Introduction: A progressive rise in the number of patients accepted for renal replacement therapy has been reported world wide . Permanent vascular access (VA) is the life-line for the majority of these patients, when hemodialysis is the treatment of choice. Thus, the successful creation of permanent vascular access and the appropriate management to decrease the complications is mandatory. A well functional access is also vital in order to deliver adequate hemodialysis therapy in end stage renal disease (ESRD) patients. Unfortunately, despite the advances in hemodialysis technology, in the field of vascular access in the last years the introduction of the polytetrafluoroethylene (PTFE) graft and the cuffed double lumen silicone catheter were the only changes. But the cost of vascular access related care was found to be more than fivefold higher for patients with arteriovenous graft (AVG) compared with patients with a functioning arteriovenous fistula (AVF) . It seems that the native arteriovenous fistula that Brescia and Cimino described in 1966 still remains the first choice VA . Thereafter, vascular access still remains the “Achilles heel” of the procedure and hemodialysis vascular access dysfunction is one of the most important causes of morbidity in this population . It has been estimated that vascular access dysfunction is responsible for 20% of all hospitalizations and the annual cost of placing and looking after dialysis vascular access in the United States exceeds 1 billion dollars per year . Nowadays, three types of permanent vascular access are used: arteriovenous fistula (AVF), arteriovenous grafts (AVG) and cuffed central venous catheters. They all have to be able to provide enough blood flow in order to deliver adequate hemodialysis, have a long use-life and low rate of complications. The native forearm arteriovenous fistulas (AVF) have the longest survival and require the fewest interventions. For this reason the forearm AV, is the first choice, following by the upper-arm AVF, the arteriovenous graft (AVG) and the cuffed central venous catheter as a final step .
History of vascular access
Vascular access for hemodialysis is closely associated with the history of dialysis. Glass needles were employed as vascular access when hemodialysis came into view in 1924. The first haemodialysis treatment in humans was carried out by Haas G who used glass cannulae to acquire blood from the radial artery and reverting it to the cubital vein . Venipuncture needles were used as means for blood acquisition from the femoral artery and its reinfusion to patient by vein puncture, in 1943 by Kolff W. . Regular hemodialysis treatments were possible in 1950s through the use of a medical apparatus ( Kolff ‘s twin-coil kidney ), thus projecting the problem of a reliable, capable of repeated use vascular access. Today, the artery-side-to-vein-end-anastomosis has become a standard procedure . In 1952, Aubaniac had described the puncture of the subclavian vein .
In the 60s, by using Alwall’s experience, Quinton, Dillard and Scribner developed arteriovenous Teflon shunt . This procedure involved two thin-walled Teflon cannulas with tapered ends were inserted near the wrist in the forearm, one into the radial artery and the other into the adjacent cephalic vein. The external ends were connected by a curved Teflon bypass tube. Later, the Teflon tube was replaced by flexible silicon rubber tubing. After the advancement of permanent vascular access, the possibility of maintenance hemodialysis was a fact and therefore a groundbreaking procedure.
In the subsequent years many variants of the AV shunt were used, with the majority of them concerning temporary vascular access from the onset of chronic dialysis treatment compensating for the time of AV fistula’s absence or maturity. In 1961, Shaldon performed hemodialysis procedures by inserting catheters into femoral artery and vein, using the Seldinger-technique . Over time, vessels in different sites were used, including the subclavian vein jugular and femoral.
In 1962 Cimino and Brescia described a ‘simple venipuncture for hemodialysis’ . In 1963 Thomas J. Fogarty invented an intravascular catheter with an inflatable balloon at its distal tip designed for embolectomy and thrombectomy . The first surgically created fistula was placed in 1965, followed by further 14 operations in 1966. In 1966 Brescia, Cimino, Appel and Hurwich published their paper about arteriovenous fistula. Appell had performed a side-to-side-anastomosis between the radial artery and the cephalic antebrachial vein. One year later, in 1967, M. Sperling reported the successful creation of an end-to-end-anastomosis between the radial artery and the cephalic antebrachial vein in the forearm of 15 patients using a stapler . In the next few years this type of AV anastomosis received popular approval. However this procedure was cast aside as first choice AV, due to the increasing numbers of elderly, hypertensive and diabetic patients with demanding vessels and high risk of a steal syndrome. End-to-end-anastomoses are still a common place technique in revision procedures.
