The aim of this assessment is to produce a patch work text incorporating three patches on professional understanding.
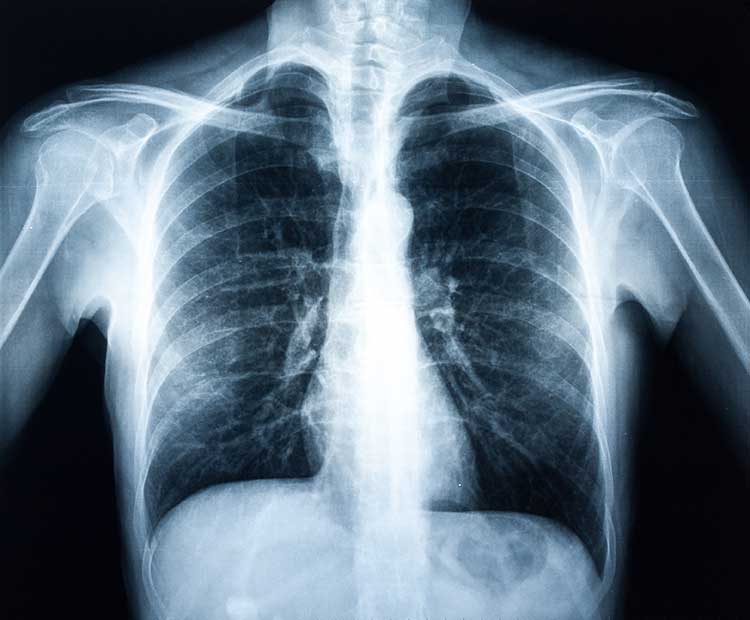
I am a second year Diagnostic Radiography student on a Inter professional programme working within the NHS. Radiography as a profession is very diverse and requires good communication among the inter-professional team. Diagnostic Radiography uses X-rays, Computerised Tomography (CT), Fluoroscopy, Nuclear Medicine, Ultra Sound and Magnetic Resonance Imaging (MRI) to generate images of bones and organs. Within this profession there are many aspects of ionising radiation that can be covered in one department; these aspects come under different modalities, many of which are mentioned above. The primary role of the radiographer is to diagnose injury or disease within the human body with the aid of these modalities using ionising radiation.
As a professional body that is in control of Radiation exposure, there are regulations and guidelines I must adhere to. Such as the radiation protection legislation and the code of professional standards and conduct in accordance with the Society of Radiographers (SoR), who are the radiographers governing body. IRMER, The ionising radiation (medical exposure) regulations, lay down the basic measures for the, 'health protection of individuals against the dangers of ionising radiation in relation to medical exposure.' This applies to anyone working with radiation within a medical environment and provides safe working surrounding s for both the radiographer and the patient. I am also bound to ten statements found within the code of conduct for radiography which exemplify the,' principles of professionalism, professional responsibility and accountability.' These codes and regulations are not only set in place to ensure good practice but to also protect the patient and provide excellent patient care.
