Interprofessional Education: the Attitudes of Respiratory Care, Nursing and Clinical Laboratory Sciences Students to Shared Learning at Prince Sultan Military College of Health Sciences (PSMCHS) in Dhahran, Saudi Arabia.
Introduction:
The health professionals vary in knowledge and skills and that have blurred the boundaries of different health professions. A brief review of literature reveals a belief thatInterprofessional education (IPE) has been recognize as an effective way of teaching that improve team work & collaborations, roles & responsibility and professional identity between health care providers that reflect on the care provide it to the patients. Interprofessional education (IPE) intends to improve training and communication among health professions, and prepare practitioners to provide effective patient-centered collaborative care1. Currently, the frequency and scope of IPE is increasing in different medical schools in U.S. and other countries worldwide1. In Saudi Arabia, there is no evidence that IPE has been used or applied.
Statement of the problem:
Interprofeesional education is an effective way of teaching that has been recognized globally. And it’s widely spreading around the world. There is no evidence that IPE has been applied in Saudi Arabia. Because of Increasing of allied health care disciplines and to provide the optimal care for the patient care all disciplines should work as a team, Interprofessional education provide the essential requirements to work as a team by focusing on three main subscales include teamwork & collaboration, professional identity and roles & responsibilities. Each subscale will reflect certain advantage.
Purpose of the study:
The aim of this study was to determine the attitudes of respiratory care (RC), nursing and clinical laboratory sciences (CLS) students during the last semester prior their graduation toward IPE using Readiness for Interprofessional Learning Scale (RIPLS) questionnaire2.
Significance of the study:
Interprofessional Education is an effective way of teaching. That’s why we need to improve PSMCHS student’s outcome and make them ready and increase their knowledge.
Research Question:
What are our student’s attitudes toward IPE?
Review of literature:
Interprofessional education (IPE) is not a new in the health care sector for researchers and professionals. However, after conducting a comprehensive review of the literature pertaining to IPE, it became clear that among the proponents of IPE initiatives, there is a lack of clarity surrounding the concept of IPE. The aim of (IPE) is to enable learners to get knowledge, skills and professional attitudes which they would not be able to get it effectively in any other way. To maximize the strengths and skills of health workers you have to implement Interprofessional education and collaborative practice, enabling them to function at the highest capacity3. With a current shortage of 4.3million health workers, implementing (IPE) is an effective way will become more and more necessary to manage the tension placed on health organizations1.
