Well I would like to describe the prevalence and research about the topic in brief in this part as it is important to know why this topic has become an issue now and why do we need to make research on it.
Plantar fasciitis is found to be the common foot complaint. It has been estimated that it affects approximately one in ten people at some time in their life (Crawford, Atkins, Edwards, 2003). However, it can occur at any age. It is twice as common in women as men and it is also common in athletes (NHS Clinical knowledge, 2009). The most common cause is infracalcaneal pain of plantar fasciitis and accounts for 11% to 15% of all foot complaints that require professional treatment (Buchbinder, 2004). A recent survey done by Riddle and Schappert in (2004) estimated that there are approximately one million patient visits per year to office-based physians and hospital departments in the United States by patients diagnosed as having plantar fasciitis. It occurs in approximately 10% of people who run regularly. Incidence of this condition peaks between the ages of 40 and 60 years (Buchbinder, 2004; Wearing , Smeathers , Urry et al., 2006). It is a bilateral complaint in about one third of patients (Buchbinder, 2004 ). Podiatric physicians, rheumatologists, general practitioners, physiotherapists and orthopaedic surgeons are the main healthcare providers involved in the treatment of plantar fasciitis (Riddle & Schappert, 2004; Crawford and Thomson, 2003; Atkins et al., 1999). As I have been working as a musculoskeletal physiotherapist this topic quite influences me as most of the patient which i have been looking suffer from this injury. So in this systematic review i would be discussing about effectiveness of low-dye taping technique in plantar fasciitis. Plantar fasciitis is not gender specific and affects approximately 2 million of the American population per year (Irving , Cook and Menz, 2006). This disorder is expected to have many factors in origin such as obesity, excessive periods of weightbearing activity and decreased ankle range of motion commonly suggested to be involved (Riddle, Pulisic, Pidcoe, Johnson 2003). A wide diversity of treatment strategies have been developed. Up to 90% of patients treated conservatively (eg taping and ultrasound), they experienced resolutions of symptoms (Thomas et al., 2001; Gill, 1997). There limited support of evidence showing specific treatment strategies for plantar fasciitis (Crawford and Thomson, 2003; Gill, 1997; McPoil et al., 2008). Atkins et al. (1999) identified 28 different conservative treatments and eight different surgical treatments, which confirms the vagueness of this condition. Foot orthoses are a common treatment for plantar heel pain, however due to the manufacturing process, they often require a time of a few weeks between the initial consultation and issuing the devices (Kosmahl, 1987; Lynch et al., 1998; Martin et al., 2001; Scherer, 1991). As such, short-term treatments such as supportive taping are used to improve symptoms during this temporary period (Martin JE, Hosch, Goforth, Murff, Lynch, Odom 2001) – the low-Dye (Dye 1939) taping technique being one of the most frequently used. Foot taping, such as low-dye taping, alters the mechanical function of the foot, decreasing stress on the plantar fascia and subsequently producing symptom relief (Saxelby, Betts, Bygrave 1997). Low-Dye taping by Dye in (1939) is a common conservative treatment for plantar fasciitis. Most research (Ator et al., 1991; Childs et al., 1996; Del et al., 2004; Harradine, Jarrett, 2001; Holmes, Wilcox, Fletcher, 2002; Keenan, Tanner, 2001; Moss, Gorton, Deters, 1993; Russo, Chipchase, 2001; Scranton, Pedangana, Whitesal, 1982; Vicenzino et al., 1997; Whitaker, Augustus, Ishi, 2003) to date has examined the mechanical effects of the tape on the lower limb.
One of the study done by Saxelby et al. in 1997 has evaluated the symptom relief offered by low-dye taping, but it had small numbers of participants and did not include a control group. But consequently there is need for larger studies that use a control group for comparison so we need to carry out this study. Those tapings which extended up the leg were known as ‘High-Dye’, while those in the foot were named ‘Low-Dye’. It has been used in the management of an array of foot pathologies, especially plantar fasciitis, and its effectiveness has been discussed by several workers (Newell1977, Miller 1977, Subotnick 1975, Van Pelt 1989). Taping as an intervention or as part of an intervention for the treatment of plantar fasciitis has been used for at least 70 years (Dye 1939). A systematic review assessing the efficacy of low-dye treatment strategy has not been found. Therefore, it was considered relevant to conduct the review. The discussion about the basic information regarding the topic in detail and why it is an issue now will be discussed in the following chapter. Well the basic aim of this review is asking whether low-dye taping is effective in the management of plantar fasciitis or not?
