Alok Kumar, Lokendra Kumar
Introduction
Cardiopulmonary bypass (CPB) is a straight forward and logical procedure governed by basic physiological principles and reasonable technical practice .It requires fore thought in planning on the part of the perfusionist, as well as alertness, attention and deductive reasoning.
The type of surgery to be performed will dictate what circuit and other equipment will be used. The condition of the patient may also require special preparation. The patient’s chart is reviewed before the case for patient age, weight, history, prior surgery, general physical condition, neurological deficits, carotid insufficiency, blood disorder, pulmonary functions, allergies and other factors that may influence the conduct of perfusion. Lab routine investigation reports are reviewed for hematocrit, platelet count, fibrinogen level, serum creatinine, serum albumin, electrolyte level and the presence of agglutinins. Abnormal finding may influence the pump prime or setup. There are many possibilities. Is blood required in the pump prime? Is the serum albumin low, requiring extra albumin addition, Is an ultrafiltration required? Is patient allergic to drugs usually included in prime? Are anatomic anomalies present requiring special technique?
The bypass circuit, cannulation and prime:–
When assembling the bypass circuit the perfusionist should assure himself that all connections are secure. He should ensure that each piece of tubing which is connected in the circuit is shored up as for as possible on the connector and that all of the locking ridges are engaged. Even though the seal is made on the first distal ridge up the connector. All of the ridges should engaged the tubing .This will help prevent accidental disconnection in that all of the locking ridges collectively prevent the tubing from slipping. For the same reason neither the tubing nor the connector should be moistened prior to engagement
Calculations are performed to determine the necessary blood flow and if blood or other blood product are needed, the pump can then be primed and the sizes of cannula determined. Drug doses in prime can also be determined. The surgeon should be informed of the required cannula size before the cannula pack is opened. In some cases the surgeon may find an unusual condition requiring different sizes of cannula. Sometimes patient’s aorta or any of the chambers or venacava may be smaller than usual or the aorta may be severely calcified.
Records:-
The perfusionist should prepare the perfusion records as completely as possible prior to bypass.The perfusion record should include the following. Name, age, sex, diagnosis, operation planned, weight, height, BSA, blood group. Important investigations, calculated full flows, hypothermic flows, cannulae size required. Hemofilter, ultrafiltrate, urine output, blood added, defibrillator.
1:-Time of starting and stopping bypass
2:-Prime volume
3:-Fluid added during procedure
4:-Drug added to the circuit by the perfusionist
The perfusionist should record the flow rate, arterial blood pressure, gas flow rate, and temperature, regularly at every five to ten minute during bypass or when one of these parameter is changed. At the end of the procedure the perfusionist should place the original copy on the patient chart.
Prebypass check list:-
The prebypass list should include the following:-
- Patient data entered in to pump computer
- Oxygenator holder in right place and secure
- Pump circuit tubing secure without kinks
- Luer connections tight
- Gas line connected
- Gas line not leaking and unobstructed all the way
- Gas supply operational, blenders and vaporizers working
- Gas exhaust cap removed and scavenger line if any obstruction
- Power code secure on both ends
- Backup power available
- Backup light source available
- Hand cranks available
- Water line connected
- Water heater –cooler operable and warming
- Oxygenator check for leaks
- Occlusion set on roller pumps
- Arterial filter primed
- Cardioplegia system primed and at proper temperature
- Drug added to cardioplegia if necessary
- Suckers and vent in proper direction in pump housing
- Pressure transducer calibrated
- Drugs added to prime as required
- Level detector operable
- Temperature probe connected
- Oxygen analyzer calibrated
- Pressure warning turn off device operable
The pump is in the operating room by this time and circulating to ensure proper operation and to remove any air that may be trapped in the oxygenator, filters, or circuit. The water heater –cooler is keeping the prime warm. This keeps the blood warm when going on bypass and prevents cardiac fibrillation from cold priming solution .
Heparin administration:-
The perfusionist should be positive that the patient has been heparinized prior to starting any of the extracorporeal pumps including the suction pumps.
The customary heparinizing dose is 3mg per kg patient body weight of heparin. 3 to 5 minute after heparin has been given and activated clotting time is started to determine adequate anticoagulation. The goal of adequate heparinization is to maintain the patients ACT at 480sec.Sometimes larger dose of heparin may be required to achieve an ACT of 4 times base line value (120×4꞊480sec).This is because of improper storage of heparin, (no cold chain for heparin storage) leading to decreased potency of Heparin, administration of heparin at wrong site, or Heparin resistance. Patient with an antithrombin III deficiency (especially children) may require additional heparin doses. Sometimes it is necessary to give large doses of heparin to achieve the proper anticoagulation status .If the extra heparin does not help the anticoagulation status, it may be necessary to give fresh frozen plasma containing antithrombin III. After 60 to 90 minute of bypass an ACT may be performed at the pump side to determine anticoagulation status. With clotting time below 300sec additional heparin should be administrated depending upon the stage of operative procedure.