In 1968 Röhl L. published thirty radial-artery-side-to-vein-end anastomoses . After anastomosis was performed, the radial artery was ligated distal to the anastomosis, thus resulting in a functional end-to end-anastomosis. Today, the artery-side-to-vein-end-anastomosis has become a standard procedure . In 1970, Girardet R. and Brittinger W.D. described their experience with the femoral vein and artery for chronic hemodialysis. Experimental trials have been done by several authors in order to establish a permanent vascular access using subcutaneous tunnel. Brittinger W. was the first to implant a plastic valve as a vascular access in an animal model but unfortunately his efforts did not proceed to a human one . Moreover during the early 70s, Buselmeier T.J. developed a U-shaped silastic prosthetic AV shunt with either one or two Teflon plugged outlets which communicated to the outside of the body. The U-shaped portion could be totally or partially implanted subcutaneously . Subsequently pediatric hemodialysis patients were extremely favored by this procedure. New materials for AV grafts were presented in 1972, one biologic and two synthetic.. In 1976, L.D. Baker Jr. presented the first results with expanded PTFE grafts in 72 haemodialysis patients . In the years to come several publications indicated the benefits and the shortcomings of the prosthetic material in question remaining the primary choice of graft for hemodialysis VA to date. The same year two authors, Mindich B. and Dardik H. had worked with a new graft material: the human umbilical cord vein. . Regrettably so, this material did not succeed in becoming a revolutionary graft material due to its inadequate resistance against the trauma of repeated cannulation and their complication (aneurysm and infection). After the subclavian route for haemodialysis access was firstly introduced by Shaldon in 1961, it was further processed in 1969 by Josef Erben, using the intraclavicular route . In the next 20 years or so, the subclavian vein was the preferred access for temporary vascular access by central venous catheterization. Today, due to phlebographic studies revealing a 50% stenosis or occlusion rate at the cannulation site, subclavian route has been discarded. The subclavian stenosis and occlusion predispose to oedema of the arm, especially after creation of an AV fistula .
The first angioplasty described by Dotter et al who introduced a type of balloon, was immensely conducive to the resolution of one of the most significant predicaments in vascular surgery and vascular access surgery .
In 1977 Gracz K.C. et al created the ‘proximal forearm fistula for maintenance hemodialysis, a variant of an AV anastomosis . An adjustment of this AVF became quite significant in the old, hypertensive and diabetic patients on the grounds that it allows s a proximal anastomosis with a low risk of hypercirculation . In 1979 Golding A.L. et al developed a “carbon transcutaneous hemodialysis access device” (CATD), commonly known as “button”, as a blood access not requiring needle puncture . As a procedure of third choice, these devices were expensive and never gained widespread acceptance. Shapiro F.L. described another type of A.L. “button”, a device similar to that developed by Golding .
Angioaccess classification
Years after the initial efforts to create the appropriate vascular access in order to perform a safe hemodialysis, modern Nephrologists have now the possibility to select the appropriate access for their patients. So the first distinction is made between temporary and permanent VA . Temporary VA with expected half-life less than 90 days, peripheral arteriovenous shunts and non cuffed double lumen catheters are included . Mid-term VA with expected half life in 3 months to 3 years include veno-venous accesses (tunneled cuffed catheters and port catheter devices) and arteriovenous internal shunts, requiring vascular graft synthetic (PTFE) or biologic (saphenous vein, Procol, etc.) material ,or external shunt. Long-term VA with an expected half-life more than 3 years includes virtually the native arteriovenous fistulas and the new generation of PTFE grafts .
Acute hemodialysis vascular access
They are used for urgent hemodialysis and should be easy to insert and available for immediate use. Currently there are available two types of such accesses: Non-tunneled dialysis catheters and cuffed, tunnelled dialysis catheters.
Double-lumen, non-cuffed, non-tunnelled hemodialysis catheters are the preferred method for immediate hemodialysis when a long term access is not available. They are made of polymers which are rigid at room temperature to facilitate insertion but soften at body temperature to minimize vessel injury and blood vessel laceration. The proximal and distal lumens should be separated by at least 2 cm to minimize recirculation .