The purpose of this study is to give low-dye taping treatment to people suffering from plantar fasciitis with respect to pain relief, gait improvement, impact on lifestyle and overall rate of success. The systematic review helps to identify the papers which relate to the question asked by the review and in turn will help to answer the review question. A organised SR protocol should be developed to carry the review in a easy way. The systematic review should be carried out in an organised manner as follows:
Background:
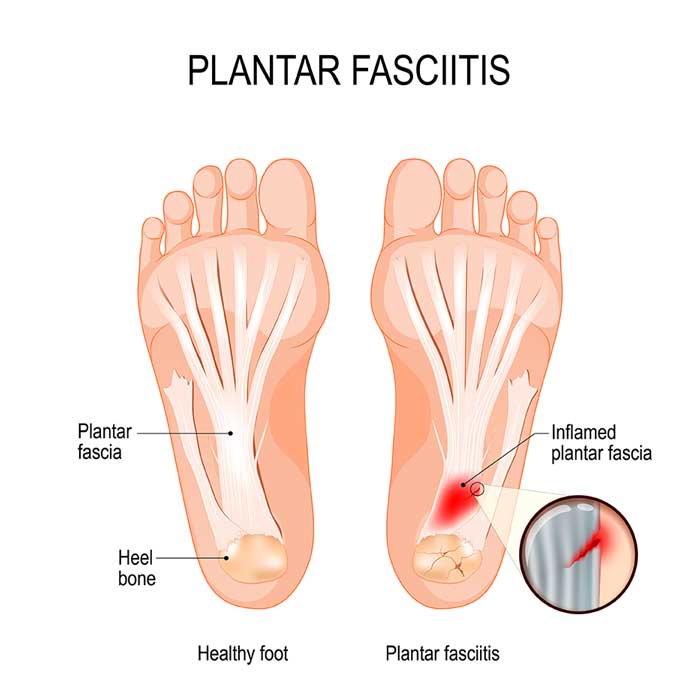
Intially i would like to discuss about plantar fascia, its situation and what structures it covers and how it causes injury.
According to Haung 1993, the plantar fascia is the major arrangement that supports and maintains the arched position of the foot. This aponeurosis acts as a “bowstring” to grip up the longitudinal arch. It covers the major part of the foot. The planter fascia is a fat, fibrous group of connective tissue. Its starting point is the medial plantar tubercle of the calcaneum. It extends along the length of the sole of the foot like a fan, being attached at its other end to the bottom of each of the toes. It is a tough, flexible structure that has a number of significant functions during running and walking. It stabilizes the metatarsal joints during impact with the ground. It behaves as a shock absorber for the whole leg. It forms the longitudinal arch of the foot and helps to raise the arch to get ready for the ‘take-off’ phase of the gait cycle. The plantar fascia helps to preserve the complex arch system of the foot and plays role in one’s equilibrium and the various phases of gait. The plantar fascia consists of a multilayered fibrous aponeurosis (Kwong, Kay, Voner, & White, 1988) that starts from the medial tubercle of the calcaneus .The plantar fascia is made of three major bands, the lateral, central, and medial. The central band is the strongest and thickest. The medial and lateral bands cover the undersurface of the abductor hallucis and abductor digiti minimi muscles, respectively. The fibers of the central band separate into 5 slips near the level of the metatarsal heads and then attach to the proximal phalanx via the plantar plate of each metatarsophalangeal joint (Schepsis, Leach, & Gorzyca, 1991).
Figure 1
Now we will discuss about plantar fasciitis. Here are some acceptable definitions of plantar fasciitis cited by experts which would be helpful in this study.