Professional Understanding Patch 1
It is on reflection of my profession and these conducts that I wish to evaluate my role and contribution to the inter-professional team with the Gibbs reflective framework 1988 being used as my guide for reflection (see appendix), as this cycle, 'encourages you to think systematically about the phases of an experience or activity,'(Gibbs 1988). Whilst working within the confinements of the NHS I have unfortunately stereotyped many of my colleagues and feel I do not appreciate the true meaning of collaborative practice "An Interprofessional process for communication and decision making that enables the separate and shared knowledge and skills of care providers to synergistically influence the client/patient care provided," (Jones & Way, 2000). As after all, 'we all share as professionals the priority to make the care of people our first concern, treating them as individuals and respecting their dignity,' (NMC 2008)
As I look back over my practical experience I can see that it was pure naivety mixed with focused ambition which caused me to initially stereotype my colleagues. I was so intent on progressing through my degree that my main focus was on what I was learning in relation to radiography, by means of what images I was producing and whether or not they where diagnostic. My focus was on insuring I wasn't missing any vital pathology or fractures and on learning more of the anatomy so I could truly understand what I was looking for and why. It was this original determination that diminished the bigger picture for me, as I was unable to see the impact that as a professional I was having not just on the patient but on how the patients treatment will be managed and by who. The fact that I had little to no interaction with paediatric or adult nurses also contributed to this problem, but this was my own fault as I ignored these chances when they arose as I felt they would inhibit my main priority. So unfortunately to me my colleagues where still labelled as either subservient, "handmaidens" of the physician (Pillitteri & Ackerman, 1993) or the 'childish, plays all the time nurse' as there was no interest or need on my behalf to change this erroneous view. Ironically it was these views that would inhibit my professional development as in order for me to progress in the way I desired and become the best professional I could be I needed to appreciate my colleagues and work together with, 'one or more members of the health care team who each make a unique contribution to achieving a common goal," (CNO 2008).
It wasn't until professional issues arose on placement that I began to question why I had labelled my colleagues this way, my first thought was through slapstick comedy and the media, regardless of the reason I was sure these were labels I wanted removed. Through both practical experience and academic modules I was slowly able to gain more of an insight into the roles and responsibilities of both child and adult nurses and although there are obvious differences, the main being that I work with and administer radiation and they don't, I found I was writing more similarities. The Code of Conducts that each individual professional is bound by provides these similarities but it's our personal views on each profession and our lack of understanding that causes the stereotypes. Through understanding my own codes of conduct, ten statements set by the Society of Radiographers (SoR) and by comparing those with the codes set forth by the Nursing and Midwifery Council (NMC) and the Royal College of Paediatrics and Child Health (RCPCH), the main similarity between the professions is clearly visible, as both documents publicly set out,' the underpinning values and principles to promote, maintain and disseminate the highest standards of behaviour in order to enhance the good standing and reputation,' (SoR 2004) of that profession and both also endorse the importance of working with others to,' protect and promote the health and wellbeing of those in your care,' (NMC). It became clear to me that although our individual professions dictate our role within the practical setting the codes and legislations we each adhere to entwine. As it is our collaboration with other health care professionals that promote and maintain patient centred practice, providing the patient with the right care at the highest quality. As an adult nurse provides care to support the recovery of patients, I as a radiographer diagnose disease and am responsible for the examination of patients using radiation. These differences help me to define myself as a professional, but it is through the collaboration with others that I am made more individual. As individuals we each have a specific role to play but as a collective our roles are so much more important, as we would not be able to fulfil our purpose of making the care of people our primary concern without the help of other professional bodies.
825 words
Patch 2
Team work or team working can be defined as a certain number of people who have shared objectives at work and who cooperate, on a permanent or temporary basis, 'to achieve those objectives in a way that allows each individual to make a distinctive contribution,' (CIPD 2010).This meant that traditional hierarchical forms were gradually replaced with employees that were expected to fulfil a variety of roles, now known as collaborative practice. Marc Alperstein and Amélie Scalercio have constructed a piece of art, 'Collaborative Works,' (see appendix) that I feel embodies this transition and highlights the individual issues that surround collaboration. The picture itself seems to document a conversation or argument that exists between two wills who are struggling to impose their presence or mark into an act. 'It is necessary that these works engage in collaborative practice to record the struggle that ensues in this dynamic exchange, one that could not exist if operating in solitude,' (Artist statement). The image almost mimics what occurs within the confines of a hospital environment, as it demonstrates that without Interprofessional working we would not be able to fulfil our collective role of good patient management and care. 'Making a difference,' (DH 1999) suggests that effective care is the product of interagency working, where professionals work in collaboration to provide care which is designed to meet the needs of the patient. This concept was further promoted with the publication of The NHS Plan (DH 2000a) a ten year programme of reform practice. The NHS Plan (DH 2000a) aimed to create a service designed around patient needs, encouraging professionals to work together.
