurodesis for the treatment of primary spontaneous pneumothorax. Curr Opin Pulm Med. 2014;20(4):371-376.
6. Hallifax RJ, Yousuf A, Jones HE, Corcoran JP, Psallidas I, Rahman NM. Effectiveness of chemical pleurodesis in spontaneous pneumothorax recurrence prevention: a systematic review. Thorax. 2017;72(12):1121-1131.
7. Noppen MM. Talc Pleurodesis. Up To Date. Retrieved September 5, 2019 from https://www-uptodate-com.ezproxy3.lhl.uab.edu/contents/talc-pleurodesis?
8. Keeratichananont W, Kaewdech A, Keeratichananont S. Efficacy and safety profile of autologous blood versus talc pleurodesis for malignant pleural effusion: a randomized controlled trial. Therapeutic Advances in Respiratory Disease. 2018;12:1753466618816625.
9. Brant A, Eaton T. Serious complications with talc slurry pleurodesis. Respirology. 2001;6(3):181-185.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "pneumothorax"
Patients can develop a pneumothorax from various means and either (primary or secondary) can occur spontaneously. A primary pneumothorax is reserved for those without any underlying lung pathology, while the term “secondary” pneumothorax is used clinically to indicate patients that carry an established diagnosis of lung disease.
Related Articles