Injury of this tissue, called as a plantar fasciitis, is very difficult to resolve. Plantar fasciitis is a localized inflammatory condition of the plantar aponeurosis of the foot and is reported to be the most common cause of inferior heel pain (Schepsis, Leach, & Gorzyca, 1991). Plantar fasciitis represents the fourth most common injury to the lower limb and represent 8 – 10% of all presenting injuries to sports clinics. It can be caused by many factors. Plantar fasciitis develops when repetitive weight-bearing stress irritates and inflames the tough connective tissues along the base of the foot. It is difficult to treat. Rehabilitation can be long and frustrating process. The use of preventing exercise and early acknowledgment of danger signals are considerable in the avoidance of this injury. Plantar fasciitis refers to an inflammation of the plantar fascia. The inflammation in the tissue results in some type of injury to the plantar fascia. Typically plantar fasciitis ults from repeated trauma to the tissue where it attaches to the calcaneus. According to souza, plantar fasciitis presents as a sharp heel pain that radiates next to the bottom of inside of the foot. In short the definition varies from person to person and it mainly depends upon the cause. The pain is found to be terrible when getting out of bed in the morning. Plantar fasciitis is a aching condition of the subcalcaneal aspect of the foot resulting from soreness or contracture of the deep fascia of the sole with or without calcaneal spur. Plantar fasciitis has been used synonymously with the following terms:
Painful heel syndrome
Subcalcaneal bursitis
Subcalcaneal pain
Runner’s heel
Medial arch sprain
According to Baxter, Plantar fasciitis can take place in runners or other athletes who repetitively land on the foot. Plantar fasciitis is an overuse damage whose occurrence accounts for 10% of all running injuries (Am J Sports Med 1991). Another vulnerable group is middle-aged people who use up much time on their feet. More infrequently, the fascia becomes irritated after a single traumatic episode, such as landing incorrectly after a jump or running a long hill. The massive majority of people will respond to conservative care and not require surgery. Appropriate treatment is necessary, however, to permit continuous participation in sports and daily activities, and to stay away from chronic damage.
Risk factors:
Plantar fasciitis is particularly prevalent in runners and people who are overweight (Hill and Cutting, 1989), however, it is also prevalent in people with systemic, inflammatory arthritis (Davis and Blair, 1950; Hassani et al., 2002; Furey, 1975; Gerster, 1980). Despite plantar fasciitis being a relatively common disorder, little is known about its etiology and pathogenesis (Wearing et al., 2006). Most anecdotally (Singh et al., 1997; Irving, Cook and Menz, 2006; Rome, 1997), intrinsic and extrinsic risk factors for plantar fasciitis have been reported. Participants in sports that engage some degree of running and jumping, e.g. basketball, tennis, step-aerobics, dancing may be at risk. Non-athletic people who spend much time on their feet. It may emerge in someone who suddenly becomes more active after a time of relative inactivity. Running on hard ground aggravates the risk, as does an increase in hill training. Worn out trainers boost risk as they lose their shock absorption properties. Obesity increases risk. There is increase in stress placed through the fascia. Other mechanical risk factors include flat feet (pes planus) and having a high arch (pes cavus). Studies done by (Riddle et al., 2003; Irving et al., 2007) identified that reduced talocrural dorsiflexion, high body mass index, pronated foot posture, and prolonged work related weightbearing are independent risk factors of plantar fasciitis. The most widely reported clinical sign of plantar fasciitis as said by Wearing et al., (2006) is pain localised to the medial tubercle of the calcaneus. Characteristically, the pain is exacerbated after periods of nonweightbearing. The pain decreases after few minutes of initial weightbearing but returns and get worst when time on feet increases (Singh et al., 1997; Thomas et al., 2001; Schepsis, Leach and Gorzyca, 1991).