The most reported benefits in the literatures from implementing interprofessional education are: Students have real world experience and insight, Programme development will attract Staff from a range of professions, students learn about the job of other practitioners, workplace practices and productivity will improve, patient outcomes will improve, confidence of the staff will be raised, patient safety will be improved1.
IPE around the world:
According to The World Health Organization (WHO), IPE is “the process by which a group of students or workers from the health-related occupations with different backgrounds learn together during certain periods of their education, with interaction as the important goal, to collaborate in providing primitive, preventive, curative, rehabilitative, and other health-related services.”1 The Center for the Advancement of Interprofessional Education (CAIPE) defines IPE as, “two or more professions learn with, from and about each other to improve collaboration and the quality of care.”4 According to Health Canada, they described IPE as changing the way we educate health care providers is key to accomplishing system change and to ensuring that health care providers have the necessary knowledge and training to work effectively on interprofessional teams within the evolving health care organization.5 The Interprofessional Education Consortium (IPEC), also described IPE as learning process that trains professionals through interdisciplinary education and diverse fieldwork experiences to work collaboratively with societies to meet the multifaceted needs of children, youth, and families. It provides the knowledge, abilities, and values individuals need to collaborate effectively with others as they help societies and families.6 D'amour et al showed the term ‘interprofessionality’ in the health field as the growth of a organized practice between professionals from different majors. It is the method by which professionals reflect on and develop ways of practicing that provides an integrated and organized answer to the needs of the client/family/population.7 The Journal of Interprofessional care described the IPE as various students team working together. Their collaborative contact is illustrated by the integration and modification of different majors' influences in light of input from other majors.8
