Theories and principles of ethics and law in healthcare services.
Table of Contents
- Part 1
a. Introduction 3
b week 1 4
c. week 2 5
d. week 3 6
e. week 4 7
f. week 5 8
g. reference and appendix 9
2. Part 2 13
a. Introduction 14
b. Theories and principles of ethics in nursing practice 14
c. Laws in nursing practice. 15
d. case study 16
e. conclusion 18
f. references. 20
Part 1
weekly writings.
Introduction
In today’s clinical practice reflective thinking is an integral part for nurses and midwifes. Reflection helps to overview one’s own practice and awareness of competence and help to improve their knowledge that leads to better practice.
Reflection
Reflection means learning from an experience and using it in another similar situation.
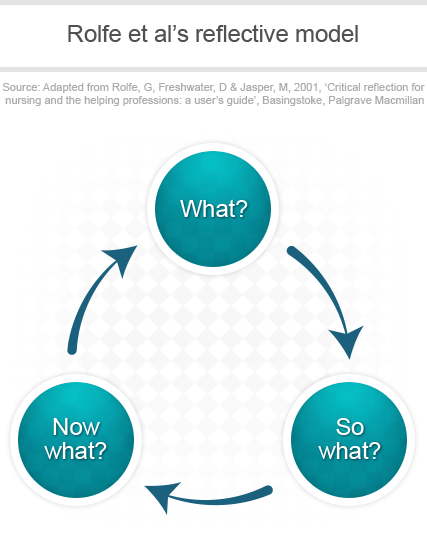
There are several models of reflection.
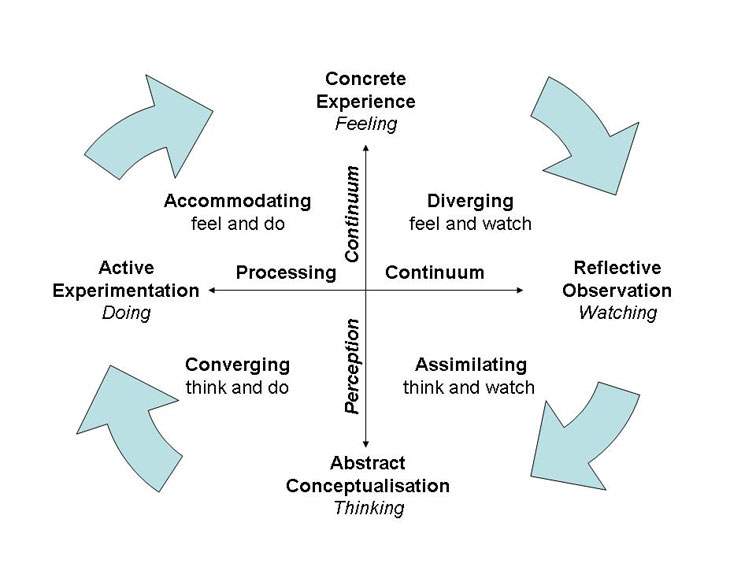
- Kolb 1984
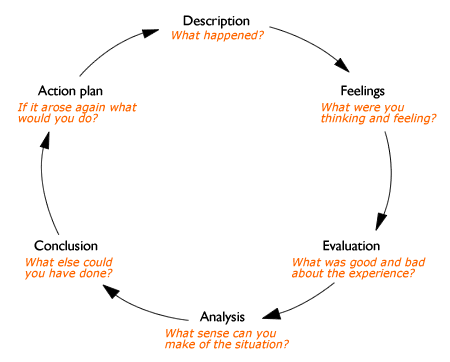
- Gibbs 1988
- Data 1991
- Johns1995
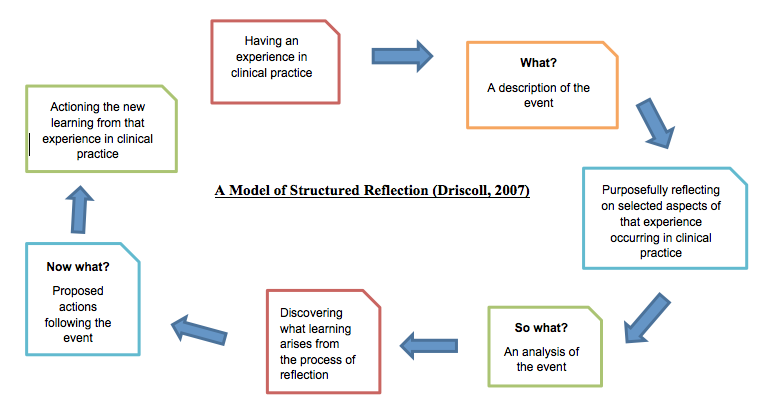
- Driscoll
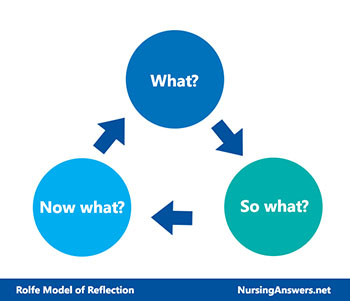
- Rolfe, Freshwater and Jasper 2001
Week 1.
“Autonomy is the freedom to make discretionary and binding decisions consistent with one’s scope of practice.” Lewis (2006)
I would reflect paternalism in the name of autonomy with a small scenario. The reflection model I used here is Gibbs model.
Liam (random name) aged 72 years old male was suffering from severe rectal bleeding and suspected rectal cancer, refused preparation for colonoscopy for further investigations and staging of the cancer. As a nurse it is my responsibility to send him for the appointment because he is deteriorating slowly with the bleeding and if he miss an appointment it’s hard to get an appointment very soon due to the current system. Liam has the autonomy to take decision for the appointment. I had decided to inform his sister (next of kin) and the consultant as I know he has rectal bleeding, to encourage him to go to the appointment and take the preparation. The doctor talked to him and given him all possible options and he opted for CT scan as he doesn’t want an invasive procedure.
Action plan.- I will be mindful next time to avoid a situation like this by early passing of all informations and updating the patient and NOK in advance and giving them ample time and all possible options to maintain autonomy.
Week 2
Management ethics
Ethics is concerned with ‘right and wrong’, although agreeing what is ‘right’ can be challenging.
Last month Irish nurses and midwifes organisation (INMO) call for an industrial action which demands pay parity with similar profession and safe staffing. I like to reflect this industrial action into my weekly reflection in the style of Rolfe model. The main questions was what was I trying to achieve, what is the importance. The main points of the industrial action was pay parity, salary increase and safe staffing. Consequences for the patients were nursing duties been withdrawn but essential care like medication rounds are catered. The strike committee had ensured that essential patient care been done and ensured that the patients are not suffering as result of industrial action. Wards like long stay been staffed as normal. Short stay ward staffed one only for essential or emergency care. No new admission been taken prior to the industrial action and patients been discharged early to avoid chaos. Every effort been taken to care for terminally and critically ill patients.
Reflection from the topic is what are the responsibilities of a manger in an event of industrial action, what are the main things to consider and how to manage the ward with out any negligence and complaints.
Week 3.
Confidentiality
Confidentiality is paramount in a civilised country like Ireland. Confidential documents in clinical setting is very much important as it contains clinical information like diagnosis and treatment of a person. This scenario I am going reflect with the what? Driscoll’s model of reflection
I am discussing a scenario which happened in my setting, a patient Rodney who’s sister is the NOK, she lives in Canada. This man has wife and daughter and they are living in Switzerland but they are not mentioned as NOK. This man became very ill one day and I want to inform to the NOK, as I am aware that the time difference between Ireland and Canada I want wait until the morning in Canada. I informed the sister. I also want to inform the daughter (visits yearly) but there is a legal issue. She is not the NOK. I reflected my experience with john’s 1995 cycle. And informed MSW and she took over the case and MSW informed his daughter. Later when Rodney became better then we got consent to keep daughter as NOK2.
The reflective learning from the scenario is importance of keeping the documents up to date.
Week 4
Consent
I would like to reflect informed consent with a small scenario with Gibbs reflective Cycle.
I had escorted a patient to SVUH for peg tube insertion the morning. I stayed with the patient until he had moved to the endoscopy room because the patient was bit challenging. He been transferred to the procedure room and after few minutes the consultant came to me and asked about the consent, the consent is missing and not included with the document I had given on admission. I never checked the documents because it been in a sealed envelope and never had an issue before. I became so upset and I feared the patient will loose the appointment and don’t want loose it. I asked the consultant whether I can get the NOK over the phone to consent but he is not happy with it. I had seen the consent from his wife (NOK) last day. The consultant said he couldn’t proceed the procedure without a valid written informed consent. I rang the ward asked to search for the consent, and arranged to transport it to the hospital and they did.
From this incident I had reflected the importance of informed consent and the legal and ethical issues behind it.
Week 5
End of life Ethics.
I would like to reflect a scenario with Rolfe reflective model (2001). The main process is what(what happened), so what(why is it important, what this means) and now what (what are going to do with it).
A female 89yrs old resident stopped eating and drinking and no urine output, doing poorly, Vitals unstable has signs of severe dehydration. Consultant reviewed and family been informed. DNR status was not discussed before left it do it when suits. Consultant prescribed subcutaneous fluids 500mls over 24hrs on trial basis and if not improving then discontinue the fluids and to start comfort care and will review next day. Resident didn’t improved and she started deteriorating. Family wants to prolong her and wants her to be transferred to an acute hospital for further diagnosis and treatment. I had initiated an MDT meeting with the family and discussed every aspect of treatment and transfer to another hospital and the NOK agreed to keep her here and continue the comfort care.
I had reflected from my old experience and initiated a MDT meeting with family.The learning or the outcome from this topic is more on the importance to keep the documentation up to date and the responsibility as a nurse.
References
- Ishikawa-nu.ac.jp. (2019). [online] Available at: https://www.ishikawa-nu.ac.jp/pdf/kenkyu/0302_01.pdf [Accessed 23 Feb. 2019].
- Chaloner , C. (2019). An introduction to ethics in nursing.
Appendix
Gibbs reflective cycle
Kolb’s learning cycle
“A nurse is not what you do. It is what you are… I am a nurse it’s not what I do, it’s what I am.”
Part 2
Introduction:
The main legal administrative body for nurses and midwives in Ireland is Midwifery Board of Ireland (NMBI). Their main role is to protect the wellbeing and security of people in general, by ensuring that nurses and midwifes are qualified enough to practice. The main responsibilities and roles are defined in Nurses and Midwives Act, 2011. It is necessary to provide unique assistance to Nursing and midwifery professions. To a degree, it is important that they should acknowledge the continuous-change obligated from the people and health service. It is also their responsibility to be aggressive and analyse the fields where they lack and requires additional training that would prompt development in patient’s outcome. Having a good knowledge of ethics and law in nursing is a vital part of nurses and midwifes professional standards. Ethics and law in healthcare emphasis on teaching applied ethics and law in a way that demonstrates the real world applications of these core components of nursing and midwifery curriculum.
Theories and principles of ethics in nursing and midwifery practice.
‘’Branch of philosophy that involves systematizing, defending, and recommending concepts of right and wrong conduct’’ Annabelle L (2017). Ethical principles are the base of decision making for planning one’s treatment in nursing and midwifery practice
The seven principles of ethics are beneficence, non-maleficence, fidelity, justice, veracity, confidentiality and respect for autonomy.
“Beneficence is defined as an act of aid, compassion and gentleness with a strong meaning of doing good to others including moral duty” Kinsinger. F. (2019)
Non-maleficence is defined as not to do any harm to others or make sure having a least harm possible with a good outcome. Beauchamp and Childress(2008).
Fidelity is defined as faithfulness to an individual or patient
Justice is defined as moral obligation to act on the basis of judgment between competing demands, equity and equality. There are three categories – distributive justice, rights based justice and legal justice.
“Veracityis the principle of truth telling, and it is grounded in respect for persons and the concept of autonomy” Regis university 2019.
Confidentiality means a piece of information about someone, keeping as secret.
Respect for autonomy means respect towards one’s right to take own decisions and liberty to act on those decisions.
Ethical theories are a system of ideologies by which an individual can decide what should do and what not to. The most used theories are utilitarianism and deontology. Utilitarianism means maximise the best for the most people. Deontology means ethics based on the duty regardless of the outcome.
Laws in nursing practice.
