This brief considers the empirical literature on the use of clinical guidelines in patient care. It is argued that negative guideline characteristics and justified concerns amongst doctors negate satisfactory adherence.
Clinical guidelines have been part of the UK landscape for many decades, as a means of improving health care for patients (Woolf et al, 1999). Research evidence suggests that a significant proportion of physicians do not adhere to clinical guidelines in patient care (e.g. Grol et al, 1998; Forsythe et al, 1999; Sherr et al, 2001; White, 2001; Thomas et al, 2003).
Sherr et al (2001) investigated adherence of Obstetric Units in the UK and Eire to antenatal HIV testing policies. The Department of Health and Royal College of Obstetricians have both issued specified guidelines, which require that antenatal HIV testing be offered to all pregnant women, and adherence to these benchmarks has generated some debate. Data from 89% of antenatal units was analysed. Only 10% of units offered testing to all presenting women, and these units were concentrated in areas of high HIV prevalence (i.e. London). Other units operated selective screening policies (offering antenatal testing to some women, identified on the basis of clinical criteria) or ‘on request’ screening.
Forsythe et al (1999) studied adherence of senior NHS staff (consultants, general practitioners) towards BMA guidelines on the ethical responsibilities doctors have towards themselves and their families. The Academy of Royal Medical Colleges, and the General Medical Council both endorse these guidelines, which generally require that doctors do not assume responsibility for their own personal (or family’s) health care. Questionnaire data was collected from four randomly chosen NHS Trusts and three local medical communities in the London (South Thames) area. Personal use of health services was the outcome measure.
Results showed that although most doctors (96%) were registered with a GP, the majority (63% of GPs and 59% of consultants) had not consulted their GP in the past year. Almost a quarter (24%) of consultants stated they would never see a GP before obtaining consultant advice. The majority (71% of GPs and 76% of consultants) self-prescribed drugs ‘usually’ or ‘sometimes’. Forsythe et al (1999) concluded “senior doctors are not following the BMA guidelines on looking after their own and their families health” (p.608).
Clinical guidelines are thought to have significant benefits for patient care (Woolf et al, 1999). However, research findings on the impact of guidelines are mixed (Morrison et al, 2001; Bennewith et al, 2002; Bousquet et al, 2003).
Bousquet et al (2003) conducted a randomised controlled trial assessing the value of guidelines of the International Consensus on Rhinitis (ICR) in caring for patients with seasonal allergic rhinitis. GPs were randomised into two groups: one group followed ICR guidelines (patients received an oral anti-histamine, a topical corticosteroid, and/or a topical ocular cromone) while the other group were free to choose appropriate treatment for patients. Outcome measures were degree of impairment[1] and symptom medication scores. Patients treated by the guidelines strategy GPs generated lower symptom scores over a three-week period compared with patients assigned to free-choice GPs. Furthermore, patients in the guideline group reported greater reductions in their degree of impairment compared to the free choice group. This trial clearly demonstrated the benefits for patients of implementing clinical guidelines.
Diggory et al (2003) reviewed the results of five audits relating to cardiovascular-pulmonary resuscitation (CPR) at the Mayday University Hospital. At least one audit focused on doctors’ adherence to elderly care policy and guidelines recommended by the Royal College of Physicians. Documentation of a CPR decision, review of all patients, and documentation of any changes to the CPR decision became policy in the emergency department. CPR decisions were documented by both trainee doctors and consultants for >91% of cases. Consultants reviewed 93% of patients within 24hours, and documented a CPR decision in 81% of cases. Benefits for patients seemed to present in a reduction in DNAR[2] orders.
Other research suggests that the benefits of guideline adherence for patients may be more limited. Morrison et al (2001; Bennewith et al, 2002) assessed the impact of clinical guidelines for the management of infertility, in both primary and secondary care settings.