Various interventions used for plantar fasciitis:
In general, plantar fasciitis is a self-limiting condition. Unfortunately, the period until resolution is frequently six to 18 months, which can direct to frustration for patients and physicians. Rest was cited by 25 percent of patients with plantar fasciitis in one study as the treatment that worked best (Wolgin, Cook, Mauldin, Graham 1994). It is equally important to correct the troubles that place individuals at risk for plantar fasciitis, such as increased amount of weight-bearing activity, increased intensity of movement, hard walking/running surfaces and worn shoes. Early recognition and treatment usually direct to a shorter course of treatment as well as improved probability of success with conservative treatment measures (Martin, Irrgang, Conti 1998, Reid 1992).
Various treatment strategies, including orthoses (Kwong et al. 1988, Gross et al. 1984, Goulet et al. 2002, Lynch et al. 1988), stretching (Probe et al. 1999, Powell et al. 1998, DiGiovanni et al. 2003, Chandler et al. 1993, Barry et al. 2002), taping (Lynch et al. 1988, Scranton et al. 1982), extracorporeal shock wave therapy (Boddeker et al. 2001, Buchbinder et al. 2002), laser therapy (Basford et al. 1998) and drug therapy in the appearance of systemic medication (Probe et al. 1999), percutaneous injection (Cunnane et al. 1996, Kamel et al. 2000, Kane et al. 1998) and topical application (Gudeman et al. 1997, Japour et al. 1999) have been investigated and have revealed variable clinical benefit.
In the recovery phase of rehabilitation, the objective is to decrease stress on the plantar fascia (J M.). Orthotic shoe inserts are thought to give stress relief and hold the plantar fascia, but a review of several studies found them to be unconvincing and contradictory due to methodology, small study size, or lack of long-term follow-up. There are many conservative treatments which can give better relief such as:
Icing: Ice massage for over 15 minutes for three times a day can give better results and decrease the inflammation.
Stretching
Heel lifts
Supportive shoes
Weight loss
Taping
Orthotics: Devices such as rubber heel cups, elastic heel inserts can provide relief for plantar fasciitis.
Night splints: Splints can provide relieve from plantar fasciitis, but it usually takes more than 12 weeks.
Taping: The purpose of taping the foot is to change the mechanical load toward the fascial enthesis. Several studies done by Lange, Chipchase, Evans, (2004); Vicenzino et al., 2005; Radford et al., 2006) have reported that antipronation tape change the longitudinal arch height and decrease pressure in the heel which are clinically relevant in patients with plantar fasciitis.
Taping can be done in many methods but i am more interested in low-dye taping as it is widely used and so i will be discussing about that technique in detail.
LOW-DYE TAPING:
Low-dye taping is an orthopaedic/sports adhesive strapping technique first described by Dye (1939) and later modified by a number of authors (Boergers, 2000; Del et al., 2004; Lange, Chipchase, Evans, 2004; Russo, Chipchase, 2001). Low-Dye taping is designed to off-load the plantar fascia. It is a short term treatment and its off-loading effects vary from patient to patient. However, as a general rule leave the tape on for a maximum of 3 days, but some might find it needs to be replaced more frequently in order remain effective. If at anytime the tape is uncomfortable, irritates, causes itching or pins and needles it should be removed immediately. The taping aims to limit foot pronation and is used in the short-term to reduce the symptoms of disorders thought to be related to excessive foot pronation which includes plantar fasciitis, tibialis posterior dysfunction, and patellofemoral syndrome (Schulthies, Draper, 1995; Whitesel, Newell, 1980).
The taping required is a 1 inch zinc oxide (rigid strapping), most chemist should stock it. Another place to access it is from www.simplyfeet.co.uk, look under strapping and for Leukoplast (2.5cm), its costs approximately £2.70p per roll (which should last for 3-4 applications)
How to apply the taping
1. The first taping is applied down the outer and inner border of the foot, repeat 3-4 times. Apply enough tension to avoid the tape wrinkling, it needs to be no tighter.
2. The second taping is applied across the underside of the foot-starting level with the ankle, apply the tape across the foot from the outside to the inside. Over lap the each strap slightly and keep going until just before reaching the ball of the foot.
3. The final taping is a securing tape-apply a piece of tape across the midfoot, at about where the second taping ends, apply across the top of the foot, but do not encircle the whole foot, as this will be too tight.