Collaboration however, does not come without its constraints, as portrayed in the artist impression the two hands are tied together, illustrating the conflict shown by each individual profession as 'Interprofessional working is extremely challenging in the workplace, and is not an easy concept for healthcare professionals to adopt,' (McWilliam et al 2003).Unfortunately this leads to a lower standard of care being delivered to patients within hospital environments, due to healthcare professionals misunderstanding the policies, education and research regarding Interprofessional working. This is owed to the, 'lack of support and training from managers,' and the need for, 'managers to involve staff in changes within practice and that this involvement facilitates co-operation.' (Deegan et al 2004). Co-operation is a major factor of a successful Interprofessional team as it not only benefits and improves the care that we provide to our patients but also enables the team itself to act efficiently by enabling professional benefits such as the, 'sharing of knowledge and the opportunities to experience areas of work outside ones own remit.' (Barr 2004) The advantages are not only work related it is also suggested that professionals may have levels of improved job satisfaction and increased levels of confidence in dealing with difficult situations.
We are all so focused on our individual job roles and on the polices and procedures that define us as a professional that we create our own conflict with an opposing profession as we try to prove ourselves, which is echoed in the picture. As each person holds one end of the tie, the tie representing the constraint we place upon ourselves and upon our professional identity, with each hand representative of how this constraint is self inflicted. After all this an image of two wills struggling to find their presence or mark in an act, as we at our place of work struggle to define our role within the patient pathway. However it is this conflict that diminishes the bigger picture as, as each hand is responsible for creating this conflict restraint; one hand can not break free of the bound without the collaboration of the other. This strongly relates back to practice as without the help and cooperation of another profession the patient like the hand would not be able to progress and consequently become free without Interprofessional collaboration. In order for us as professionals to 'provide care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions' (Institute of medicine PCC) we must work as Interprofessional team and, 'learn from and about each other to improve collaboration and the quality of care." (CAIPE 1997). There will always be a time that I as radiographer will need to cooperate with other members of the Interprofessional team, be it in surgery with consultants, anaesthetists and nurses or in the department with the radiologists, and it is this collaboration that will ensure that the patient is the focus point and that they will be managed and assessed as an individual with all pathways collectively working together, as opposed to two wills who are struggling to impose their presence or mark into an act.
Words 798.
Patch 3
Throughout this past year the main focus both practically and academically has been on collaborative practice, and how this has represented itself as a personal struggle to over come problems such as stereotyping colleagues, conflict issues and communication concerns. With the aid of the CPD module these issues that once clouded personal judgment faded and the real connotation of collaborative practice was revealed. Collaborative practice infers that people from different professional and academic backgrounds form a working relationship for the purpose of enhanced service provision.
Although the real value of collaborative working is clear the move towards collaborative practice in Health and Social Care proved challenging, as it was essentially, 'the change from institutional to community-based care,' (Barr et al, 1999). This meant that the, 'demarcations and hierarchical relations between professions were neither sustainable,' (Sibbald, 2000) or appropriate and new ways of working that, 'crossed professional boundaries had to be created, in order to allow a more flexible approach to care delivery,' (Malin et al, 2002). This transition became the cause of conflict within a now Interprofessional team and as a result stereotypes were formed and communication problems arouse. It seems that although this change was for the better, in providing a better standard of care for the patient, this focus was lost by the professionals whose duty this was. This is still very much an issue, where professionals are so centred on their individual position; they forget how much of a role they play in the Interprofessional team. The fact that collaborative practice has lacked a clear definition and instead has been linked with terms such as cooperation, coordination, participation and integration, has in some ways strengthened the issues that have prevented professionals from satisfying its purpose efficiently. It is also a relatively new field of practice, 'with the first major studies being undertaken in the 1980s,' (Roy, 2001) however, since the implementation of the 1990 NHS and Community Care Act (Department of Health, 1990), the collaborative practice has featured prominently in government policy documents to promote, 'joint working, partnership and the creation of a 'seamless service' between health and social care,' (Maxwell, 1998; Payne, 1995).