Cannulation:-
The cannula is then placed by the surgeon with the help of purse string sutures to hold the cannula and decrease bleeding. A test transfusion through the arterial cannula is performed to ensure proper placement. If the pump arterial line pressure rises greatly during the test transfusion the cannula opening may be occluded by the aortic wall or the cannula, or tubing may be kinked or the arterial cannula may be in the arterial media and not in the aortic lumen. Even worse it may be protruding in to the media which would cause a dissection. Some teams remove blood from the patient via venous cannula after anesthetic induction called autologous blood withdrawing. This temporary removal preserves the platelets and clotting factors that would be lost during bypass for reinfusion at the end of the bypass period. This blood has the advantage of having platelets, clotting factors and RBC. The disadvantage is that the hematocrit of the patient drops for the bypass run.
Bypass initiation:-
The initiation of bypass begins after the surgeon has instructed the perfusionist to initiate (start) or go on bypass. The perfusionist should repeat this instruction loudly, enough for everyone to hear. This is a good safety measure to ensure that the perfusionist has heard the surgeon correctly and that the surgeon is indeed ready for bypass to begin. Accidents have occurred when perfusionist have thought they heard the surgeon tell them to go on bypass when in fact they had not.
The anesthesiologist stops the ventilation after bypass is initiated. A practical routine of going on bypass should be used to initiate bypass. This routine may be unique to the institution or the perfusionist. The repetition of following this pattern is an obvious safety asset. The oxygen flow is started and the arterial clamp removed. The pump flow is begun slowly, while observing the arterial line pressure to make sure there is no obstruction of the arterial line and that the cannula is functioning properly. If the arterial line pressure suddenly rises there may be several causes. Terminate bypass and systemically review possible causes.
Causes of high aortic line pressure:-
- Kink in arterial cannula or line
- Cannula improperly positioned
- Clamp too near the cannula ( this will occur when aortic cross clamp is applied )
- Cannula too small
- Arterial systemic blood pressure is very high
- Aortic dissection
- Blockage in arterial filter
The venous clamp or occluder is opened and venous return is checked. Flow is slowly increased to a cardiac index of 2.4L/min/m2. Poor venous return prohibits the establishment of adequate bypass. Is impossible to maintain adequate flow if the venous return does not equal to arterial blood flow. This problem should be dealt with early in the case. The problem can be assessed systematically and corrected.
Causes of poor venous return:-
- Kink in the venous line or cannula
- Air lock in venous line or cannula
- Oxygenator or venous reservoir is not positioned low enough (as venous return is gravity dependent)
- Non cardiac suction (wall suction) being used instead of pump suckers, wasting blood.
- Fluid rapidly moving to interstitial area due to decreased intravascular COP (this takes time).
- Venous cannula placed too far down or up and vena cava not draining
- Vent or cardioplegia line open by mistake (inadvertently).
- Bleeding due to accidental laceration or puncture in back of heart
- Bleeding due to other causes such as internal bleeding, or open saphenous vein, or central venous cannula or arterial connecter of peripheral artery.
- Occasionally the venous line may “Chatter” due to excessive negative pressure causing a suction effect. The easy way to correct this is to place a clamp on the venous line that partially occludes the return. If the pump has a built in venous occluder this could of course, be slightly closed.
Checks list after bypass is initiated:-
Immediately after bypass is established and full flow established, standard operating procedures are reviewed. This review ensures that some aspects of perfusion are not being overlooked. Some perfusionists use a written checklist for this stage also. These checks should be repeated mentally every few minutes if possible.
On bypass safety checks:-
- Blood flows are at proper rate, for the age of patient, core temperature.
- Arterial line pressure is normal
- Oxygen started at proper flow and FiO2.
- Oxygen saturation normal
- Patient’s arterial pressure should be 50 to 90 mmHg for adult patients and 30 to 50 mmHg for pediatric patients.
- Temperature appropriate to surgical requirement.
- Coagulation status acceptable
- Acid base management
- Check the safety devices and other function as required should be done at least once
- Bubble detector on
- Level detector on
- Manifolds in right position
- Drugs given as required
- Oxygen analyzer on
Management of cardiopulmonary bypass:-
- Monitoring
- Hypotension
- Temperature
- Renal function on bypass
- Crass clamp periods
- Cardioplegia Administration
- Venting
- Fluid Management
Suckers and vents
The suckers attached to the CPB circuit allow blood to be salvaged from the operative field to be returned to the circuit via the reservoir.
