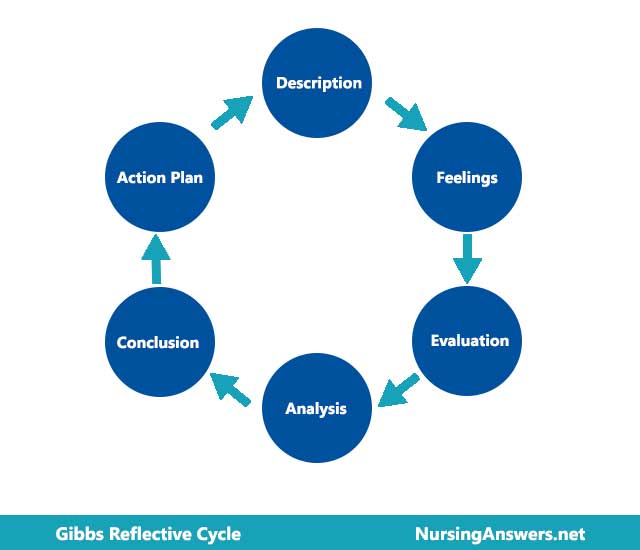
This is a reflective account of teaching a patient stoma care, using Gibbs Reflective Cycle (1988). By conceptualising the reflective cycle as commencing with a description of an event and ending with the development of an action plan, this model facilitates experiential learning. The model is praised for its focus on learning from experience rather than attempting to change experience (Rolfe et al., 2001). It also increases commitment to learning via the development of an action plan.
The following components of Gibbs model will form the structure of this reflective account: description; feelings; evaluation; analysis; conclusion; and action plan.
Description
The teaching took place on a male surgical ward that specialises in bowel surgery. The patient, ‘Tom,’ whose real name will remain anonymous in respect of confidentiality (NMC Code, 2008; NHS Confidentiality Code of Practice, DH 2003), was admitted for surgery for colorectal cancer. Tom would be provided with a temporary transverse colostomy post-surgery, which would require the learning of new skills in order for him to manage his own care needs once discharged from hospital.
Being patient-centred (Pelzang, 2010), I introduced myself to Tom and asked his permission to go through some information with him, explaining that the aim was to prepare him for managing his colostomy after surgery. The four steps to teaching colostomy care, as offered by Tolch (1997), were then implemented. These four steps comprised devising a teaching plan, assessing and documenting progress, encouraging participation, and anticipating problems.
Using sample equipment, I talked Tom through the procedure, step by step, with pauses to confirm his understanding or answer any questions. At first, all necessary equipment was assembled, including a stoma bag, scissors, disposal sack, soap, warm tap water, dry disposable wipes, and stoma sizing template. I discussed the equipment with Tom before showing him how to empty the pouch whilst ensuring no spillage and maintaining hygiene. Pictures were used, where appropriate, to show Tom how the peristomal skin needs to be cleaned with moistened gauze and repeated several times until the skin and stoma are clean. Tom was informed not to be alarmed by small specks of blood on the gauze, explaining that this is normal and can occur each time the stoma is cleaned due to the small blood capillaries on the stomal surface being very delicate.
Teaching Tom the basics of how to empty, clean, and change his colostomy was followed by the provision of some information on signs and symptoms of potential problems or complications, such as little or no stools, increased pain, and other signs of infection, etc. It was also necessary to teach Tom how to deal with problems that might arise after hospital discharge, such as a leakage. I also provided a contact list for colostomy supplies, along with details of the Colostomy Association, which provides telephone support and written information for patients. I encouraged Tom to maintain contact with the organisation and to access it as much as he needed. This would facilitate his transition from hospital to home, which can be a stressful time for patients with a newly formed stoma (Fulham, 2008).
Finally, a post-surgery teaching plan was devised collaboratively to provide reassurance that Tom would still be receiving help with developing his self-management skills once the colostomy was fitted.
Feelings
Initially, I was apprehensive about handling such a personal and sensitive topic with a patient, especially since I was aware that adjusting to a stoma can be both physically and psychologically challenging to the patient. I did not want to do or say anything that would in any way hinder this adjustment. I was particularly anxious of ensuring that I demonstrated that a colostomy can be self-managed effectively, whilst at the same time not being seen as dismissing any of Tom’s own concerns or anxieties.