The importance of collaboration has always been emphasised practically and is also part of the academic pathway in the hope that the surrounding issues can be resolved before practitioners become professionals. Throughout the module the significance of collaboration with regards to person centred care became more important than the issues that encircled collaborative practice. It became increasingly essential to see the patient as equal partners in planning, developing and assessing care to make sure it is most appropriate for their needs and putting service users and their families at the heart of all decisions. In order to provide an excellent level of service each patient needs to be viewed as the individual they are, they can not be stereotyped by their age, sex, or symptoms. The main reason being that the way in which one patient is managed and treated would not work for another patient representing with the same symptoms, as his or her body could react differently to that treatment, thus complicating the initial problem. It is the duty of any professional body to provide, 'care that respects the person as an individual and is arranged according to their needs,' (DH 2008). However this care can not be administered without good communication from each professional that is responsible for the pathway of each individual service user. Communication is pivotal in a successful relationship be it between colleagues in the work place, students at university or family at home, it enables individuals to express themselves their concerns or relay important information to others. When this barrier is broken especially within the hospital sector each department become isolated and effectively treats the patient blind, as without communication from the nursing staff or the accident and emergency department a radiographer would not be aware of the symptoms a patient presents with and would therefore not be able to conduct an examination catered to that individuals needs. The requirement for good communication enhances not only the professionals' skills and ability to provide and excellent level of person centred care but enables a successful Interprofessional team to be consolidated, something that is also promoted academically. Interprofessional Learning can be defined as, 'Occasions when two or more professions learn with, from and about each other to improve collaboration and the quality of care,' (CAIPE 2005). Interprofessional learning enables different health and social care workers and agencies to gain a greater appreciation of each others values, knowledge and abilities and facilitates the best use of their skills which underpins the reality of the complexity of healthcare. Single professions or individual professionals working in isolation do not have 'the expertise to respond adequately and effectively to the complexity of many service users' needs,' (CAIPE 2006). In order to ensure that care given is safe, seamless and of a high standard it is essential that individual professionals,' respect the integrity and contribution of each profession,' (CAIPE 2006) and communicate with them effectively, relaying all the appropriate medical history and continuing to work closely with each other to ensure the patient is managed correctly and efficiently.
Good patient care stems from a well defined Interprofessional team that collaboratively work with each other, to overcome communication issues, conflict issues and the stereotyping of their colleagues. By doing this all the professionals involved are able to treat the patient as an individual and cater to their individual needs, making them a part of the process and involving them in the decisions made about them. This all bauds well for the successful running of the NHS and in turn successful patient management, each professional chooses to be apart of this system to improve the quality of life for each and every service user, but it is important to remember that this can not be achieved by individuals who become isolated form a team. Although it is important to be an individual, it is of greater importance to be individual that is a part of an Interprofessional team.
Words 1014.
References:
Barr, H (2005) Interprofessional Education: Today, Yesterday and Tomorrow. Accessed on 30.08.10. Reviewed 2004. Available at: http://www.health.heacademy.ac.uk/publications/occasionalpaper/occp1revised.pdf
CAIPE. Interprofessional learning. Accessed on 23.11.10. Reviewed 2010. Available at: http://www.caipe.org.uk
CIPD 2010 Team working. What is team working? Accessed on 03.10.10. Reviewed on 01.01.10. Available at: http://www.cipd.co.uk/subjects/maneco/general/teamwork.htm.
Collaborative works. Marc Alperstein and Amélie Scalercio. Accessed on 16.08.10. Reviewed 2010. Available at: http://www.marcalperstein.com/collaboration
Cooper, H., Braye, S,. and Geyer, R. ( 2004) Complexity and Interprofessional education. Learning in Health and Social Care 3 (4) pp 179-189. Accessed 02.02.10.