These catheters can be inserted into the central veins: femoral, jugular, or subclavian veins . The femoral artery can be used as an access central vein when all others central veins have been excluded. A modified Seldinger guide wire technique is used for their insertion. Image guided assistance in placing these catheters is recommended to avoid or minimize some of the immediate insertion complications, but non-cuffed catheters are also suitable for use at the bedside of the patient
The 2006 National Kidney Foundation Dialysis Outcomes Quality Initiative (K/DOQI) guidelines recommend, after internal jugular or subclavian vein insertion, identifying radiographically any potential complications and confirming tip placement prior to either anticoagulation or catheter use . These guidelines also recommend ultrasound vessel identification prior to insertion. In general, now the subclavian catheters should be avoided because of the high incidence of vein stenosis and thrombosis.
The maximum blood flow with this class of catheters is usually blood pump speeds of 300 mL/min, with an actual blood flow of 250 mL/min or less . Femoral catheters have to be at least 18 to 25 cm in length in order to have lower recirculation. The routine use-life of these catheters varies by site of insertion. In general, internal jugular catheters are suitable for two to three weeks of use, while femoral catheters are usually used for a single treatment (ambulatory patients) or for three to seven days in bed bound patients . However, the KDOQI guidelines suggest that non-cuffed, non-tunnelled catheters be used for less than one week and that cuffed, tunnelled catheters be placed for those who require dialysis for longer than one week . More recently a non-cuffed, non-tunnelled triple-lumen dialysis catheter has been developed. The purpose for third lumen is for blood drawing and the intravenous administration of drugs and fluid. In a multicenter, prospective study, blood flow rates and infectious complications were similar with double lumen catheter .
Infectious complications are the principal reason why the catheter must be removed.
Permanent Vascular Access
Taking into consideration patient factors such as life expectancy, comorbidities, and status of the venous and arterial vascular system is very important in order to prescribe the appropriate access. Other factors are determined by the type of access itself, as arteriovenous fistula (AVF), arteriovenous graft (AVG), or TC which have a different effect on circulatory system. Also the duration of their functionality and the risk for infection and thrombosis are important factors to consider. Each type of surgical anastomosis has advantages and disadvantages . In 2002 the American Association for Vascular Surgery and the Society for Vascular Surgery published reporting standards according to which three essential components of VA should be mentioned: conduit (autogenous, prosthetic), location and configuration (strait, looped, direct, etc.) .
Arteriovenous fistula
An AVF is the preferred type of vascular access; it has the lowest complication rates for thrombosis (~ one-sixth of AVGs) and infection (~ one-tenth of AVGs) .
There are 3 types of AVF s:
• First type when artery and vein are connected in their natural position, either with a side-to-side or a side-artery-to-vein-end anastomosis.
• Second type, where a vein is moved to connect to an artery in end-to-side fashion to either bridge a larger anatomical distance, or to bring the vein to the surface where it is accessible for cannulation and requires a tunnel to position the vein in its new location.
• Third type where a vein is removed from its anatomical location and, is connected to an artery and vein in end-to-end fashion.
Both second and third type requires the formation of a tunnel . End-to-end anastomoses are now rarely performed, since the complete disruption of the artery imposes a risk for peripheral ischemia and thrombosis. The most common surgical technique today is the side-to-end anastomosis. However technical problems as cutting the end of the vein in an oblique angle may create functional problems due to stenosis. An anastomosis more proximal in the arterial system should be smaller to prevent steal and limit maximal fistula flow, with the inherent complication of ischemic steal or heart failure . Arteriovenous fistula creation is often performed under local anaesthesia, with low morbidity and requires time for maturation. Data from the Dialysis Outcomes and Practice Patterns Study (DOPPS) indicate that AVFs should mature at least 14 days before use . Fistula size and flow increase over time, of 8-12 weeks and the initial blood flow rates has a range of 200-300 mL/min.
Placement of AVFs should be initiated when the patient reaches CKD stage 4, or within 1 year of the anticipated start of dialysis. A physical examination should document blood pressure differences between the upper extremities and an Allen test should be performed, the lack of a well-developed palmar arch predicts a higher risk for vascular steal symptoms if the dominant artery is used for forearm fistulas creation due to inadequate collateral circulation .
