Chris Williams is 20 years old and works in an office in the city. He is a keen runner and is training for the London Marathon. He goes out every morning before work for a 4-6 mile run.
He has no history of cardiovascular or respiratory problems. He is 1.9 m tall and weighs 78 kg. One morning near the end of his run, he has a sudden sharp pain in his right chest and back. The pain is so bad he has to stop his run and limps home, feeling very short of breath.
As the pain and shortness of breath do not go away, he takes a taxi to his local A&E department.
There he is noted to have tachycardia and tachypnoea, with repeated dry coughing. His blood pressure is 110/78 and there are reduced breath sounds in the right chest. He is sent for a chest x-ray which gives a definite diagnosis. He is told he will have to stay in hospital for perhaps a week for observation, and will be given oxygen which should relieve his symptoms.
His condition may resolve spontaneously, but if not, a minor surgical procedure will be necessary.
Approximately 18 men and 6 women in every 100,000 people per year are admitted to hospital with a primary spontaneous pneumothorax. Now, although this may not seem like much there is a 30% chance of recurrence within the first 6 months (Patient.co.uk, 2013) and this is not mentioning the number of cases of patients presenting with secondary pneumothorax. This can be a serious condition affecting people of all ages notably tall thin men in their twenties in the case of a primary pneumothorax and people aged in their sixties in the case of a secondary pneumothorax. (Patient.co.uk, 2013)
What is a Pneumothorax and what are the different classifications
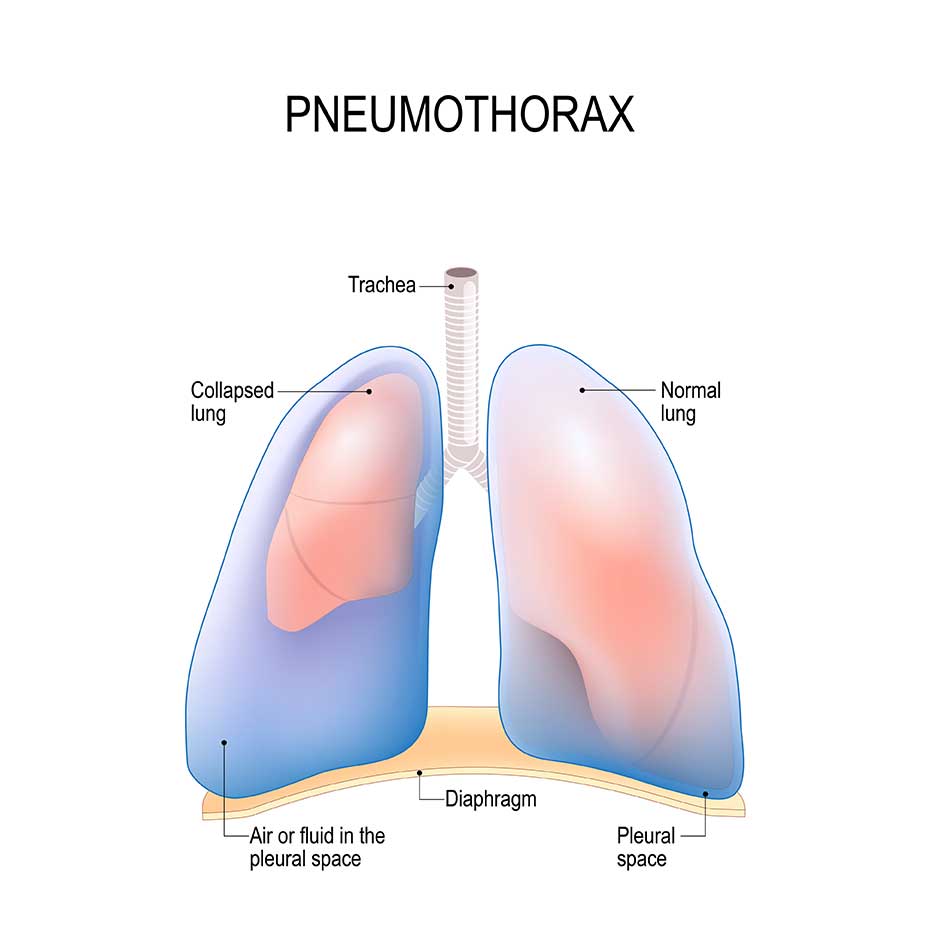
A pneumothorax is defined as the presence of air or gas in the pleural cavity surrounding the lung. The collection of gas increases the pressure outside of the lungs causing it to collapse either partly or completely. (See Figure 1)
https://www.mayoclinic.com/images/image_popup/mcdc7_collapsed_lung.jpg
Figure : An image showing a primary pneumothorax (Clinic, 2013)
There are 3 main classifications of a pneumothorax based on their causes:
Spontaneous Pneumothorax
Primary Spontaneous
Secondary Spontaneous
Traumatic Pneumothorax
Iatrogenic pneumothorax
Non – iatrogenic pneumothorax
Tension Pneumothorax
Primary Spontaneous Pneumothorax
A type of pneumothorax in a person who is otherwise healthy, where there is no known underlying lung disease or trauma. The exact cause of this is unknown however, it is believed that these pneumothoraces occur due to a tiny tear of a bleb on the apical surface of the lung.(Mackenzie and Gray, 2007)
A bleb is a thin walled balloon like extension or air sacs that occur in the visceral pleura surrounding the lungs. (see figure 2) (Martin and Oxford University Press., 2007)
The wall of the bleb is not as strong as normal lung tissue and is thus prone to tearing and allowing air to leak out. However, recent studies have shown that this is not the only cause and that in some cases there is disease of the functional parts of the lungs and increase visceral porosity allowing air to leak out and get trapped between the lung and chest wall.(Mackenzie and Gray, 2007)
You are considered to be at a greater risk of primary spontaneous pneumothorax if you are tall and skinny, as Chris is tall and skinny this may be a reason for his pneumothorax or at least a factor.