.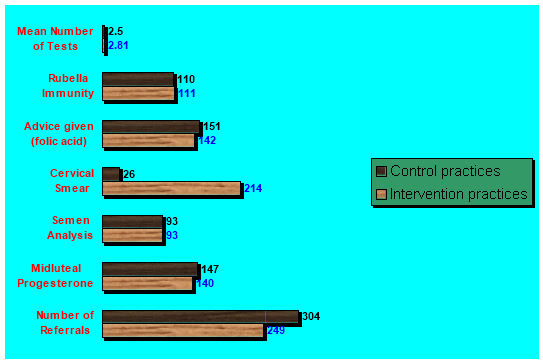
Figure 1 Clinical investigations completed for intervention and control practices (Morrison et al, 2001)
Over 200 general practices and NHS hospitals accepting referrals for infertility in Greater Glasgow were randomised to a control or intervention condition. The intervention group received clinical guidelines. No group differences were found in referral rates, albeit referrals from intervention practices were more complete, incorporating all essential clinical investigations (e.g. semen analysis, rubella immunity) (see Figure 1).
No group differences emerged in the percentage of referrals in which a management plan was achieved within one year, in the mean duration between first appointment and date of management plan, and costs of referrals. On the whole, this study demonstrates a differential effect of guideline adherence across different criteria of patient care. Despite the (modest) increase in the number of recommended clinical investigations performed prior to referral, clinical guidelines were no more cost effective than having no guidelines. Overall, research findings are mixed regarding the benefits of guideline adherence for patient. Nevertheless, improvements in some aspects of care have been demonstrated.
What guideline characteristics are pertinent to adherence? Michie et al (2004) assessed the reasons why GPs do not always conform to guidelines. The focus was on guidelines set by the UKs National Service Framework (NSF) for Coronary Heart Disease (CHD). London based GPs, who were classified as either ‘high implementers’ (adhered to five or more of 6 CHD standards) or ‘low implementers’ (adhered to 1 or 2 guidelines), were interviewed on their beliefs, self-reported behaviours, and organisational context. Several issues differentiated the two groups: views about evidence based practice; control over clinical practice; and the repercussions of adhering to guidelines.
Low implementers were more sceptical about evidence-based practice, more worried about the lack of control over the development and implementation of guidelines, and their own professional duties as doctors, and adverse consequences for GPs/patients that outweigh any benefits. This study highlights the importance of GP attitudes towards guideline adherence.
Irani et al (2003) emphasised the methodological characteristics of the guidelines themselves. They assessed the quality of national clinical practice guidelines (CPGs) on benign prostatic hyperplasia, and lower urinary tract symptoms. Two independent assessors appraised methodological quality of the CPGs using the St.Georges Hospital Medical School Health Care Evaluation Unit Appraisal Instrument. This tool incorporates items gauging three criteria: rigour of development (e.g. ‘Is there a description of the sources of information used to select the evidence on which the recommendations are based?’), context and content (e.g. ‘Is there a satisfactory description of the patients to which the guidelines are meant to apply?’), and clinical application (‘Does the guideline document suggest possible methods for dissemination and implementation?’). Analysis revealed substantial variability in quality across CPGs.
Grol et al (1998) found an association between guideline characteristics and adherence. An observation design was used to study 47 specific recommendations from 10 clinical guidelines in relation to 12 different guideline characteristics. For example, evidence base, clinical experience, concerned with daily practice, and ambiguity. Regression analysis revealed three key characteristics that predicted most of the variance in compliance rate: ‘the recommendation is vague and not precisely defined’, ‘the recommendation demands change of fixed routines’, and ‘the recommendation is controversial and not compatible with current values’.
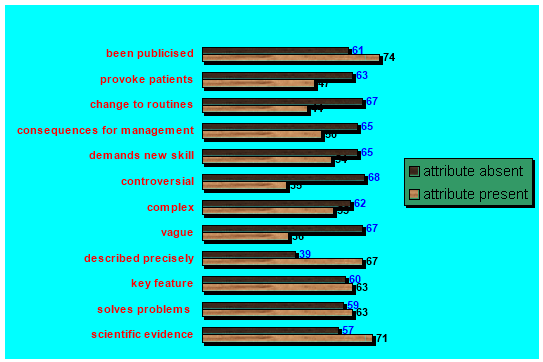
Figure 2 Rates of compliance across guideline attributes (present or absent) (Grol et al, 1998)
Figure 2 illustrates differentials in adherence rates as a function of the presence or absence of different guideline attributes. In general practitioners were more likely to comply in the presence of an evidence base, capacity to solve clinical problems, precisely described, and media publicity. Compliance was also more probable in the absence of capacity to provoke patients, requiring change to clinical routines, significant consequences for management, demanding new skills/training, controversy, complexity, and ambiguity.