DOH (2000a) A Health Service of all the Talents: Developing the NHS Workforce. DoH London. Accessed on 30.08.10. Reviewed 2010. Available at: www.dh.go.uk
DOH (2000b) The NHS Plan: A Plan for Investment, A Plan for Reform. DoH London. Accessed on 30.08.10. Reviewed 2010. Available at: www.dh.gov.uk
DOH (2001) Working Together - Learning Together: a Framework for Lifelong Learning for the NHS. DoH London. Accessed on 30.08.10. Reviewed 2010. Available at: www.dh.gov.uk
Framework for action on Interprofessional education and collaborative practice. Health professionals networks nursing and midwifery human resources for health. Publisher WHO the world health organisation. Reviewed 2010. Accessed 20.08.10
Freeth, D (2001) Sustaining Interprofessional collaboration. Journal of Interprofessional Care 15 pp 37-46. Accessed 02.09.10.
Gibbs G (1988) Learning by Doing: A guide to teaching and learning methods. Further Education Unit. Oxford Polytechnic: Oxford 2009. Accessed on 20.08.10. Reviewed 2009. Available at: http://www.brookes.ac.uk/services/upgrade/a-z/reflective_gibbs.html
Glen, S and Reeves, S. (2004) Developing Interprofessional education in the pre-registration curricula: mission impossible? Nurse Education in Practice 4 pp 45-52. Accessed 05.09.10
Gordon F, Walsh C, Marshall M, Wilson F, Hunt T (2004). Developing Interprofessional capability in students of health and social care - the role of practice-based learning. Journal of Integrated Care 12 (4) pp 12-18. Accessed 05.09.10
Interprofessional Collaboration among health colleges and professions. College of nurses Ontario (CNO). Accessed on 22.08.10. Reviewed May 2008. Available at: http://www.hprac.org
Interprofessional learning. Practice based learning. Accessed n 25.11.10. Reviewed 04.09.08. Available at: http://www.practicebasedlearning.org/resources/ipl/intro.htm
Interprofessional learning and caring for needs. London: South Bank University.
Whitehead, D. (2001) Applying collaborative practice to health promotion. Nursing Standard. 15(20) pp33-37. Accessed 15.11.10
Jones and Way 2000 collaborative practice. Collaborative practice. Support the development of improved collaboration in healthcare. South eastern Interprofessional Collaborative Learning Environment (SEIPCLE). Queens University. Accessed 20.08.10. Reviewed no date. Available at: http://www.rehab.queensu.ca/uploads/clined/CollaborativePracticeModule.pdf
Patient centred care. Why patient centred care? Accessed on 21.08.10. Reviewed 2008. Available at: http://www.patientcenteredcare.net/.
Patient centred care policies (2008). Accessed on 21.11.10. Reviewed 2010. Available at: www.dh.gov.uk.
Person centred care. The health foundation . Accessed on 20.11.10. Reviewed 2010. Available at: http://www.health.org.uk
Person Centred Care (2006). Accessed on 21.11.10. Reviewed 2010. Available at: www.cmg.org.uk.
RCPHC. Royal college of paediatrics and child health. Codes of Conduct. Accessed 23.08.10. Reviewed no date. Available at: http://www.rcpch.ac.uk.
SoR statements of conduct Radiography. Statements for Professional Conduct. The college of radiographers. Accessed 22.08.10. Reviewed September 2004. Available at: www.sor.org
Appendix 1
Gibbs reflective cycle 1988
http://www.deakin.edu.au/itl/pd/tl-modules/teaching-approach/group-assignments/images/reflective-practice.gif
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "radiography"
Radiography: specialisation in the use of radiographic, radiation therapy and magnetic resonance equipment to administer radiation treatment and produce images of body structures for the diagnosis and treatment of injury and disease.
Related Articles