http://www.blebinfo.co.uk/media/bleb2.jpg
Figure : A bleb on the apical surface of the left lung (Blebinfo, 2013)
Secondary Spontaneous Pneumothorax
This is a pneumothorax that develops secondary to underlying lung pathology, for example, Patients with COPD are at an increased risk in developing a pneumothorax. (Light, 1993)
There is an increase in risk if the primary pathology weakens the lung walls in some form as this makes it more likely that the wall will tear allowing air to escape from the lung and be trapped between the lungs and the thorax and put pressure on the lung causing it to collapse. (Schiffman, 2012)
Examples of common lung pathology leading to an increase in chance of developing a pneumothorax:
COPD
Asthma
Tuberculosis
Lung Cancer
Pneumonia
As Chris is known to have no cardiovascular or respiratory problems he definitely did not have a secondary spontaneous pneumothorax.
Traumatic Pneumothorax
Traumatic pneumothoraces occur as a result of a blunt or penetrating wound allowing air to enter the pleural space. (e.g. broken rib piercing the lungs or a sharp blade)
An Iatrogenic pneumothorax is secondary to a procedure on the lungs compromising the structure of the lungs and other structures surrounding it, thus making it more prone to tearing. (find a reference)
Tension Pneumothorax
A tension pneumothorax is a life threatening complication that arises when air can enter the pleural space but not escape, due to the formation of a one way flap valve mechanism.
The one way flap valve allows air to enter the pleural space on inspiration but prevents outflow thus creating an increasing positive pressure of air in the pleural space. This increase in pressure will force the lung to collapse and thus push the contents of the mediastinum across impairing venous return to the heart.
Inevitably, hypoxic conditions develop, and can ultimately lead to death relatively quickly. (see figure 3)
This is more likely to occur with a traumatic pneumothorax or an iatrogenic pneumothorax than any other kind. (MedScape, 2013)
http://programs.northlandcollege.edu/biology/ap1forms/ap1casestudies/Critical%20Care%20Case%20Study/Mr%20Jones/tension.gif
Figure 3: A picture showing a tension pneumothorax and how it affects the nearby structures (Snapshots, 2013)
Risk Factors increasing likelihood of pneumothorax
Although we have identified a few of the causes of pneumothoraces above some people are more predisposed to a pneumothorax than others and these are based on a few things:
Sex
Males, who are otherwise probably healthy, tend to be at a greater risk of a pneumothorax (primary spontaneous) than females, the reasons for this are still unclear.
Height
This is thought to be a risk factor as there is a greater pleural pressure gradient in the apex compared to the base thus it experiences far greater distension increase the likelihood of a bleb/ bullae formation. (Mackenzie and Gray, 2007)
Smoking
Emphysema-like changes are thought to occur in the lung walls and there is found to be an increase in the number of blebs/bullae on the surface of the lung wall with increase cigarette smoking, thus increasing the likely chance of rupture and developing a pneumothorax. (Cheng et al., 2009)
Genetics
Some connective tissue disorders can result in the increase chance of developing a pneumothorax (specifically, a secondary spontaneous pneumothorax) such as Marfan’s Syndrome. (MedScape)
Marfan’s syndrome is an inherited dominant genetic disorder of connective tissue with those suffering being abnormally tall, with long limbs. Height as we already know is already a contributing factor to developing a pneumothorax.