Vent catheters are for direct and indirect venting of the left ventricle and feature perforated tips. A choice of either PVC or silicone is available along with straight and malleable bodies with depth marking. Vents are available in pediatrics and adult size. Straight body models are available with a malleable or stiff guide-wire style introducer for easy insertion and placement.
Vent catheters terminate with a air vented or non-vented round tip.
“Vent” suckers are specifically used to drain blood that has not been directly removed from the heart by the venous cannulae. The most common sites for placing dedicated vents are (Figure 1 and 2):
• The aortic root.
• The left ventricle.
• The right superior pulmonary vein.
• The left ventricular apex; and
• The left atrium or pulmonary artery.
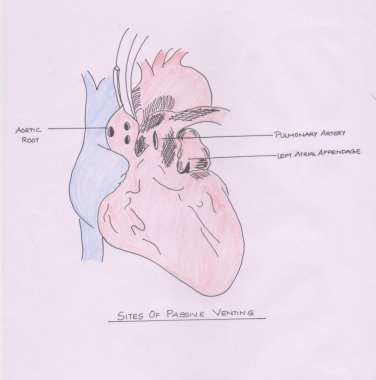
Figure 1.
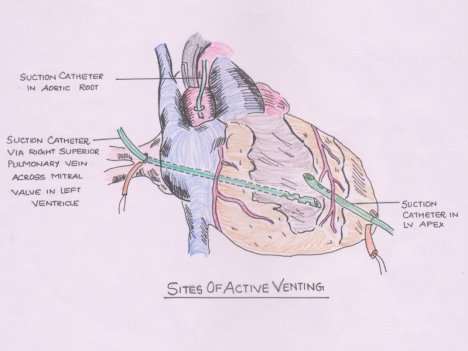
Figure 2.
There are a number of reasons for venting the heart during CPB:
• To prevent distension of the heart.
• To reduce myocardial re-warming.
• To evacuate air from the cardiac chambers during the de-airing phase of the procedure;
• To improve surgical exposure; and
• To create a dry surgical field, especially during the distal coronary anastomosis phase of
CABG surgery.
There are complications associated with all sites used for venting, most commonly relating
to injury to tissues at the site. Venting via the left ventricular (LV) apex, however, is associated with particularly serious consequences including:
• Damage to the LV wall due to excessive suction;
• LV wall rupture if inadequately closed at the end of the bypass period; and
• Embolization through air entrained into the LV.
Active venting with high levels of suction can lead to air being introduced into the arterial side of the CPB circuit due to a small percentage of air sucked into the venous side of the reservoir and oxygenator passing through the circuit into the arterial side. Therefore, suction pressure and duration should be kept to a minimum.
Termination of bypass:-
- The first step in terminating bypass is to ensure that all patient related surgical issues, ABG, contractility of heart and other factors are satisfactory. The ECG should be acceptable and the pacemaker placed if required
- The hematocrit should be in acceptable range
- The potassium should be in normal range (3.5 to 5.5 mEq/L).
- Temperature status
– The termination begins with gradual clamping of venous line while arterial flow is decreased
– The Anesthesiologist starts ventilation.
– The pulmonary artery diastolic pressure or PCWP is the indicator of the volume level of the patients
– The arterial pressure waveform status show the effect of the heart ejecting the volume. The arterial systolic pressure should rise to an acceptable level of at least 90 to 100 mmHg. The pump is then completely stopped as the venous line totally clamped.
– Salvaging remaining blood.
Suggested reading
- Reed CC, Kurusz M, Lawrence AE Jr.Safety and techniques in perfusion. Stafford, TX: Quali-Med, 1988:23.
- Davis RF, Dobbs JL, Casson H. Conduct and monitoring of cardiopulmonary bypass. In: Gravlee GP , Davis RF , Utley JR , eds.Cardiopulmonary bypass, principles and practiceBaltimore: Williams & Wilkins, 1993:579.
- Hessel EA. Cardiopulmonary bypass circuitry and cannulation techniques. In: Gravlee GP, Davis RF, Utley JR , eds.Cardiopulmonary bypass, principles and practice. Baltimore: Williams & Wilkins, 1993:55–92
- Magilligan DJ, Oyama C. Ultrafiltration during cardiopulmonary bypass: laboratory evaluation and initial clinical experience.Ann Thorac Surg1984; 37:33–39.
Cite This Work
To export a reference to this article please select a referencing style below:

