Introduction
Within the context of healthcare one of the most important factors is the establishment of an effective therapeutic relationship between the nurse and
patient (Foster & Hawkins, 2005). The ways in which nursing staff and patients interact can be influential in terms of information transfer, provision
of psychological support, and may also provide some therapeutic benefits in themselves (Welch, 2005). Hence, there has been a renewed focus on the
importance of how nurses interact with patients in practice, in order to enhance patient outcomes (Nursing and Midwifery Council, 2008; Sutcliffe, 2011).
Understanding the fundamental components of this relationship and how to achieve these components in practice remains a vital aspect of nurse training and
continuing professional development (Ramjan, 2004; Perraud et al., 2006).
In accordance with the perceived importance of the therapeutic relationship, the aim of this paper is to provide an evidence-based review of how this
relationship may be used in nursing practice. This will be supplemented with a reflection on personal observations made by the author, utilising a
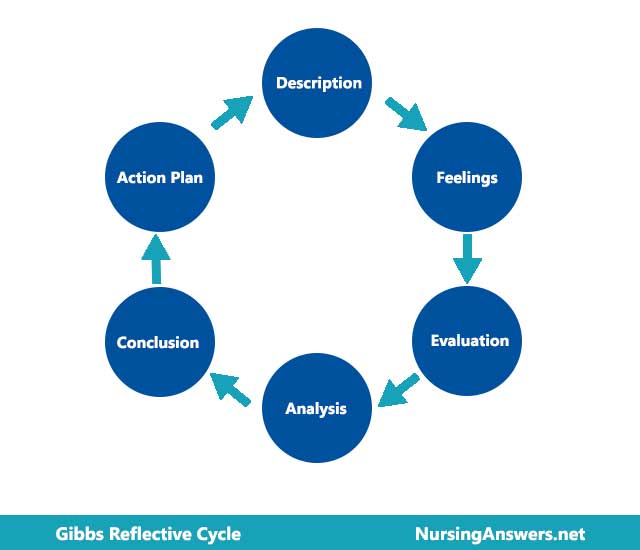
reflective model (Nielsen et al., 2007). The model in this case will be that devised by Gibbs (1988), which has been validated as a useful tool for
personal practice development and goal-setting in the clinical domain (Foster & Hawkins, 2005). This model emphasises a step-wise approach to
reflection, encompassing: description, feelings, evaluation, analysis, conclusion and action plan formulation (Gibbs, 1988). Therefore, this paper will
consider the therapeutic relationship from the perspective of a specified practice context experienced by the author, with a discussion of how practice can
be improved based on the best available evidence from the literature.
Reflection context
The main context of care that will be the focus of this essay is the elderly rehabilitation ward, where the author first encountered a number of issues
regarding the need for optimal relationships between practitioners and patients in practice. The goal of this ward is to assist elderly patients in
adapting to their functional capacities and lifestyle abilities, in order that they can achieve the maximum possible degree of quality of life in the
community setting following discharge (Routasalo et al., 2004). Consequently, numerous health professionals provide an input into the care pathway,
including physiotherapists, occupational therapists and physicians, in addition to nursing staff (Hershkovitz et al., 2007).
From the perspective of the author, there are several important aspects of this scenario that relate to the therapeutic relationship: the large increase in
personal responsibilities in terms of assisting patients with activities, the need to motivate and communicate effectively with patients to ensure that
they are able to remain psychologically motivated, and the need to coordinate personal clinical care activities with those of others to ensure the patient
journey is smooth (Siegert & Taylor, 2004). The remainder of this paper will consider the therapeutic relationship grounded within this practice
context, supplemented with personal experiences from this placement, in order to highlight these factors in greater detail.
Evidence-based reflection
Defining the therapeutic relationship
In order to fully appreciate the need for a therapeutic relationship it is important to define this relationship in a practice context. The term is often
used within the context of psychiatric or psychological therapy distribution in modern literature, although the aim of this paper is to consider the term
as a more general way in which nurses communicate and interact with patients to establish a clear clinical outcome (Bulmer Smith et al., 2009). McKlindon
& Barnsteiner (1999) suggest that the therapeutic relationship needs to be a two-way, reciprocal relationship at all times, involving nursing staff,
the patient and their family, where appropriate. There is a need to emphasise caring in this relationship, with positive communication and clear boundaries
of both personal and professional interactions (McCormack, 2004). Hence, the relationship between a nurse and patient should fit into the patient-centred
model of care, where patients are not only listened to within a clinical decision-making context, but are actively encouraged to participate in their own
care pathway (McCormack & McCance, 2006).