I could sense that Tom was anxious, which reminded me that this was more difficult for him and thus I needed to be calm and confident in order to facilitate the learning process and relieve any of Tom’s own stresses. I am confident that I managed to achieve this as Tom became much more relaxed as the session progressed, asking more questions and becoming more involved.
I am disappointed, however, that my practice was influenced by assumptions. For example, I had not realised the importance of offering the patient the opportunity to have a family member or carer involved in the teaching process (Turnball, 2010). Assuming that the procedure being taught was so personal that the patient would not want anyone else involved in learning how to change their colostomy, I prevented Tom and his family members from having the opportunity to be more involved. Their involvement, if desired, might have been a useful process and, indeed, it would have ensured a level of consistent support on discharge from the hospital. Mezirow (1981) describes this reflection as a ‘perspective transformation’ – on reading the literature after a few teaching sessions with Tom, I realised that my belief system had influenced the way in which I taught Tom.
Evaluation
The pre-surgery teaching sessions have been successful and Tom has shown continued understanding of the implications of having a colostomy that needs regular changing. Indeed, during the last teaching session Tom took the role of teacher and showed me how to change a colostomy. He is still, understandably, nervous about when the time comes for him to do this on a regular basis, but has been reassured that he won’t be expected to be completely independent post-surgery. It is likely that myself or a colleague will initially change the colostomy so that Tom can observe the procedure before gradually becoming more involved.
I am aware that during this period I will need to be mindful not to show any signs of distaste when changing the colostomy as patients adjustment can be severely impacted by this (Armstrong, 2001). Indeed, I communicated sensitively at all times and was mindful of enabling Tom to be fully engage in the care process, as recommended by the Department of Health ‘expert patient’ approach to health management (DH, 2001), as well as the Health Foundation’s ‘co-creating health’ initiatives (Collins and Grazin, 2008). This appeared effective in developing a ‘partnership’ with Tom so that we could work together in developing his skills to manage his colostomy.
I found Tom’s engagement with the whole process very rewarding as it gave me much deeper insight into the needs of men preparing for a colostomy, which helped me to move beyond the basic teaching skills of changing a colostomy to a more tailored approach to teaching that addressed Tom’s specific needs. He was particularly concerned about the dietary implications of the colostomy and whether this would impact his social activities. My knowledge regarding the dietary aspects of colostomy care is basic and thus I was not prepared to adequately answer all of Tom’s questions. I did, however, provide him with an information leaflet covering such matters and told him that if he had any further questions I could find someone he could talk to.
Significant psychological symptoms, such as depression and anxiety, have been reported in 20% of patients with a stoma (White, 1997). Psychological morbidity is often the result of problems coming to terms with changes in body image and altered patterns of bowel elimination. For psychological adjustment to occur, it was fundamental for me to empathise with Tom whilst also reassuring him that there should be no need to impose any long-term dietary restrictions. Food is often a great source of concern for patients and on researching the literature and talking to colleagues I am now aware of the wealth of information and advice available for patients (Persson et al., 2005).
A significant challenge during the teaching process was that Tom was trying to adjust to a cancer diagnosis whilst at the same time trying to adjust to the lifestyle changes introduced by a colostomy. However, providing Tom with the skills to manage his own stoma is likely, according to the evidence, to facilitate psychological adjustment by providing a sense of control that would have previously been lost when first diagnosed (Bekkers et al., 1996). Indeed, studies have shown that increases in a patient’s feelings of control, which are enhanced when the patient has the appropriate set of skills to manage the situation, can be fundamental in adjusting to having a colostomy (McVey, Madill, and Fielding, 2001). Models of self-management also indicate that increasing a patient’s self-efficacy (confidence) to self-manage has a number of positive physical and psychological outcomes (Simmons et al., 2007).
There are some skills not demonstrated within the described teaching sessions, but which would have been present if I had been teaching Tom post-operatively. For example, it will be important for me to adopt infection control precautions by wearing disposable gloves and apron (Rust, 2007). At the same time, it will be important that I explain the rationale for this to Tom so that he doesn’t feel stigmatised. In preparation for this, I have made Tom aware of this pre-surgery.