4. Initially the tape will feel slightly tight, but this should ease, if it feels uncomfortable at all-remove immediately.
Effects of Low-Dye taping:
Offers support for the medial longitudinal arch and reduces pronation (inward rolling of the foot).
Can be used for any condition affected by excessive pronation – Plantar fasciitis, Tibialis Posterior Tendonopathy/Dysfunction, Sinus tarsi syndrome.
Limitation of taping: One restriction of long term taping is that there is danger for skin breakdown. So therefore it may be considered only as a short term management option.
Literature review:
For writing the literature review, the following databases and books were searched. There was a detailed search on internet which gave a lot of information about plantar fasciitis. Some information was gathered from books and journals as well. Some of the journals were available online while rest of them had to be purchased from library. Some of the books were available online as well.
The following databases had been searched for writing this literature review:
Medline
AMED
CINAHL
ClinPSYC
EMBASE
PsycINFO
PEDRO.
The following information was gathered from all the sources taking account of the review question.
The proximal insertional disorder of the plantar fascia is best known as plantar fasciitis and as per Lemont, Ammirati and Usen in (2003), histopathologic research has found no signs of inflammation but has reported degenerative changes in the plantar fascia. The prevalence of plantar fasciitis has not been studied (Riddle & Scappert 2004), but it is estimated that it affects 10 percent of the general population at some time during life (Demaio et al., 1993).
PF is considered a self-limiting condition, however, the typical resolution time is anywhere from 6-18 months, sometimes longer (Young, Rutherford, Niedfeldt 2001) which can lead to frustration on both that is the physician and patient. Most experts agree that early recognition and treatment of PF leads to a shorter course of treatment and greater probability of success with conservative therapies (Singh, Angel, Bcntk, Trevino 1997). Of the many treatment options available for PF, one of the most effective is also the most fundamental – rest and avoidance of aggravating activity provides significant relief. One study cited rest as the treatment that worked best for 25percent of PF patients (Wolgin, Cook, Graham, Mauldin, 1994). Martin et al. 2001 compared custom orthoses, over-the-counter arch supports, and tension night splints in the management of plantar fasciitis. Lynch et al. compared anti-inflammatory therapy, accommodative therapy and mechanical therapy in the management of plantar fasciitis. There are several conservative treatments that are employed to manage this condition. Scientists at the University of Bridgeport Chiropractic College in Calgary, Alberta, conducted an comprehensive review of the literature from 1980 to March 2005 on the management of plantar fasciitis. They concluded that due to numerous methodological flaws, none of the 15 randomised controlled trials showed finally which conservative treatment modality was best for plantar fasciitis (JCCA, 2006). Contrast baths’, in which the application of cold and heat to a wounded area is alternated, are widely believed to reduce oedema (tissue swelling) and relieve uneasiness following an injury (Sullivan and Anderson 2000). A hunt of the scientific literature on this topic using Medline uncovered just two articles in this area, and one of the articles was unreliable in nature, with no rigorous, controlled testing of the efficacy of contrast baths. The other journal article listed research carried out at the University of North Carolina in which 30 subjects with post-acute sprained ankles were assigned to either a cold (n = 10), heat (n = 10), or contrast-bath (n = 10) treatment group (‘Comparison of Three Treatment Procedures for Minimizing Ankle Sprain Swelling’, Physical Therapy, Vol 68 (7), pp1072-1076, 1988). Volumetric measurements of the subjects’ ankles were completed in a specially constructed tank, prior to and after treatment. An increase in the measure of oedema was actually observed with all three treatments, but cold application was connected with the least measure of swelling; contrast baths were no better than the direct application of heat when it came to controlling swelling. This study is somewhat faulty, since there were no control individuals with whom the persons utilizing a variety of treatments could be compared. Nonetheless, the research suggests that there is nothing particularly beneficial about contrast baths (especially when compared with the application of nothing but cold) in the management of sprained ankles or oedema in common. Interestingly enough, there also does not show to be a single study in the scientific literature involving contrast baths with quicker recovery from injury or with a considerable decrease in pain associated with an injury. Compression is thought to be valuable in this phase through taping of the foot (Anderson 2000).
Scherer and the Biomechanics Graduate Research Group in 1998 performed a prospective study in which they treated 73 patients with 118 painful heels with taping, nonsteriodal anti-inflammatory drugs, injections, and rigid orthoses (98% received these orthoses). The study showed that, within 6 weeks, approximately 84% of the patients had at least 80% relief of symptoms. This study also identified a subgroup of 43 heels (27patients) that received only mechanical therapy with taping or orthoses. Of this group, 90% had more than 80% relief of symptoms. The author concluded that mechanical control of midtarsal joint was the most successful treatment modality for plantar fasciitis. In an attempt to measure the effects of ‘Low-Dye’ taping on the foot, eight patients (nine feet) with plantar fasciitis were studied using the pedobarograph to investigate changes in gait patterns. In addition, patients completed a questionnaire to assess symptom improvement. Significant changes between the untaped and taped foot were found in respect of pressure levels, areas under the pressure time curves and temporal parameters. The questionnaire revealed subjective improvements in symptoms in eight out of the nine feet studied (Saxelby, Betts and Bygrave 2004). The results from this nonrandomised trial indicate that this technique may be helpful for pain associated with plantar fasciitis. This article reveals that taping technique can improve gait to some extent.
The best method to avoid plantar fasciitis is to minimise your risk factors. Follow the guidelines outlined above for selecting suitable and well-constructed shoes. Progress training schedules properly and works in new environments gradually. Keep your calf muscles physically powerful. Although plantar fasciitis is a prevalent problem, little scientific evidence exists concerning the most appropriate intervention (Crawford, Atkins, Edwards 2002 ).
In the book by Rose Macdonald (2009), named “Pocketbook of Taping Techniques By Rose Macdonald”, Functional taping is now acknowledged as a skill which is essential for those concerned in the treatment and rehabilitation of sports injuries and many other conditions such as muscle imbalances, unstable joints and neural control. It incorporates all the basic techniques essential to the practice of good taping but also includes chapters on new evidence-based procedures written by experts from around the world. To assist in the development of these techniques, this pocketbook demonstrates many new methods which may be used as indicated or customized to suit the clinical situation. The Key Features in the book are
Structured by body region with highly-illustrated descriptions of significant taping techniques
Covers all aspects of functional taping
New techniques to modify muscle activity and proprioception based on scientific evidence.
Handy, portable size for simple reference in the field.
Well there are few papers (Saxelby et al., 1997; Radford et al., 2006; Osborne and Allison, 2006; Landorf et al., 2005) published in the journals which say that low-dye taping has been effective in the management of plantar fasciitis. We will discuss about the papers in detail in the later part of the review. A systematic review conducted by Radford et al., in (2006) of randomised controlled trials examined the result of low-dye taping on biomechanical variables. According to Kogler et al. (1999), the supportive tape reduces the symptoms of plantar heel pain by reducing strain in the plantar fascia during standing and ambulation.
A study conducted by Nolan and Kennedy in 2009 aimed to determine the special effects of Low-Dye taping on peak plantar pressure immediately post-application and found that Low-Dye tape’s initially reduced lateral forefoot peak plantar pressure after a 10-minute walk. However, the tape continued to have an effect on the medial forefoot after 20 minutes of exercise.
Chapter 2:
Now we will be discussing about the systematic review methodology in this chapter
The basis for a systematic review:
According to Altmann (1999), Systematic reviews, in healthcare, have been described as providing objective overviews of all the evidence currently available on a particular topic of interest. Such overviews cover clinical trials in order to establish where effects of healthcare are consistent and where they may vary. This is achieved through the use of explicit, systematic methods aimed at limiting systematic error (bias) and reducing the chance of effect (Higgins and Green 2006). So systematic review are useful to decide which treatment in health care is more effective.