The therapeutic relationship encompasses three important domains of care: physical, psychological and emotional care (Pelzang, 2010). These elements may be
more profoundly encountered by nursing staff on hospital wards due to their prolonged exposure to specific patients and their in-depth interactions in the
patient care journey, when compared to other members of staff who may have less face-to-face time with individuals (Pelzang, 2010). Within the setting of
the elderly rehabilitation ward, many patients are transitioning from an acute or chronic care scenario to community care and require additional,
specialist assistance in doing so (McCormack, 2003). Consequently, nursing staff in this ward are exposed to patients for extended periods of time and need
to consider the holistic aspects of care in order to achieve successful rehabilitation (Cott, 2004). Therefore, the therapeutic relationship in this
context involves establishing the capabilities of the patient, working with the patient to achieve set goals, and ensuring that the psychological and
emotional aspects of chronic illness or disability can be managed effectively in the long term (McCormack & McCance, 2006).
Communication
In light of the definition of the therapeutic relationship within the context of rehabilitation, the remaining sections of this paper will evaluate the
core aspects involved in maintaining a therapeutic relationship, with this section focusing on communication between nurse and patient.
The specific clinical scenario the author has struggled with in the rehabilitation placement is when a patient has higher expectations than they should in
terms of their ability to perform tasks or live independently following discharge. Patients are obviously passionate in maintaining independence in the
majority of cases and this can cloud their judgement as to their genuine abilities and capabilities in functional tasks (Cott, 2004). While it is important
to acknowledge the feelings and ideas of a patient and act accordingly, it can be negligent of nursing duties not to act with the patient’s best
interests at heart (McCormack, 2003). Therefore, the nurse needs to maintain that their actions are guided by medical evidence and professional protocols,
as well as reflecting the need and desires of the patient (NMC, 2008).
Communication encompasses not only verbal communication with the patient, but is also reflected in body language and actions (Yoo & Chae, 2011). Having
an open body posture, including the avoidance of crossed arms, can help in establishing rapport, while maintaining eye contact and avoiding distractions
during conversations with patients can enhance the bond between nurse and patient (Brown & Bylund, 2008). Communication is also as much about relaying
information as it is about receiving information and therefore, nursing staff should be able to elicit patient concerns specifically and utilise these
appropriately without blocking these interactions with a one-sided approach to conversation (Yoo & Chae, 2011). The opposite is also true, whereby
overly expressive patients may limit the nurse-led component of the communication episode; both parties need to be good at communication for a perfect
mutual appreciation of ideas to occur (Sheldon et al., 2006). In practice this may be difficult to achieve, but the obligations of the nurse to facilitate
this process are a core component of the therapeutic relationship.
Communicating effectively with patients in the elderly rehabilitation setting was a massive responsibility and challenge for the author, as this was their
first encounter with such patients in this setting. The expectation of knowledge in this setting was high and it could be frustrating to patients who want
answers from a junior or inexperienced practitioner (McCormack, 2003; Leach, 2005). Hence communication needed to focus on establishing information,
sharing action plans and building general rapport that would enable the development of trust and a mutually beneficial exchange of ideas (Leach, 2005). The
author found this form of communication challenging to achieve on a routine basis within the rehabilitation setting, due to the need to balance a
motivational approach with a realistic form of communication regarding expected patient capabilities and outcomes. Hence, the reflective scenario will
focus on aspects of this particular communication episode as a component of the therapeutic relationship.
Empathy
Empathy is a cornerstone of effective communication with patients and is defined as the ability to share or identify with the emotional state of the
patient (Brunero et al., 2010). If done effectively an empathic response to patient concerns can yield a sense of shared understanding, reinforcing the
notion that the patient’s concerns are being listened to (Kirk, 2007). By establishing an empathic response with a patient, practitioners often
remark that they are better able to connect with the experiences of the patient, allowing them greater insight into how they can help the patient (Brunero
et al., 2010). Therefore, empathy is a core component of establishing a meaningful therapeutic relationship with patients in all settings.
The nurse can develop empathic communication skills in a number of ways, including through specific communication skills training (Webster, 2010). This
training often emphasises the role of open-ended questions and body language within the context of empathy, whereby nurses should ask patients specifically
about their emotions and feelings during a clinical interaction (Stickley & Freshwater, 2006). Often the process of asking a patient how they feel
about a particular reaction is sufficient to allow them to relax and become more comfortable conveying these thoughts and feelings. On the part of the
nurse, it is important to reflect these responses back to the patient by further exploring these issues and offering an active listening approach, rather
than redirecting the focus of the conversation back to more clinical matters (Brunero et al., 2010). Although it has been argued that empathy is an
intrinsic quality, which some people possess, the representation of empathy in communication is important in clinical care and should be delivered through
verbal, non-verbal and emotional communication skills (Welch, 2005).