It became clear that there were several closely linked terms that institutes and organizations, such as education institutions, specific health care divisions, professionals and researchers use in order to define the concept of IPE depend on extensive review of the literature related to IPE. It is crucial to determine some of the terms. They include:
COLLABORATIVE PATIENT-CENTERED PRACTICE is intended to encourage the active participation of each major in patient care. It improves patient and family-centered goals and values, offers mechanisms for unlimited communication among health care providers, and optimizes care givers participation in clinical decision making within and across majors promoting respect for disciplinary contributions of all professionals. 9
An interprofessional process of communication and decision making known as “COLLABORATION IN HEALTH CARE TEAMS” that allows the separate and shared knowledge and skills of health care providers to effect the client/patient care provided.10
EDUCATIONAL CONTINUUM is the progress through the continuum that allows for augmented knowledge difficulty and gratitude of other occupations.11
Implications of IPE:
The optimal patient care requires knowledge and assistance from many health care professions. Traditional ways of learning result in students in the health professions entering the working environment weakly prepared for clinical practice and the predictable teamwork in which they will be required to participate. Lack of knowledge of different roles and a relative absence of teamwork skills are some of the difficulties that may faced in working with multiple professions. Proper education is the ways that can be correct both of these deficits. Students who involved in IPE report an easier transition from professional school to practice.12
Methodology
Participants:
Sixty-seven students (25 from RC; 14 Nursing; 28 CLS) were recruited in this study. All surveyed students never exposed to IPE or professional experience.
Measures:
All students were asked to answer the RIPLS questionnaire. The questionnaire consisted of 3 subscales with 19 items to assess the readiness of students in interactive engaging with other students and shared learning2. The 3 subscales include teamwork & collaboration, professional identity and roles & responsibilities. The total RIPLS scores ranged from 19 to 95. All respondents were instructed on all RIPLS measured concepts. Readiness for interprofessional learning scale has been previously applied and seems to be a valid scale for measuring attitudes toward IPE for pre graduate students (23); However, its content validity was established by a panel of parts who confirmed the relevance of each item, clarity, format and ease of completion of the questionnaire and integer responses ranged between one (strongly disagree) to five (strongly agree).