Law is a set of regulations imposed by government or a body of officials to control or normalise people’s behaviour. There 4 types of law, common law, constitutional law, legislation, human rights law and EU law. Health act 2011, is the main act been introduced in 2011, which has 13 parts includes the fitness to practice committee, competence and renaming Anbord altranais to NMBI. NMBI or nursing and midwifery board of Ireland’ the statutory body which sets the standards for the education, registration and professional conduct of nurses and midwives. NMBI Educates nurses and midwives how to care for patients , families and the society. The key roles of NMBI is to safeguard the public and integration of nursing and midwifery practice. They also establish and maintain the register of nurses. They sets standards and provide support to nurses. They are also responsible for establishing, maintaining and reviewing scope of practice, code of professional conduct and ethics.
The important aspect in law which are more reliable to nurses are autonomy, accountability human rights, professional practise, negligence, informed consents, confidentiality, professional relationship, access to information, legal issues and documentation, and beginning and end of life issues.
Case study
I would like to reflect the theories and principles of law and ethics with an incident happened in my ward John 90years old, had history of stroke, left hemiparesis, CAD, on COPD, on 2litre continuous oxygen via nasal prongs, is unwell and he was for resuscitation on admission according to his wish,. He is deteriorating and the consultant reviewed and decided to transfer him to the hospital. I had informed his NOK is his wife and but his wife and daughter doesn’t want him to be transferred or resuscitated due to the complications and his illness.
In this scenario there is legal and ethical dilemma as who’s decision to be followed. As per the autonomy it is the patient’s right and that should be respected or followed. On an ethical point of view beneficence or the good for the patient might indicate not for resuscitation. The point we consider will be the quality of life, justice to patient and non-maleficence in the event of resuscitation. To rule out the dilemma I have informed my manager and initiated a MDT meeting with family and discussed in detail including the current situation in emergency units, the suffering he might going through his stay in their and during the treatment like IV antibiotics, ventilator support etc. had discussed. Family had decided not to go for resuscitation and to start comfort care. He has been moved to a single room to maintain his privacy and dignity. The wife was so happy to have a private space and quiet room for their dying husband. I have clearly documented this in the nurses notes. [
Advocacy is an important idea in nursing practice; it is frequently used to describe the nurse-patient relationship. Patient advocacy is not merely the defence of breaches of patient rights. Advocacy for nursing originate from a philosophy of nursing in which nursing practice is the support of an individual to promote his or her own well-being, as understood by that individual. It is an ethic of practice. Advocacy refers to helping patients to obtain the needed care, assuring quality of care, defending the patients right and serving as abridge between the patient an the healthcare system. In this particular situation nurse act as an advocate between the family and the medical team for the best possible outcome for the patient relevant to his condition.
In NMBI’s professional code and ethics, confidentiality and trust is the 4th principle. Confidentiality and honesty form foundation of a faithful relationship between and client. Nurses and midwifes should take professional judgement and accountability where a confidential information is shared. In todays world we have more interest in keeping computerised documentation and automation, nurses and nurse mangers need be alert and aware that sensitive documents are more easy to access for more people with a benefit of good and bad.
“Clinical negligence is described as when an individual is harmed because the other person fails to do the care which reasonable and prudent person would use under the same circumstances, negligence said to have occurred” Peckmann.j.p (1996). In the scenario discussed above it is very easy to slip into this area of negligence if we didn’t do proper documentation. Nursing documentation is a information that explains about the care given to a patient or group of group of patients, which is written or electronically generated. Through documentation nurses communicates to other professionals in the system about their observations, decisions actions and outcomes of care. Documentation explains what happened and when.
Ethical dilemmas is defined as circumstances when a choice has to be made between two equally unsatisfactory alternatives. There are several methods to solve ethical dilemma, like refute the paradox, select an alternative that is better and less bad and find an alterative. In john’s case even though his autonomy hasn’t respected but the better option to opt for comfort care because that is better and less trauma or suffering for him and finally to keep him comfort for the days left. Ethical problem solving is important factor in nursing management.
Conclusion.