In the present scenario, the author was able to empathise with patients on the rehabilitation ward to a high degree and many patients were frank and open
about their emotional needs and worries regarding the rehabilitation process. Often the patients’ worries were highly emotive and this affected the
author such that the patient was regarded as an object of sympathy or pity in some cases due to their hardships. This made the author feel uncomfortable
during patient interactions for a number of reasons: firstly, because it was an emotional situation, and secondly because the expectations of the patient
with regards to rehabilitation were higher than expected and it was often difficult to address these in a controlled manner. Hence, the reflective
experience demonstrates a number of feelings in this situation, which reflect problems with the therapeutic relationship.
Trust and respect
One of the primary outcomes of the therapeutic relationship is to establish a caring and trusting relationship between the nurse and patient (Brown et al.,
2006). Trust is a concept based on respect and openness within this relationship and this often takes time to establish, acting as an extension of the
professional respect a patient may hold for a nurse and vice versa (Miller, 2006). Within the context of elderly care rehabilitation, nurses need to
establish a strong bond of trust as patients will often have to make compromises in terms of assisted living devices and acceptance of their functional
limitations when attempting to optimise their quality of life (Schmalenberg et al., 2005). Unless they trust the healthcare professionals involved in their
care they are less likely to adhere to recommendations or to accept help, reducing the potential positive impacts of nursing interventions (McCabe, 2004).
Establishing trust within a therapeutic relationship requires time and demands that the practitioner is able to manage their communication skills
appropriately to ensure the patient feels that they are listened to and involved in their own care (Brown et al., 2006). Both the practitioner and the
patient must be receptive to the idea of trust within the relationship in order for this to be achieved, which often involves addressing barriers to trust,
including suspiciousness of the intentions of healthcare professionals, poor communication, and mutual respect on a personal level (Miller, 2006). When a
trusting relationship is achieved there is a greater chance that patients will be receptive to clinical interventions and nursing input, at least when
delivered on a personal level (Wolf & Zuzelo, 2006). Equally, nursing staff can trust that patients will make informed decisions about their care and
will follow guidance, when appropriate (Schmalenberg et al., 2005).
Within the present reflective context, the author felt as though there was a distinct lack of trust in the therapeutic relationship, primarily due to the
fact that a patient would often wish for their expectations to be met without heeding specific nursing advice on several occasions. This was likely
secondary to the fact that the author found it difficult to convey these ideas in a sensitive manner, while addressing the concerns of the patient in an
empathic way. Hence, it can be perceived that the patient and nurse did not enter a trusting relationship, as communication between the two was suboptimal
(McCabe, 2004). However, on a more positive note, the relationships formed with patient during the initial days on placement were friendly and demonstrated
a degree of mutual respect, which is an important facet of the therapeutic relationship (Stickley & Freshwater, 2006). Hence, there were positive and
negative aspects to the therapeutic relationships formed in practice during this placement, according to a reflective evaluation.
To make sense of this situation, the author analysed these positive and negative factors within this context. What was clear to the author was that the
communication skills that had been utilised so far in therapeutic relationship building relied heavily on patient factors, rather than nursing input.
Hence, there was an imbalance in the way information was presented and received within this relationship, to the detriment of the therapeutic journey. The
reasons for poor communication and trust establishment stemmed from multiple factors, including the younger age of the author compared to patients,
relative inexperience on the part of the author, and the highly charged emotional nature of interactions in this setting. Therefore, it was clear that one
of the main factors that was missing in the therapeutic relationships was the projection of a strong professional identity, which could guide the patient
towards a suitable clinical outcome and would assist in developing the appropriate communication tools for the rehabilitation process.
Professional values
While it is clear that the need for the therapeutic relationship stems from a desire to form a constructive clinical partnership with a patient in a
specific context, there is also a professional responsibility to engage patients in this manner in practice (Chitty & Black, 2007). The Nursing and
Midwifery Council (2008) advocate communication, trust, dignity and respect during the treatment of all patients as a fundamental aspect of care delivery
and therefore establishing a therapeutic relationship can be considered a core aspect of all nursing practice (Fahrenwald et al., 2005).
However, within the context of effective nursing practice it is recognised that there is a need to respect the personal boundaries of the patient and to
act as a professional rather than a friend in most cases (Rushton, 2006). Professionalism in the context of rehabilitation care includes the need to be
realistic with regards to patient expectations, while ensuring appropriate levels of motivation and commitment to a therapeutic plan (Fahrenwald et al.,
2005; Rushton, 2006). For some practitioners, an overly empathic response to patients and their condition can lead to sympathy and warped clinical decision
making processes, often favouring the opinion of the patient over established guidance (Bulmer Smith et al., 2009). This is likely to have a detrimental
impact on the patient in the long term and should be avoided as a result.
Within the Gibbs reflective cycle (1988), the author has noted that one of the main conclusions that can be drawn from working within the rehabilitation
sphere is that maintenance of professional values and boundaries is essential to avoid becoming overly emotional or inappropriately involved in patient
care (Stickley & Freshwater, 2006; Baker et al., 2008). The author should try not to become too attached to patients during their care journey in order
to make an objective assessment of their capabilities and therapeutic needs, as relying too heavily on the opinions and desires of the patient can yield
unsatisfactory results in the long term, particularly when these go against recommended practice (Leach, 2005). By applying more rigorous professional
boundaries in the future, and focusing on explaining complex situations from a nursing perspective, rather than yielding to the patients’ wishes, the
author can improve their contribution to practice in the long term and enhance the patient journey through rehabilitation.
Conclusion
In summary, this paper has considered the personal experiences of the author within the context of a reflective practice episode in order to appreciate the
value and tenets of the therapeutic relationship in practice. The core components of the therapeutic relationship, as they relate to the present scenario,
have been discussed with reference to the evidence base in order to develop a constructive reflective episode reflecting a description of events, feeling,
evaluation, analysis and conclusion.
The process of reflection should yield a suitable action plan and in this case the author feels that they should engage with patients in a more
professional manner, ensuring that they maintain an empathic and understanding approach to care while maintaining nursing boundaries. In order to achieve
this, communication skills should be enhanced in the future, through attendance at specific communication skills courses, in order to become more
comfortable in managing potential conflicts or hostility. This should enhance the therapeutic relationship and ensure that future patients can be managed
in a manner that benefits all members of the relationship. Furthermore, it is important that the author is aware of how other colleagues maintain
professional boundaries and can direct their relationship accordingly in practice, and consultation with colleagues on this point would be a useful
learning tool. On completion of these tasks, the author should therefore feel better prepared to engage with patients in a meaningful way, ensuring that
trust is developed and that patients have an effective care process, in all areas of care.
References
Baker, C., Pulling, C., McGraw, R., Dagnone, J. D., Hopkins‐Rosseel, D., & Medves, J. (2008). Simulation in interprofessional education for
patient‐centred collaborative care. Journal of Advanced Nursing, 64(4), 372-379.
Brown, D., White, J., & Leibbrandt, L. (2006). Collaborative partnerships for nursing faculties and health service providers: what can nursing learn
from business literature?. Journal of Nursing Management, 14(3), 170-179.
Brown, R. F., & Bylund, C. L. (2008). Communication skills training: describing a new conceptual model. Academic Medicine, 83(1),
37-44.
Brunero, S., Lamont, S., & Coates, M. (2010). A review of empathy education in nursing. Nursing Inquiry, 17(1), 65-74.
Bulmer Smith, K., Profetto-McGrath, J., & Cummings, G. G. (2009). Emotional intelligence and nursing: An integrative literature review. International Journal of Nursing Studies, 46(12), 1624-1636.
Chitty, K. K., & Black, B. P. (2007). Professional nursing: concepts & challenges. London: WB Saunders Co.
Cott, C. (2004). Client-centred rehabilitation: client perspectives. Disability & Rehabilitation, 26(24), 1411-1422.
Fahrenwald, N. L., Bassett, S. D., Tschetter, L., Carson, P. P., White, L., & Winterboer, V. J. (2005). Teaching core nursing values. Journal of Professional Nursing, 21(1), 46-51.
Foster, T., & Hawkins, J. (2005). The therapeutic relationship: dead or merely impeded by technology?. British Journal of Nursing, 14
(13), 698-702.
Gibbs, G. (1988). Learning by doing: a guide to teaching and learning methods. Further Education Unit. Oxford Polytechnic: Oxford
Hershkovitz, A., Kalandariov, Z., Hermush, V., Weiss, R., & Brill, S. (2007). Factors affecting short-term rehabilitation outcomes of disabled elderly
patients with proximal hip fracture. Archives of Physical Medicine and Rehabilitation, 88(7), 916-921.