Ultrasound must be done before surgical implantation because it can provide information for maximal surgical success by mapping arteries and veins; eg, a preoperative arterial lumen diameter >2 mm is associated with successful fistula maturation, while a diameter of 600 mL/min, a diameter >0.6 cm with discernible margins, and be at a depth of 0.6 cm (between 0.5 and 1.0 cm) from the surface 6 weeks after creation. In fistulas that are maturing successfully, flow increases rapidly post-surgery, from baseline values of 30-50 mL/min to 200-800 mL/min within 1 week, generally reaching flows >480 mL/min at 8 weeks .The AVFs must be evaluated 4-6 weeks after placement, and experienced examiners (eg, dialysis nurses) can identify non-maturing fistulas with 80% accuracy .
Arteriovenous graft
AVGs were the most commonly used type of dialysis access in the US however, they do not last as long as AVFs and have higher rates of infection and thrombosis . Grafts present a second choice of VA when AVF are not able to be performed because of vascular problems. They can be placed in the forearm, the upper arm, and the thigh, and can have a straight, curved, or loop configuration. They may offer a large surface area for cannulation. AVGs can be cannulated about 2-3 weeks after placement, although there are studies suggesting that immediate assessment after placement for PTFE AVGs is possible . This interval is needed in order to allow the surrounding tissue to adhere to the PTFE conduit, to reduce the postsurgical oedema and the risk for local complications such as perigraft hematoma and seroma .
Tunnelled hemodialysis catheter
TCs are used when AVFs or AVGs aren’t possible to be created for several reasons such as multiple vascular surgeries, that lead to vascular thrombosis or when patients have severe peripheral vascular disease or very low cardiac output. It’s more often in paediatric and very old patients.
Unfortunately they are associated with the highest infection rate and they are not a very long-term access option. Studies have revealed that central venous catheters are colonized within 10 days of placement; however, colonization of the catheter biofilm does not correspond to positive blood cultures or clinical signs of bacteremia . Recently Power A. et al published their experience with 759 TCs. The survival rate at 1,2 and 5 years was 85%, 72% and 48% respectively. The infection rate was 0.34 per 1000 catheter day showing with careful and appropriate use of TCs, they can provide effective and adequate long term hemodialysis and rates of access related infection almost similar to AVGs’ .
Hemodialysis vascular access in children
The choice of replacement therapy in children is variable. The registry of the North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) reports that of patients initiating renal replacement therapy in paediatric centres : one quarter of children underwent preemptive renal transplantation, one half were started on peritoneal dialysis and one quarter were started on hemodialysis. Kidney transplantation remains the preferred therapy for paediatric patients therefore, many paediatric patients receive maintenance HD through an indwelling catheter in perspective of short HD period . In the United States less than 800 paediatric patients receive maintenance HD therapy, therefore surgical experience and clinical data for fistulae or grafts creation in small patients is limited due to rare need for such procedures. Smaller patients, especially those less than 10kg, are very demanding in surgical and nursing skill, this is significant reason the majority of smaller patients receive PD for their maintenance dialysis modality .
Peritoneal dialysis is much more common in infants and younger children , significantly due to problems of vascular access. However, hemodialysis can be performed successfully in infants and very young children, as well . Children who will join in hemodialysis will need evaluation of their vasculature for placement of an arteriovenous (AV) fistula, arteriovenous graft, or cuffed double lumen catheter. The use of an AV fistula, the recommended type of vascular access in adults, is limited in children due to the size of their vessels. In the 2008 NAPRTCS annual report, vascular access for hemodialysis included external percutaneous catheter in 77.7 percent of patients, internal AV fistula in 12.3 percent, and internal and external AV shunt in 7.3 and 0.7 percent, respectively . K/DOQI has encouraged greater use of AV fistulas in larger children receiving hemodialysis who are not likely to receive a transplant within 12 months, with a goal of achieving more effective dialysis with fewer complications (eg, infection) than occurs with catheters. The choice of catheter size and configuration depends on the size of the patient. It is suggested by studies that in children as small as 4 to 5 kg a dual-lumen 8 Fr catheter can be well tolerated, and as the child becomes larger in size, a larger volume access can be placed . Vascular access should be able to provide sufficient blood flow and adequate dialysis with a Kt/V greater than 1.2. Kt/V is influenced further by the recirculation rate. Because flow rates in paediatrics vary by the size of catheter, which varies by the size of the patient, a recommended flow rate of 3 to 5 mL/kg/min is acceptable in most patients .