Analysis
The teaching style adopted was based on social learning theory, which included assessing Tom’s readiness and ability to take an active role in learning about managing the stoma. On talking to Tom and seeing that he was keen to learn and become independent in taking care of the stoma, a teaching plan was devised. This was to be followed with the implementation of the teaching plan and then an evaluation of the process and outcome, in line with the structured approach to teaching recommended by O’Connor (2005). Furthermore, patient goals were set for post-surgery stoma care in order to help Tom progress towards achieving independence (Rust, 2007).
In devising the teaching plan, it was important to consider the type of colostomy Tom would be fitted with. In this case, it was a temporary transverse colostomy that would need emptying several times a day due to the elimination of soft stools. If Tom had a sigmoid colostomy, his stools would be firmer and less frequent, requiring less time and effort in management of the stoma.
Kember et al. (1999) have found that students can be categorised as non-reflectors (i.e. lack evidence of deliberate appraisal), reflectors (i.e. demonstrate insight through analysis, discrimination, and evaluation), and critical reflectors (i.e. indicate a transformation from initial perspective). This reflective account has highlighted that I am a reflector and that, indeed, I tend to reflect during as well as after an event. In this case, this has enabled me to identify my professional strengths and weaknesses. Identifying my strengths has increased my self-confidence in providing care and support within this area of healthcare. It has also enabled me to identify where further professional development is needed so that I can continue to hone the skills necessary to provide high quality patient care.
I agree with Pierson (1998) that reflection is a technique and a purposeful inter-subjective process, as well as with Heideggerian’s (1966) notion that reflection is the integration of calculative and contemplative thinking. It is a technique and resource that I shall continue to develop both professionally and personally.
Conclusion
As many as approximately 15,000 people in the UK undergo stoma surgery in the UK (White, 1998). Adapting to a stoma and its daily management can take time and thus teaching these patients the practical skills necessary for stoma care needs to ideally commence as soon as possible, preferably pre-surgery. Indeed, teaching needs to be conducted in a planned, organised manner, in collaboration with the patient and based on their own readiness and ability to learn about stoma care. Taking this organised approach ensures that no vital aspects of care are omitted and that the patient and healthcare provider are working towards mutually agreed goals.
The psychological implications of adjusting to a colostomy must not be underestimated or overshadowed by the need for practical skills in stoma care to be taught. Instead, teaching practical skills can be viewed as another component of psychological care since psychological adjustment can be affected if patients feel that they do not have sufficient knowledge and skills to change their colostomy or deal with any problems that might arise post-discharge (Metcalf, 2001).
Action Plan
Clause 3 of the UKCC Code of Professional Conduct (1992) states that nurses must “maintain and improve her professional knowledge and competence.” In relation to my professional knowledge and competence in teaching patients colostomy care, it is essential that I take steps towards continued professional development in terms of enhancing my knowledge surrounding the dietary needs of people with a colostomy. I have begun to meet this action plan by accessing nutritional advice from the Colostomy Association, but will endeavour to examine evidence-based practice in the provision of dietary advice for patients with a new stoma.
I would also like to learn some specific skills for increasing self-efficacy that I can integrate into my teaching approach. I have acquired greater insight into the importance of patient confidence in self-management. There is a wealth of evidence available for the importance of promoting self-efficacy and I intend to start increasing my knowledge in this area by reading a comprehensive systematic review on self-management programmes for cancer survivors (Davies and Batehup, 2010).
In addition, intend to rectify my assumptive actions surrounding the involvement of Tom’s family in the education process. During our next teaching session, I will ask Tom about his feelings regarding having anyone else involved in the teaching, with any expressed wishes being checked with relevant friends and family.
In conclusion, using this reflective model has helped me to realise that my learning is a proactive process accompanied by continual reflection that provides insight into areas for further professional development.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "gibbs reflective cycle"
Gibbs' Reflective Cycle was developed by Graham Gibbs in 1988 to give structure to learning from experiences. It offers a framework for examining experiences, and given its cyclic nature lends itself particularly well to repeated experiences, allowing you to learn and plan from things that either went well or didn’t go well. It covers 6 stages.
Related Articles