Methodology:
Systematic literature reviews are a method of making sense of large bodies of information, and a means of contributing to the answers to questions about what works and what does not- and many other types of question too (Petticrew and Roberts 2006). They are a method of mapping out areas of uncertainty, and identifying where little or no relevant research has been done, but where new studies are needed. Systematic reviews are literature reviews that remain closely to a set of scientific methods that explicitly aim to limit systematic error (bias), mainly by attempting to identify, appraise and synthesize all relevant studies in order to answer a particular question.
Definition of systematic review: A review that strives to comprehensive identify, appraise, and synthesize all the significant studies on a specified topic. Systematic reviews are often used to test just a single hypothesis, or a series of related hypotheses (Petticrew and Roberts 2006).
Systematic reviews provide information about the effectiveness of interventions by identifying, appraising, and summarising the results of otherwise unmanageable quantities of research (Light and Pillemer 1984, Mulrow 1994). A review of the evidence on a obviously formulated question that uses systematic and explicit methods to identify, select and critically appraise relevant primary research, and to remove and analyse data from the studies that are incorporated in the review. Statistical methods (meta-analysis) may or may not be used.
Systematic reviews are defined, according to the Cochrane collaboration, as scientific literature reviews aimed at answering clearly formulated questions by use of systematic and explicit methods for identifying, selecting, and critically appraising relevant research, and for collecting and analysing data from the literature included in the review (The Cochrane collaboration.
During a systematic review, meta-analysis may be used as a statistical tool for analysing and summarising the results of the included studies (Green and Higgins 2005). In order to fulfil this function, a systematic review should: (i) present a synthesis of the acquired knowledge regarding one particular clinical question derived from all relevant studies that are identifiable at one point in time, (ii) identify the level of internal validity and the subsequent potential systematic error risk associated with the acquired knowledge and (iii) provide recommendations for improving any identified shortcoming related to internal validity, for further research. Owing to continued further research, systematic reviews should also provide continued updates of their synthesis.
Why do a systematic review? A rationale:
Single studies can usefully be seen as similar to single respondents in a survey. The results from one respondent may say something, and sometimes something very important, but one might well get the opposite answer from the next respondent. It is more likely that one will learn more by examining data from other respondents, by looking at the range of answers and examining why those answers vary, and by attempting to summarize them (Petticrew and Roberts 2006). Literature reviews are also, in essence surveys, and it is worth remembering that they share very similar biases with other forms of social surveys.
History of systematic review:
From the 1930s onwards, and possibly even before, the specific term “systematic review” was being used to refer to literature reviews (Petticrew and Roberts 2006). In short, contrary to what is commonly supposed, neither the term “systematic review” nor the general approach of systematic literature reviewing is particularly new, nor particularly biomedical. Many systematic reviews involve a statistical pooling of the findings of the primary studies. This approach, meta-analysis, probably derives in its current form from Glass and Smith’s work, which began in the late 1970s (Glass and Smith 1978).
Systematic Review Process:
Scoping review:
A scoping review involves a search of the literature to determine what sorts of studies addressing the systematic review question have been carried out, where they are published, in which databases they have been indexed, what sorts of outcomes they have assessed, and in which populations (Petticrew and Roberts 2006). It may include restricted searches across a limited number of key databases, limited to a certain time period, and perhaps restricted by language. This can help cost a review for the purpose of drawing up a funding proposal, and can help with estimating how long it is likely to take, and what mix of skills might be needed to carry it out. From the below systematic review on effectiveness of low dye taping in the management of plantar fasciitis we can see that one relevant study has been found which involves effectiveness of taping in the management of plantar fasciitis but that differs from the current systematic review as it did not involve low dye taping which is the key factor of the undergoing review and this review is based on only effectiveness of low dye taping and not taping in broader context.
Chapter 3:
Role of the protocol:
The protocol will specifies the plan which the review will follow to identify, appraise and collate evidence (Cook, Sackett and Spitzer 1995). The first milestone of any review is the development and approval of the protocol before proceeding
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "plantar fasciitis"
Plantar fasciitis is one of the most common causes of heel pain. It involves inflammation of a thick band of tissue that runs across the bottom of your foot and connects your heel bone to your toes (plantar fascia). PF is usually diagnosed and common with runners, but can also be related to those that are obese.
Related Articles