Vascular access complications and Survival
Studies have shown a mortality risk dependent on access type, with the highest risk associated with central venous dialysis catheters, followed by AVGs and then AVFs . The CHOICE study examined mortality based on access type in 616 hemodialysis patients for up to 3 years of follow-up. Central venous catheters and AVGs were associated with approximately 50% and 26% increased mortality, respectively, compared with AVFs with prevalence in men and elderly patients . Despite these findings and the KDOQI recommendations, dialysis access data from 2002-2003 showed that only 33% of prevalent hemodialysis patients in the US were being dialyzed via AVFs. Contrary in Europe and Canada, the majority of the patients (74% and 53% respectively) were being dialyzed via AVFs .
Vascular access admissions continue to fall, with more procedures now performed in an outpatient setting, and are 45.1 percent below levels noted in 1993. By two-year time period, the adjusted relative risks of all- cause and cardiovascular hospitalization among hemodialysis patients vary little when compared to the reference period of 1997-1998; the risk of hospitalization for infection, however, is now 18 percent greater than in the reference period, while that of a vascular access hospitalization is 30 percent less. Among African American patients, the relative risk of an all-cause hospitalization or one related to infection is almost equal to that of white patients; the risk of a vascular access hospitalization, however, is 24 percent higher. In our previous work with 149 hemodialysis patients who had undergone 202 vascular access procedures (177 Cimino-Brescia fistulae and 25 PTFE grafts we found that the Cimino-Brescia fistula was used as the first choice of vascular access in all patients except one in the elderly group. PTFE grafts were the second or third choice in 7 patients younger than 65 and 15 in the elderly group (p: NS). The only reason for technique failure was vascular thrombosis in both groups (p: NS). Other complications were: aneurysms (10/48 and 14/101, p: NS), infections (0/48 and 2/101 p: NS) and oedema (0/48 and 6/101, p: NS). (Table ….. Five-year technique survival of the first AV fistula in the two groups was 35% and 45% respectively (log-rank test, p: NS). (FIGURE…..) Our findings suggested that there was no difference in vascular access complications across age groups and the survival of the first AV fistula is independent of age.
Other encouraging results include a 22.9 percent fall in dialysis access admissions since 1999 for peritoneal dialysis patients, among hemodialysis patients, admissions for bacteremia/septicemia continue to rise sharply, reaching 112 per 1,000 patient years – similar to the rate of 109 for vascular access infections, and possibly reflecting an increased use of cuffed catheters. In 2010 USRDS Annual Data Report hospitalization in 2008, increased again, to a point 45.8 percent above their 1993 level. In 2007-2008, women treated with hemodialysis were 16 percent more likely to be hospitalized, overall, than male. They also had a greater risk than men of cardiovascular, infectious, and vascular access hospitalizations 11, 14, and 29 percent greater, respectively. Recently unpublished our data are more different than those we published in 1998. We found in 189 patients that female had more possibility to start HD with double lumen catheter than male and also patients with heart failure independent of sex. Female patients had PTEF grafts as first vascular access (p=0,023) and the elderly patients had more complications and more vascular access procedures (p=0.026).
Non-tunnelled double lumen catheters complications
The non-tunnelled double lumen catheters’ complications concern the insertion, the infection and thrombosis of the vessel.