Clinical guidelines in the UK have historically been prescribed by a multiplicity of agencies, notably the Department of Health, and profession-specific bodies, such as the Royal College or Surgeons, Royal College of Nursing, and British Medical Association. The National Centre for Clinical Excellence (NICE) currently sets clinical guidelines. This body continually publishes benchmarks for most areas of clinical practice. The Department of Health has also established Essence of Care standards, which have a more generic focus (DOH, 2003). Guidelines are purportedly based on empirical evidence, notably randomised control trials, hence satisfying the requirement for evidence-based practice. However, reservations amongst GPs about the notion of evidence-based guidelines, which often fall outside their clinical experience, has been identified as one reason for low adherence amongst doctors (The BRIDGE Study Group, 2002; Michie et al, 2004). GP scepticism is partly justified.
Morice and Parry-Billings (2006) discuss the validity of such ‘evidence’, identifying several important important issues. Firstly, NICE, the DOH, and other relevant prescribing bodies rely on clinical trials, many of which select patient groups “to give the trial treatment maximum scope to show an effect”. Then there is publication bias –studies showing positive or dramatic effects are more likely to be published than studies showing no difference/effect. Guidelines are often linked to meta-analyses, which by definition will be ‘infected’ by the research biases already mentioned. What is worrying is that many national guidelines are adapted locally, in the form of hospital policy (e.g. Sherr et al, 2001; Diggory et al, 2003), and these adaptations may have an even weaker evidence base than the national benchmarks set by NICE, DOH, and other prescribers. None of this is likely to improve GPs attitudes towards guideline adherence.
Do doctors need guidelines? In a discussion of heart disease regulations in the UK, Petch (2002) argued that the specification of treatment criteria has not been very successful in the USA and other countries. Adherence to guidelines is criticised on three grounds. Firstly, guidelines imply universal health care, an ideal most nations cannot afford, least of all the UK, which relies on rationing (i.e. waiting) due to limited health resources. Attempting to implement similar standards for every single patient is expensive. Secondly, recommended treatments can often have complications/side effects, so that certain treatments may be inappropriate for certain patients, but yet be a mandatory therapy, which the doctor is compelled to follow regardless. Thirdly, administering the same treatment to all patients is not cost-effective. The treatment may not benefit every patient. It is usually not clear “which patients will benefit from which drugs and hence the victim of a heart attack will be recommended to take aspirin, a statin, a β blocker, and an angiotensin converting inhibitor, in addition to other drugs…” (p.474).
Nevertheless, guidelines remain an integral element of patient care. This raises an important question: what kind of support do GPs require in order to adhere to guidelines? Marshall et al (2001) investigated factors that facilitate guideline acceptance in health professionals. Representatives from general practices in the NHS Northern and Yorkshire region were interviewed. Thematic analysis highlighted several issues including the need for training (staff often lacked the requisite clinical expertise to implement some guidelines), a conflict between responsibility and control (nurses/doctors are responsible for implementing criteria, but have no say over resource allocation), the and ‘cul-de-sac’ of patient non-compliance (e.g. little can be done if patients refuse treatment, and this is interpreted as failure of staff to adhere to guidelines).
CONCLUSION
Several key issues have emerged from this review. Firstly, research findings are mixed regarding the benefits of clinical guidelines for patient care. There is clearly a need for more randomised controlled trials. The benefits for patients probably vary across disease types, clinical setting, and doctor and patient characteristics. Doctors have serious concerns about the use of guidelines in patient care, and these reservations are mostly justified. Perhaps the most defensible concerns relate to questionable evidence base, the need to account for differences in how individual patients respond to treatment, and poor guideline characteristics, such as ambiguity. Unsatisfactory guideline implementation by doctors will probably persist until these problems are fully addressed by NICE and the Department of Health.