Kirk, T. W. (2007). Beyond empathy: clinical intimacy in nursing practice.Nursing Philosophy, 8(4), 233-243.
Leach, M. J. (2005). Rapport: a key to treatment success. Complementary Therapies in Clinical Practice, 11(4), 262-265.
McCabe, C. (2004). Nurse–patient communication: an exploration of patients’ experiences. Journal of Clinical Nursing, 13(1),
41-49.
McCormack, B. (2003). A conceptual framework for person‐centred practice with older people. International Journal of Nursing Practice, 9(3), 202-209.
McCormack, B. (2004). Person‐centredness in gerontological nursing: an overview of the literature. Journal of Clinical Nursing, 13
(s1), 31-38.
McCormack, B., & McCance, T. V. (2006). Development of a framework for person‐centred nursing. Journal of Advanced Nursing, 56
(5), 472-479.
Miller, J. F. (2006). Opportunities and obstacles for good work in nursing.Nursing Ethics, 13(5), 471-487.
Nielsen, A., Stragnell, S., & Jester, P. (2007). Guide for reflection using the clinical judgment model. The Journal of Nursing Education, 46(11), 513-516.
Nursing and Midwifery Council (2008). Code of Professional Conduct. Available at: http://www.nmc-uk.org/aDisplayDocument.aspx?documentID=5982 [accessed 6 th October 2014]
Pelzang, R. (2010). Time to learn: understanding patient-centred care. British Journal of Nursing, 19(14), 912.
Perraud, S., Delaney, K. R., Carlson‐Sabelli, L., Johnson, M. E., Shephard, R., & Paun, O. (2006). Advanced practice psychiatric mental health
nursing, finding our core: The therapeutic relationship in 21st century. Perspectives in Psychiatric Care, 42(4), 215-226.
Ramjan, L. M. (2004). Nurses and the ‘therapeutic relationship’: Caring for adolescents with anorexia nervosa. Journal of Advanced Nursing, 45(5), 495-503.
Routasalo, P., Arve, S., & Lauri, S. (2004). Geriatric rehabilitation nursing: developing a model. International Journal of Nursing Practice, 10(5), 207-215.
Rushton, C. H. (2006). Defining and addressing moral distress: tools for critical care nursing leaders. AACN Advanced Critical Care, 17
(2), 161-168.
Schmalenberg, C., Kramer, M., King, C. R., Krugman, M., Lund, C., Poduska, D., & Rapp, D. (2005). Excellence through evidence: securing
collegial/collaborative nurse-physician relationships, part 2. Journal of Nursing Administration, 35(11), 507-514.
Sheldon, L. K., Barrett, R., & Ellington, L. (2006). Difficult communication in nursing. Journal of Nursing Scholarship, 38(2),
141-147.
Siegert, R. J., & Taylor, W. J. (2004). Theoretical aspects of goal-setting and motivation in rehabilitation. Disability & Rehabilitation, 26(1), 1-8.
Stickley, T., & Freshwater, D. (2006). The art of listening in the therapeutic relationship: The role of the modern mental health nurse is becoming
more technical when, argue Theodore Stickley and Dawn Freshwater, what would really benefit patients is the often misunderstood art of listening. Mental Health Practice, 9(5), 12-18.
Sutcliffe, H. (2011). Understanding the NMC code of conduct: a student perspective. Nursing Standard, 25(52), 35-39.
Webster, D. (2010). Promoting empathy through a creative reflective teaching strategy: a mixed-method study. The Journal of Nursing Education, 49(2), 87-94.
Welch, M. (2005). Pivotal moments in the therapeutic relationship. International Journal of Mental Health Nursing, 14(3), 161-165.
Wolf, Z. R., & Zuzelo, P. R. (2006). “Never again” stories of nurses: dilemmas in nursing practice. Qualitative Health Research, 16(9), 1191-1206.
Yoo, M. S., & Chae, S. M. (2011). Effects of peer review on communication skills and learning motivation among nursing students. The Journal of Nursing Education, 50(4), 230-233.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "gibbs reflective cycle"
Gibbs' Reflective Cycle was developed by Graham Gibbs in 1988 to give structure to learning from experiences. It offers a framework for examining experiences, and given its cyclic nature lends itself particularly well to repeated experiences, allowing you to learn and plan from things that either went well or didn’t go well. It covers 6 stages.
Related Articles