Lung disease
If the patient has a previous lung disease (especially those mentioned above, see secondary spontaneous pneumothorax) then there is a highly likely chance of developing a pneumothorax as the walls of the lung are likely to be weakened by the disease and thus it is more likely to cause a tear or develop and rupture a bullae, causing the lung to collapse. (Schiffman, 2012)
Mechanical Ventilation
More likely to cause iatrogenic pneumothorax which is a type of traumatic pneumothorax
Air is pumped into the lungs under a positive pressure; this creates a greater pressure inside the lugs than outside. Once the pressure builds up enough, the air wants to escape and may do this by bursting through the lung wall. (Noppen and De Keukeleire, 2008)
Lung cancer
Having lung cancer and developing a pneumothorax is rarely seen but is a possibility. The exact cause of a pneumothorax from lung cancer still remains unknown. (VenceviÄius and CicÄ-nas, 2009)
Signs and Symptoms of Pneumothorax
Typically people experiencing a pneumothorax of some sort will present with common signs and symptoms such as:
A small pneumothorax can cause:
Sudden sharp pain felt in the affected lung which is worse on inspiration
Shortness of breath
For a larger pneumothorax
Tachycardia – a heart rate of 100bpm or more
Tachypnoea – a breathing rate of 20 breaths a minute or more
Hypercapnia – increase in blood co2 levels
Hypoxia (leading to cyanosis)
A larger pneumothorax may result in one side of the lung collapsing completely resulting in the above symptoms. As the lung is collapsed oxygenation of the blood will have reduced thus there will also be an accumulation in blood CO2 (Hypercapnia). Also as a result of the increase CO2 blood levels there is an increase in breathing rate to prevent acidosis of the blood thus patients may experience tachypnoea. As the lung collapses this puts pressure on the heart and surrounding structures pushing it to the unaffected side, this presses on the vena cava impeding venous return and thus as another negative feedback mechanism, the heart beats faster to accommodate for reduced cardiac output. Eventually, all these symptoms accumulate and then hypoxia is presented which is typically seen with cyanotic skin colour. The symptoms for a large pneumothorax are synonymous with a tension pneumothorax too. [Apps M, 2012]
However, although these symptoms are typical of pneumothorax it is not to say that there may be other lung pathology at action.
Diagnosis of a Pneumothorax
The signs and symptoms for a pneumothorax are very vague and do not allow you to determine whether a pneumothorax is present or if there is some other pathology.
Various imaging techniques and physical examinations can be used to determine whether there is a pneumothorax and its severity.
A Chest Examination
When conducting a physical respiratory examination, when locating the trachea you may find that in patients with a large pneumothorax that the trachea has shifted to the unaffected side, this is due to the collapsed lung pushing it.
Also when percussing the affected lung/ lung area you will hear hyper-resonant sounds indicating a hollow structure – or in this case less hollow structure as the lung is no longer where it should be
Also when auscultating the area you will hear reduced/ no air flow with some possible crackling and this is due to air not being able to enter the lung as it has collapsed and is not inflating. [Yeatman N, 2012]
Medical Imaging Techniques
As a method of confirmation various imaging techniques can be implemented in order to visualise the extent and severity of the pneumothorax.
X-rays
The left lung – collapsed and pressing on the surrounding structures.
Trachea pushed to the righthttp://www.blebinfo.co.uk/media/xray.jpg
Figure 4: A PosterioAnterior X-ray showing a left lung pneumothorax (Masterclass, 2012)
This is the most preferred method of viewing the chest as it is cheap, fast and non-invasive.
A PosterioAnterior radiograph will be used to examine the chest as it allows us to get a fairly true visualisation of the heart, enabling us to determine its size.
The patient must have a full expanded chest (or as fully as can be done) in order for a clear x-ray to be formed.
What you can see in figure 4 above, is that the left lung has completely collapsed and is now pushing on the structures to the right.
The trachea has deviated from central to the unaffected side a sign of a pneumothorax.
The size of the pneumothorax can be determined by measuring the distance from the chest wall to the lung
It is said that an air rim of 2cm is equivalent to 50% of the hemi-thorax. (Masterclass, 2012)
CT Scan (Computed tomography)
Collapsed left lung – pneumothoraxhttp://wikidoc.org/images/5/57/Pneumothorax_CT.jpg
Figure 4: A CT Scan of a left lung pneumothorax (Masterclass, 2012)
A CT scan is much more sensitive to picking up different densities in tissue and thus it can detect even the smallest of pneumothoraces and underlying lung disease, If present.
This can be used when patients are unable to turn and lay on their stomach such as patients in Intensive Treatment Unit. (Masterclass, 2012)
Ultrasound
The fastest method of determining a pneumothorax.