BIBLIOGRAPHY
Bennewith, O., Stocks, N., Gunnell, D., Peters, T.J., Evans, M.O. & Sharp, D.J. (2002) General practice based intervention to prevent repeat episodes of deliberate self harm: cluster randomised controlled trial. British Medical Journal, 324, p.1254.
Bousquet, J., Lund, V.J., van Cauwenberge, P., Bremard-Oury, C., Mounedi, N., Stevens, M.T. & El-Akkad, T. (2003) Implementation of guidelines for seasonal allergic rhinitis: a randomised controlled trial. Allergy, 58, pp.733-741.
Diggory, P., Cauchi, L., Griffith, D., Jones, V., Lawrence, E., Mehta, A., O’Mahony, P. & Vigus, J. (2003) The influence of new guidelines on cardiopulmonary resuscitation (CPR) decisions. Five cycles of audit of a clerk proforma which included a resuscitation decision. Resuscitation, 56, pp.159-165.
Forsythe, M., Calnan, M. & Wall, B. (1999) Doctors as patients: postal survey examining consultants and general practitioners adherence to guidelines. British Medical Journal, 319, pp.605-608.
Grol, R., Dalhuijsen, J., Thomas, S., Veld, C.I., Rutten, G. & Mokkink, H. (1998) Attributes of clinical guidelines that influence use of guidelines in general practice: observational study. British Medical Journal, 317, pp.858-861.
Irani, J., Brown, C.T., van der Meulen, J. & Emberton, M. (2003) A review of guidelines on benign prostatic hyperplasia and lower urinary tract symptoms: are all guidelines the same? British Journal of Urology, 92, pp.937-942.
Marshall, J.L., Mead, P., Jones, K., Kaba, E. & Roberts, A.P. (2001) The implementation of venous leg ulcer guidelines: process analysis of the intervention used in a multi-centre, pragmatic, randomised, controlled trial. Journal of Clinical Nursing, 10, pp.758-766.
Michie, S., Hendy, J., Smith, J. & Adshead, F. (2004) Evidence into practice: a theory based study of achieving national health targets in primary care. Journal of Evaluation in Clinical Practice, 10, pp.447-456.
Morice, A.H. & Parry-Billings, M. (2006) Evidence based guidelines – a step too far? Pulmonary Pharmacology and Therapeutics, 19, pp.230-232.
Morrison, J., Carroll, L., Twaddle, S., Cameron, I., Grimshaw, J., Leyland, A., Baillie, H. & Watt, G. (2001) Pragmatic randomised controlled trial to evaluate guidelines for the management of infertility across the primary care-secondary care interface. British Medical Journal, 322, pp.1-5.
Petch, M.C. (2002) Heart disease guidelines, regulations, and the law. Heart, 87, pp.472-479.
Sherr, L., Bergenstrom, A., Bell, E., McCann, E. & Hudson, C.N. (2001) Adherence to policy guidelines – a review of HIV ante-natal screening policies in the UK and Eire. Psychology, Health and Medicine, 6, pp.463-471.
The BRIDGE Study Group (2002) Responses of primary health care professionals to UK national guidelines on the management and referral of women with breast conditions. Journal of Evaluation in Clinical Practice, 8, pp.319-325.
Thomas, A.N., Pilkington, C.E. & Greer, R. (2003) Critical incident reporting in UK intensive care units: a postal survey. Journal of Evaluation in Clinical Practice, 9, pp.59-68.
White, S.M. (2001) An audit of audit and continued educational and professional development. Anaesthesia, 56, pp.1003-1004.
Woolf, S.H., Grol, R., Hutchinson, A., Eccles, M. & Grimshaw, J. (1999) Clinical guidelines: potential benefits, limitations, and harms of clinical guidelines. British Medical Journal, 318, pp.527-530.
Footnotes
[1] Using the Standardised Rhinoconjunctivitis Quality of Life Questionnaire (RQLQ).
[2] ‘Do not attempt resuscitation’
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "CPR"
Cardiopulmonary resuscitation is a “combination of oral resuscitation (mouth-to-mouth breathing), which supplies oxygen to the lungs, and external cardiac massage (chest compression), which is intended to normalise cardiac function and blood circulation.
Related Articles