In the scenario I tried to critically evaluate the legal and ethical issue related to a patient’s autonomy VS beneficence. Both are equally important and autonomy had more weight than the beneficence but had to respect the family wishes as it seems more beneficial to the patient. The Nurse have to balance the legal and ethical aspect of a patients rights, freedoms and choices against what is the most beneficial and health maximizing approach. End of life care is an important ethical responsibility for the nurses. It is the main responsibility of the nurses to help there patients die in outmost nobility and responsibility. Nurses also have the legal and ethical responsibility to respond to the offer for care, indifferent of the approach. It the main responsibility of the nurses to check the health needs and decide the level needed for care. Nurses practicing in heath profession face many disputes, regardless of all disputes, they have very big favourable circumstances to provide in a certain way to boost the health of the needed people and have a good positive collision on the public heal. The limit of the patient ought to be evaluated and characterized before any interventions arranged and implemented with the moral thinking process working in parallel to guarantee the consideration and treatment of the patient isn’t just moral yet legitimate.
References
- Anon, (2019). Ethics at a Glance. [online] Available at: https://rhchp.regis.edu/HCE/EthicsAtAGlance/Veracity/Veracity.pdf [Accessed 25 Feb. 2019].
- Beachamp,T.L., & Childress, J.E.(2008). Principles of bio medical ethics.(6th ed.). New York:Oxford university Press.
- beckmann j p. (1996). nursing negligence. Available: https://books.google.ie/books?hl=en&lr=&id=-A05DQAAQBAJ&oi=fnd&pg=PP1&dq=negligence+in+nursing&ots=3oP2_GY3OK&sig=2O05YL_9NcShBmzBQBmo59VBw-A&redir_esc=y#v=onepage&q=negligence%20in%20nursing&f=false. Last accessed 26th feb2019.
- Cain, P. (1999) ‘Respecting and breaking confidences: conceptual, ethical and educational issues’, Nurse Education Today, 19(3), pp. 175–181. Available at: http://proxy.library.rcsi.ie/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=10578826&site=ehost-live (Accessed: 25 February 2019).
- Corporate Finance Institute. (2019). Ethical Dilemma – Definition, How to Solve, and Examples. [online] Available at: https://corporatefinanceinstitute.com/resources/knowledge/other/ethical-dilemma/ [Accessed 25 Feb. 2019].
- Fealy G., Casey M., Brady A.M., Hegarty J., Kennedy C., McNamara M., O’Reilly P., Prizeman G. and Rohde D. (2014) National Review of the Scope of Nursing and Midwifery Practice Framework. Dublin, Nursing and Midwifery Board of Ireland.
- Gelling L (1999) ‘Ethical principles in healthcare research’, Nursing Standard, 13(36), pp. 39–42. Available at: http://proxy.library.rcsi.ie/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=107201673&site=ehost-live (Accessed: 24 February 2019).
- Kinsinger, F. (2019). Beneficence and the professional’s moral imperative.
- Milholland, D. (2019). Privacy and confidentiality of patient information. Challenges for nursing.. [online] Europepmc.org. Available at: https://europepmc.org/abstract/med/8301390 [Accessed 25 Feb. 2019].
- Medium. (2019). Ethics Defined – The Ethical World – Medium. [online] Available at: https://medium.com/the-ethical-world/ethics-defined-33a1a6cc3064 [Accessed 25 Feb. 2019].
- Nmbi.ie. (2019). NMBI – Our role: Nursing & Midwifery Board of Ireland. [online] Available at: https://www.nmbi.ie/What-We-Do/Our-Role [Accessed 25 Feb. 2019].
- Nmbi.ie. (2019). NMBI – Code of Professional Conduct and Ethics. [online] Available at: https://www.nmbi.ie/Standards-Guidance/Code [Accessed 25 Feb. 2019].
- P, G. (2019). Nursing advocacy: an ethic of practice. – PubMed – NCBI. [online] Ncbi.nlm.nih.gov. Available at: https://www.ncbi.nlm.nih.gov/pubmed/7728551 [Accessed 25 Feb. 2019].
- Selvi, S. T. (2017) ‘Documentation in Nursing Practice’, International Journal of Nursing Education, 9(4), pp. 121–123. doi: 10.5958/0974-9357.2017.00108.8.
- Thompson, J., Thompson, H. and Kelly, L. (1992). Ethics in nursing. Lanham: University Press of America.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "rolfe reflective model"
The Rolfe model was developed initially for nursing and care education, but has become more broad in its subsequent applications, not least because of the clarity of the model and its ease of use. The three stages of the model ask you to consider, in turn, what happened, the implications of the occurrence, and the consequences for future conduct.
Related Articles