Data analysis and Results:
Statistical analysis:
Data were analyzed using GraphPad Prism 5 software (GraphPad Software Inc., La Jolla, CA, USA). The Kolmogorov–Smirnov test of normality was applied. Data were presented as Means and SD. A one-way analysis of variance (ANOVA) with post hoc Bonferronitest was done to determine differences between the study groups. A p-value 0.05 was considered statistically significant.
Results:
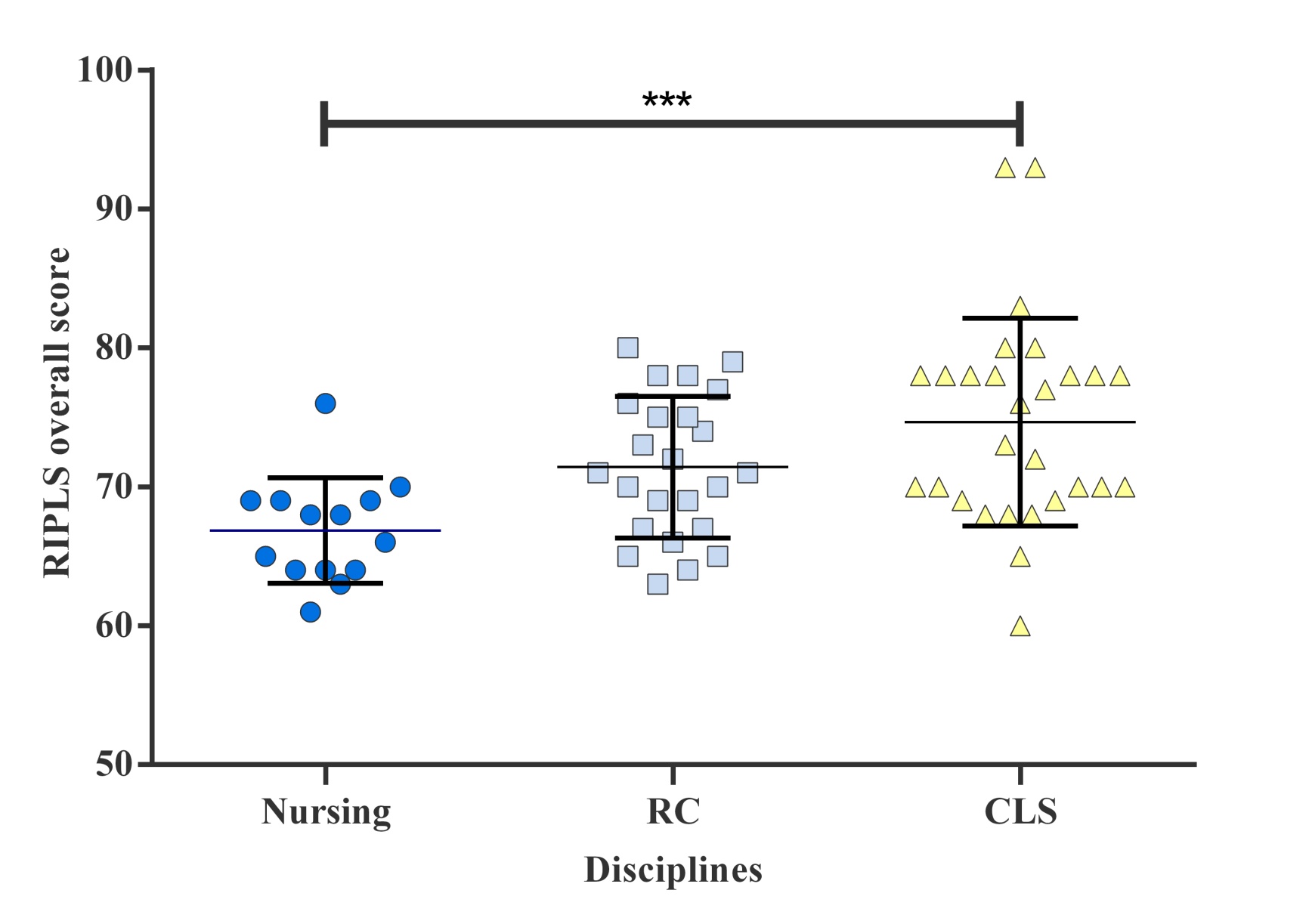
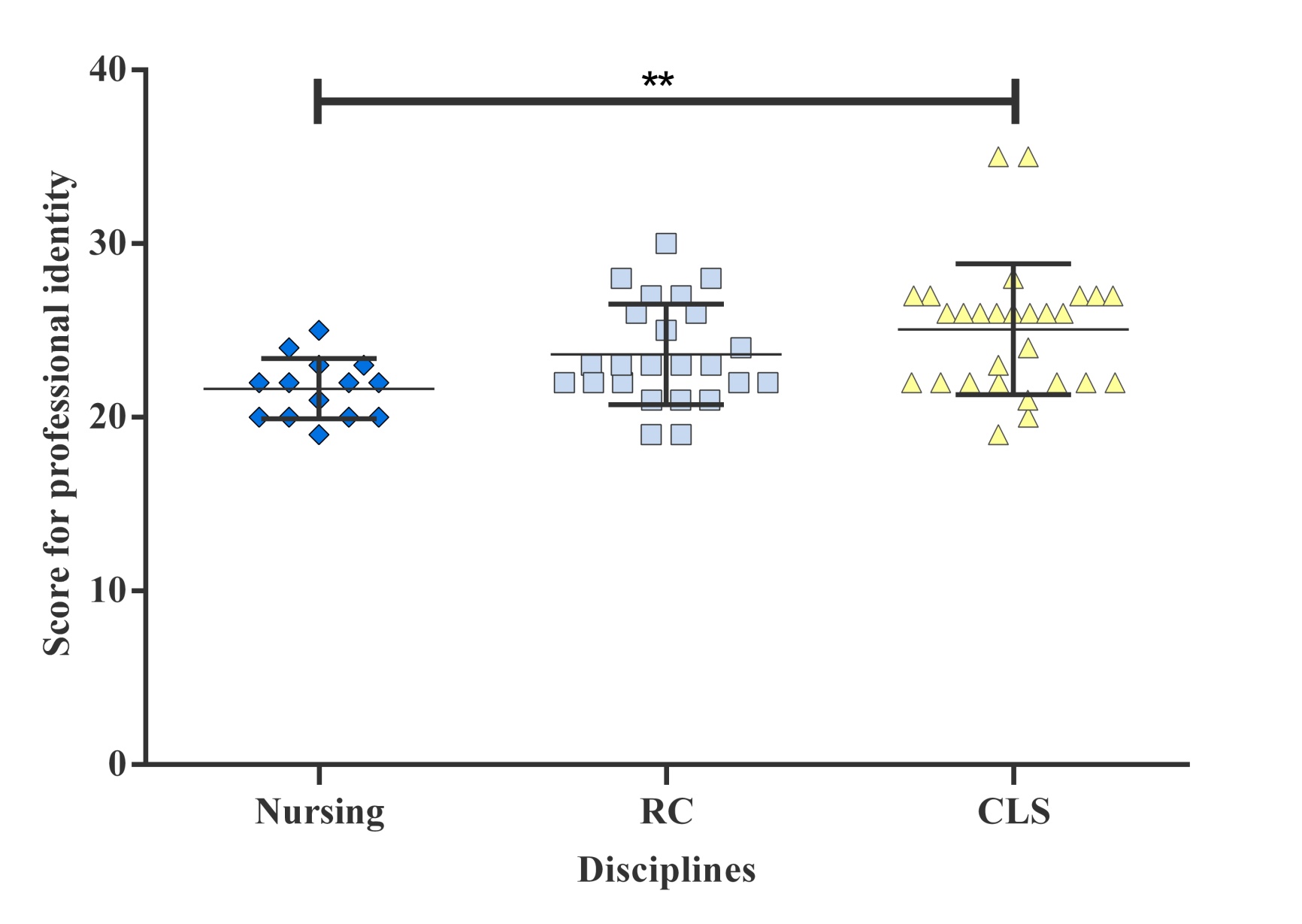
Sixty-seven students (49% male & 51% female) with the age mean of 22.24 ± 0.89, Table 1 and as illustrated in Figure 1. A total of 67 questionnaires were collected. The response rate was 100% [25(37%) RC; 14(21%) nursing; 28(42%) CLS]. The overall scores on the RIPLS were considered high, ranging from 66.9 to 74.6, Table 2. CLS scored the highest among other disciplines 74.6(79%); 71.4(75%) RC; and 66.9(70%) nursing. The one-way ANOVA revealed highly significant difference among the three groups’ mean score for overall attitudes [ANOVA p= 0.001 Table 2 and as illustrated in Figure 2]. A post hoc Bonferroni comparison indicated that the overall RIPLS scores of CLS were statistically higher than nursing [ANOVA p= 0.009].
|
Table 1. Demographic information of students enrolled in the study. |
|||||
|
Health care discipline |
Numbers |
|
Percentage |
||
|
Respiratory therapy |
25 |
37.31 |
|||
|
Nurses |
14 |
20.9 |
|||
|
CLS |
|
|
28 |
41.79 |
|
|
GENDER |
|
|
Numbers |
|
Percentage |
|
MALE |
|
|
33 |
49.25 |
|
|
FEMALE |
|
|
34 |
50.75 |
|
Figure 1. The mean score of RIPLS among the three disciplines at PSMCHS.

RIPLS mean
Teamwork &
collaboration
Roles &
responsibilities
Professional
identity
Overall
Table 2. RIPLS scores by professional disciplines.
|
Possible
min&max score |
Nursing
M(SD) |
RC
M ( SD) |
CLS
M ( SD) |
One-way ANOVA
P-value |
|
|
Subscales
|
|||||
|
Teamwork and collaboration
|
9 - 45 |
38.14(2.28) |
38.42(3.85) |
39.07(3.76) |
0.25 |
|
Professional identity
|
7 - 35 |
21.64(1.73) |
23.63(2.90) |
25.07(3.76) |
0.005 |
|
Roles and Responsibilities
|
3 - 15 |
7.07(1.14) |
9.37(2.16) |
10.5(2.58) |
0.001 |
|
Overall
|
19 - 95 |
66.86(3.8) |
71.42(5.09) |
74.64(7.47) |
0.009 |
Figure 2. Score differences for professional identity, roles & responsibilities, and overall score. of RIPLS among the three disciplines at PSMCHS. Significant differences illustrated using ANOVA with post hoc analysis. Lines represent mean±SD.