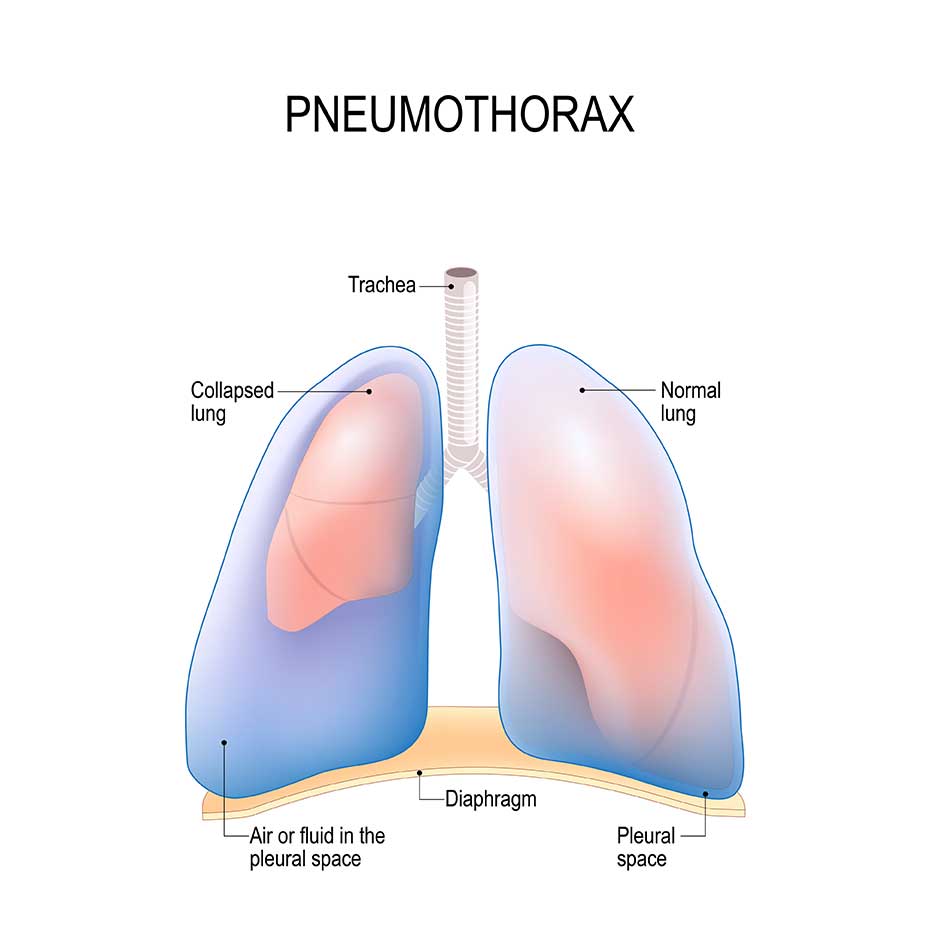
The severity and likelihood of insertion complications varies with the site of insertion. The complication rate and the severity are lowest in the femoral position. The primary problem is perforation of the femoral artery. Bleeding usually resolves within minutes of direct compression. Large femoral or retroperitoneal hematomas occur occasionally . Subclavian insertion complications are potentially more serious. Over-insertion of guide-wire can occasionally lead to atrial or ventricular arrhythmias. The vast majority of these are transient and hemodynamically insignificant . Penetration or cannulation of the subclavian artery can lead to hemothorax, which in some cases requires a thoracotomy tube. Cases of pericardial rupture and tamponade also have been described . Subclavian insertion from the left has an increased risk of atrial perforation which can present with acute hemopericardium upon initiation of dialysis. The incidence of pneumothorax varies from less than 1 percent to more than 10 percent of insertions, depending on the skill and experience of the physician. The risk of pneumothorax is greater from the left than right side, since the pleura and dome of the lung are higher on the left . Due to high rate of catheter-induced subclavian stenosis and subsequent loss of the ipsilateral arm for future hemodialysis access internal jugular vein insertion, particularly the right internal jugular vein is the preferred site of insertion. At internal jugular insertions carry a higher likelihood of carotid artery penetration, but a lower risk of pneumothorax (0.1 percent). Ultrasound guided cannulation of the vessel is recommended to minimize these complications. The location of the catheter tip in subclavian and internal jugular insertion should always be confirmed by fluoroscopy or x-ray prior to the initiation of hemodialysis or the administration of anticoagulants.
Ultrasound-guided catheter insertion is lesser likelihood of arterial puncture or pneumothorax . Prevention and treatment of catheter thrombosis are important clinical issues. To prevent formation of thrombus, both lumens of the double lumen catheter are instilled with heparin following hemodialysis. The amount injected should only fill the catheter lumen to minimize systemic heparinization. Anecdotal evidence suggest that chronic anticoagulation with warfarin or low molecular weight heparin may also prevent catheter thrombus, due to either intraluminal clot or fibrin sheath formation . Lytic agents such as urokinase and alteplase are effective in treatment of catheter thrombosis. Alteplase has effectiveness rates in thrombosis treatment comparable to that observed with urokinase . However if non-cuffed catheters cannot have adequate blood flow then they should be exchanged. Ventral vein catheters are associated with the development of central vein stenosis . This complication appears to occur more often with subclavian (40 to 50 percent of cases in some studies) than with internal jugular insertions (up to 10 percent) . It has been proposed that central venous cannulation creates a nidus of vascular injury and fibrosis. The rapid blood flows associated with the hemodialysis catheter then create turbulence that can accelerate endothelial proliferation, eventually leading to venous stenosis . The K/DOQI guidelines therefore recommend avoiding placement in the subclavian vein, unless no other options are available. If central venous thrombosis is detected early, it responds well to directly applied thrombolytic therapy or to percutaneous transluminal angioplasty when the fibrotic stenosis can be crossed with a guidewire . The infection risks associated with temporary double lumen catheters include local exit site infection and systemic bacteremia, both of which require prompt removal of the catheter and appropriate intravenous antibiotic therapy . Bacteremia generally results from either contamination of the catheter lumen or migration of bacteria from the skin through the entry site, down the hemodialysis catheter into the blood stream . Skin flora, Staphylococcus and Streptococcus species, are responsible for the majority of infections. There is conflicting evidence concerning the risk of infection based upon the site of insertion.
In the largest prospective randomized study, the risk of infection was not reduced with jugular versus femoral venous catheterization . A prospective nonrandomized studies suggest that the infection risk appears to sequentially increase for hemodialysis catheters inserted into the subclavian, internal jugular, and femoral veins, respectively .
Overall, compared with the subclavian vein, the internal jugular vein remains the preferred access site in ambulatory patients because of the high rate of central vein stenosis associated with subclavian vein catheterization (see above). In the Intensive Care Unit, either femoral or internal jugular vein placement is satisfactory, with the use of ultrasound making internal jugular vein placement safer.
The best solution is to prevent the infection by proper placement technique, optimal exit site care and management of the catheter within the HD facility .
Arteriovenous fistulas complications
Complications of AVFs can be divided into early and late causes.
Early causes include inflow problems such as small or atherosclerotic arteries, or juxta-anastomotic stenosis so a pre-operative evaluations for suitable access sites has to been performed .
The aetiology of this acquired lesion is not entirely clear, but may be related to manipulating the free end of the vein, torsion, poor angulation, or loss of the vasa vasorum during anatomic dissection. This lesion often can be adequately treated with angioplasty or by surgical revision . Outflow problems may include accessory veins that divert blood flow from the intended superficial vessel to deeper conduits, or central venous stenosis in patients with prior central venous catheters. Vessels smaller than one-fourth of the fistula diameter are usually not hemodynamically relevant. Juxta-anastomotic stenosis and accessory veins are the most common causes for early failure AVFs when pre-operative evaluations for suitable access sites have been performed .
Late causes for failure of AVFs include venous stenosis, thrombosis, and acquired arterial lesions such as aneurysms or stenosis. Venous stenosis may become apparent as flow decreases over time, worsening weekly Kt/V ([dialyzer clearance
_ time]/body volume) or increasing recirculation. Native fistulas typically will not thrombose until flow is severely diminished. Static pressure measurements, which are helpful in graft monitoring, do not appear as helpful in AVFs, since collaterals surrounding the stenosis area often develop, effectively masking the rise in fistula outflow resistance. Stenotic lesions can be treated by angioplasty. Thrombectomy of fistulas, although technically more challenging than in AVGs, is often successful and if flow is re-established, primary patency is longer than in grafts . Aneurysms may form over the course of years as the fistula increases with increased flow and, unless associated with stenotic lesions, are more a cosmetic than functional concern. If the skin overlying the aneurysm is blanching or atrophic, or if there are signs of ulceration
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "pneumothorax"
Patients can develop a pneumothorax from various means and either (primary or secondary) can occur spontaneously. A primary pneumothorax is reserved for those without any underlying lung pathology, while the term “secondary” pneumothorax is used clinically to indicate patients that carry an established diagnosis of lung disease.
Related Articles