Ultrasound imaging is used commonly for trauma patients who have developed a traumatic pneumothorax.
It can also detect any other lung problems that may exist due to the trauma in emergency situations. (Masterclass, 2012)
Treatment and management of pneumothorax
Treatment of pneumothoraces depend on the size and the underlying cause if there is one. There are 3 main courses of treatment, which include:
Monitor progress
Often the pneumothorax is small enough to just leave and it will heal on its own. All that is required is regular monitoring and x-rays at 2 weekly intervals in order to see the lung has fully re-inflated.
The air that was trapped in the pleural space equalises in pressure with the lungs and may cause the lung to collapse a little. Soon once the tear has healed, the trapped air is slowly absorbed into the blood stream.
Inserting a needle/chest drain
A chest drain is required when the pneumothorax is greater than 20% of the lung volume, if there is no recurrence once the air has been drained then 2 weekly interval x-rays are required to ensure the lung re-inflates fully.
However, if there is recurrence then an intercostal drain placed under the second rib with an underwater seal is required for 2-3 days.
Surgery or pleurodesis
If after 2-3 days the pneumothorax is still present and the underwater tube is still bubbling then surgery is required.
There are 2 options:
Talc Pleurodesis
This is where through a chest drain, talc is introduced to the body causing irritation to the pleura, effectively closing the space between the visceral and parietal pleura such that no further air can be trapped.
This is usually quite apainful procedure so patients are given local anaesthetic and some sort of sedative to prevent them feeling pain during surgery.
Pleurectomy
APPS, Dr M C P. (2012, DECEMBER 7TH). Lung Mechanics [PowerPoint slides]. Presented at a GM1400 lecture at Queen Mary University of London.
BLEBINFO 2013. SPONTANEOUS PNEUMOTHORAX :: View topic – Blebs / Bullae.
CHENG, Y.-L., HUANG, T.-W., LIN, C.-K., LEE, S.-C., TZAO, C., CHEN, J.-C. & CHANG, H. 2009. The impact of smoking in primary spontaneous pneumothorax. The Journal of Thoracic and Cardiovascular Surgery, 192-195.
CLINIC, M. 2013. Mayo Clinic medical information and tools for healthy living – MayoClinic.com.
LIGHT, R. W. 1993. Management of Spontaneous Pneumothorax. American Journal of Respiratory and Critical Care Medicine, 148, 245-248.
MACKENZIE, S. & GRAY, A. 2007. Primary spontaneous pneumothorax: why all the confusion over first-line treatment? 2013.
MARTIN, E. A. & OXFORD UNIVERSITY PRESS. 2007. Concise medical dictionary, Oxford ; New York, Oxford University Press.
MASTERCLASS, R. 2012. Radiology Masterclass – Galleries – Chest X-Ray Galleries – Pneumothorax gallery – Normal reference [Online]. Available: http://radiologymasterclass.co.uk/gallery/chest/pneumothorax/pneumothorax_a.html [Accessed 27/01 2013].
MEDSCAPE. Pneumothorax, Tension and Traumatic [Online]. Available: http://misc.medscape.com/pi/android/medscapeapp/html/A827551-business.html [Accessed 2013 27/01].
MEDSCAPE 2013. Pneumothorax.
NOPPEN, M. & DE KEUKELEIRE, T. 2008. Pneumothorax. Respiration, 76, 121-127.
PATIENT.CO.UK. 2013. Pneumothorax | Doctor | Patient.co.uk [Online]. Available: http://www.patient.co.uk/doctor/pneumothorax [Accessed 26/01 2013].
SCHIFFMAN, G., MD, FCCP. 2012. Pneumothorax (Collapsed Lung) Causes, Symptoms, Treatment – MedicineNet [Online]. Available: http://www.medicinenet.com/pneumothorax/article.htm [Accessed 26/01 2013].
SNAPSHOTS, C. C. N. 2013. Critical Care Nurse Snapshots: Tension Pneumothorax [Online]. Available: http://programs.northlandcollege.edu/biology/ap1forms/ap1casestudies/Critical%20Care%20Case%20Study/Mr%20Jones/tension.htm [Accessed 2013.
VENCEVIÄŒIUS, V. & CICÄ-NAS, S. 2009. Spontaneous pneumothorax as a first sign of pulmonary carcinoma. World Journal of Surgical Oncology, 7, 57.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "pneumothorax"
Patients can develop a pneumothorax from various means and either (primary or secondary) can occur spontaneously. A primary pneumothorax is reserved for those without any underlying lung pathology, while the term “secondary” pneumothorax is used clinically to indicate patients that carry an established diagnosis of lung disease.
Related Articles