Discussion:
This study demonstrates that healthcare students in PSMCHS are ready for IPE. However, this finding concurs with the previous studies conducted across Tehran university13, Auckland university3 and Asian university14. Statement that students start a new professional course will show high level of enthusiasm for IPE. “However, a study in an Asian university reported that the existence of professional stereotype and hierarchy has affected the medical faculty staff’s and students’ willingness to participate in IPE”14. When dividing the results, scoring is different between the disciplines. Each subscale reflects certain attitudes toward IPE. CLS students score the highest while nursing students score the lowest. This study shows that CLS students are the most readiness to learn with other disciplines students when compared with RC and nursing. ANOCA shows highly significance difference for CLS students in overall scores when compared with nursing students. Professional Identity subscale shows there is a moderate significance between CLS students and nursing students. Roles and responsibility subscale shows there is high significance between CLS students and nursing, and moderate significance between RC students and nursing students. Nursing students scored the lowest in roles and responsibility that this finding is in contrast what other studies shows for nursing students in roles and responsibility subscale.
Recommendations:
This study provides a useful insight into the readiness of the PSMCHS students toward IPE. The study results suggested that healthcare students in PSMCHS showed enthusiasm toward IPE, at course start. To take advantage of this enthusiasm, we argue for the early implementation of IPE initiatives for PSMCHS students. However, it may be necessary to enhance the nursing students’ awareness of their professional identity and the benefits of IPE.
References
- World Health Organization AIECP Framework for Action on Interprofessional Education & Collaborative Practice. Geneva: World Health Organization; 2010.
- Parsell G, Bligh J . The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Med Educ 1999;33:95–100.
- Horsburgh, M, R Lamdin, and E Williamson. “Multiprofessional Learning: The Attitudes of Medical, Nursing and Pharmacy Students to Shared Learning.” Medical education 35.9 (2001): 876–883.
- Centre for Advancement in Interprofessional Education (CAIPE 2002) Interprofessional education – a definition. Retrieved April 5, 2007 from http://www.caipe.org.uk/
- Health Canada: Interprofessional Education on Patient Centered Collaborative Practice (IECPCP) Available at http://www.hcsc.gc.ca/english/hhr/research-synthesis.html; accessed April 15, 2007.
- Interprofessional Education Consortium (IPEC). (June, 2002). Creating, Implementing, and Sustaining Interprofessional Education, volume III of a series. [Electronic version]. San Francisco, CA: Stuart Foundation.
- D'amour, D., Oandasan, I. (2005). Interprofessionality as the field of interprofessional practice and interprofessional education: An emerging concept. Journal of Interprofessional Care, 19 (2), 1356- 1820. Retrieved May 4, 2007
- Clark, P.G. (1993), Journal of Interprofessional Care, 7(3), p. 219-220.
- Health Canada (2001) Social accountability: A vision for Canadian medical schools. Ottawa: Health Canada.
- Way, D., L. Jones, et al. (2001). Improving the effectiveness of primary health care through nurs practitioner / family physician structured collaborative practice. University of Ottawa: 1- 57.
- Adapted from Clark, P.G. (1993), Journal of Interprofessional Care, 7(3), p. 219-220.
- Jones L, Packard T, Nahrstedt K. Evaluation of a training curriculum for inter-agency collaboration. J Community Pract 2002;10:23–9.
- Ahmad MI, Chan SW-C, Wong LL, Tan ML, Liaw SY. Are first-year healthcare undergraduates at an Asian university ready for interprofessional education? J Interprof Care. 2013 Feb 19;
- Dargahi H, Shirazi M, Yazdanparast SA. Interprofessional Learning: the Attitudes of Medical, Nursing and Pharmacy Students to Shared Learning at Tehran University of Medical Sciences. Thrita Journal of Medical Sciences. 2012 Jun 1;1(2):44–8.
Cite This Work
To export a reference to this article please select a referencing style below:

