Maariyah Iqbal
- INTRODUCTION
In this chapter, the background of the problem will be presented. This will be followed by the research problem as well as the particular purpose and question, specifically highlighting why the topic area chosen is of great interest.
1.1 Background
The National Health Service (NHS) provides healthcare for all citizens within the United Kingdom (UK) and it is funded by taxes; the core principles of the NHS are to meet the needs of everyone and it is based on a patient’s clinical need(s) and not on their ability to pay (Slee et al., 2008). The National Institute for Health and Care Excellence (NICE) 2017 provides guidance on how to promote good health as well as prevention and treatment of health. The NHS in England receives over 1 million patients approximately every 36 hours, and this organisation employs over an estimated of 1.5 million people making it to one of the top five world’s largest workforces (NHS Choices, 2016). Despite the success of the services of the NHS there is more work needed to continue to improve services and deliver care (NHS Improvement, 2015). Therefore, the NHS continues to remain under pressure as there are further increases in demand for care (NHS Improvement, 2015). This means an increased demand for all health care practitioners, including Radiographers. The demand for services means increased waiting times, may lead to increased work pressure.
To improve services the department of health set an ongoing standard for the NHS where the patient spends four hours or less in the Accident and Emergency (A&E) from arrival to admission or discharge (House of commons, 2005). However, a report from the Kings Fund (2016) shows that A&E departments are soaring to six million patients attending, this is placing a huge strain on services making it difficult to meet this target. Data from the briefing paper from Houses of Parliament (Appendix 1) show that in some areas such as; Greater London and Manchester there was 26-32% of patients that waited for more than four hours.
Increased demands of work continue to leave the NHS under pressure as there are further increases in demand for care, and issues with being able to discharge medically fit patients (NHS Improvement, 2015). Extracted from the quarterly data summary issue (2008), in England one of the main issues surrounding discharging of patients is that they are still awaiting results of tests and discharge forms are not being complete in time (NHS England, 2015). Good planning in regards to discharging is imperative as it will improve patient flow and satisfactory, and can also decrease the chances of patients being readmitted again (Family Caregiver Alliance, 2016).
The department of health puts forward ten operating principles in regards to discharging, one of which is the multidisciplinary team working together to plan care, and make decisions on the process and timing of discharging (Nursing Standard, 2010). Professionals can extend their roles beyond their scope of practice, and can be further trained to contribute to discharging of patients which can ease pressures of other staff in the A&E department such as; doctors. Research also taken from (Grayson’s, no date) showed that a search search by the NHS Litigation Authority for descriptions of failure/delay diagnosis or incorrect diagnosis in 2014/15. The results of the response showed, 183 mentions of fractures. This highlighted that misinterpretation of images was also one of the factors of delayed discharge.
In the context of clinical imaging, radiographers reporting on images is well established in the UK and it makes a major contribution to clinical imaging services and contribution to multidisciplinary care (The Society of Radiographers, 2017). A study was carried out by Snaith (2007) whereby three reporting radiographers were trained to discharge patients or refer to A&E (Accident & Emergency) for further assessment. The results were significant and showed that that 1760 examinations were reviews, 5% of these were discharged and 2% were referred. However, the number of patients recalled due to incorrect interpretation was decreased by 52% in those 4 months compared with the previous 3 years’ data (The College of Radiographers, 2017). This shows that Radiographers can extend their role not just within clinical imaging services, but also outside of their department by contributing to the management of patients and decreasing the risk of radiographic misinterpretation.
Initially, radiographers produce high quality images of the body, screen for abnormalities and take part in surgical examinations to identify and diagnose injury and disease (The National Careers Service, 2016). Thus, being able to distinguish between normal and abnormal appearances that are evident on images is one of the standards that should be met by a radiographer (HCPC, 2017). The red dot system is implemented by radiographers in emergency departments to highlight acute abnormalities. Radiography Abnormality Detection Schemes (RADS) is one of the ways in which radiographers interpret images produced. They are able to make an initial interpretation on images obtained which gives them a proactive role in the diagnostic process, and assists doctors in the correct interpretation of radiographic images (SoR, no date).
However, despite there being a set standard for radiographers to meet. Clinical imaging services are under increasing pressure year on year as radiographers are required to enhance the quality of the image, productivity, which is difficult due to staffing levels (Beardmore, 2013). In addition, these problematic areas can have a knock-on effect on other significant areas within the NHS; such as supervision of newly qualified and students that are training there. After research, the author has found that there is a variation in of training in hospitals and university, as the time that students spend on clinical placement has found to be different. The University of Leeds (2017) 50% of the course is in clinical placement, however, students at the Birmingham City University (2017) spend 35% of their course on clinical placement. This highlights there is a variation in clinical placement and this could affect the new registrants that may not be equally competent once qualified or even meet a certain threshold.
Ultimately, all students must meet specific standards in order to receive their Health and care professions council (HCPC) registration to be able to become and work as a newly qualified radiographer (the Society and College of Radiographers, 2017). The HCPC is an independent regulator, it regulates 15 other professions besides radiographers, they are established to protect the public by maintaining a register of all those that hold the protected title of “social worker”, so that registrants practice safely, legally and effectively (University of Bedfordshire, 2017). The HCPC set standards, approve courses that meet those standards, register those who pass the courses and clinical competencies, and hold them to their standards. In relation to diagnostic radiography, they set standards of proficiency for all radiographers which set out safe and effective practice, it covers areas in depth; so, all radiographers should be able to maintain fitness and practice (Health and Care Professions Council, 2013), this is elaborated on further from on section 3 to 3.3 (Appendix 2). It is vital that all standards that are discussed and mentioned, are met in order to be able to receive the registration.
Additionally, once qualified and registered under the HCPC; a newly qualified radiographer is supported on their job role by a period of preceptorship. Although there is no ‘defined’ period of preceptorship it is support for those that have newly qualified. It is a period of adaptation to a job role, consolidating knowledge and skills till he or she is able to work as an autonomous radiographer. (The Society and College of Radiographers, 2017).
Moreover, as there is a shortage of staff as the NHS staff survey conducted in 2013 that showed that the staff stated that they felt under pressure and over worked, as they were working extra hours increasing from 69.7% to 70.5% from the previous year (UNISON, 2014). This highlights that training students, or even supporting staff within an organisation can be difficult as staff can be difficult due to staffing issues and work pressures. However, from research the author has found that an increase of patients will mean an increase in the range and capability of clinical images which will consequent needs of training radiographers to safely extend their roles.
Moreover, initial training whereby it leads to either role extension, or continuing professional development are integral to radiographic practice (The Society of Radiographers, 2017). Radiographers are expected to build on their postgraduate qualifications and clinical managers are encouraged to embed this use of learning tool in radiographer’s personal development reviews (The Society of Radiographers, 2017). In context, of this radiographer are able to extend their roles by Radiographer Abnormality Detection Schemes (RADS). RADS allows radiographers to red dot images which put a mark on the image suggesting there is an abnormality present (Carver and Carver, 2012). Thus, making it easier for the clinician/referrer to look at when reporting on it. Being able to implement RADS can help to reduce errors and improve accuracy (Chan, 2007). The aim of this system is to assist emergency departments, especially when there is a shortage of staff such as; radiologists that do the reporting which helps location of the abnormality to be commented on sooner (Coelho and Rodrigues, no date).
The basis of the problem around RADS will now be further discussed, which will be able to give an insight of the purpose of this research.
1.1 Research Problem
RADS has become an accepted norm for radiographers (Carver and Carver, 2012). Before implementing RADS, it is essential that radiographers are able to evaluate and manipulate images for quality purposes which allows them to the be able to understand the image to implement RADS.
A study carried out by Brearly et al., 2005 which looked at the accuracy of radiographers use of the red dot system with and without training on this area, and whether or not they can assess how a normal image would be presented. There was a significant improvement found in the sensitivity for detecting abnormalities, however, there was no change in the actual specificity. This highlights that, after training took place radiographers were able to red dot more images than before the training took place, however, the number of radiographs that radiographers selected as being normal there was no change found. Therefore, the validity of this study is limited as it not clear on whether the sample of radiographs before and after training were comparable. However, Hardy and Culpan (2007) carried out a study whereby they assessed radiographers before and after training in their ability to red dot images. They introduced a training programme for 10 weeks, the results showed that their accuracy as a group increased for 89.9% to 93% and their sensitivity (number of abnormal images) however, the specificity (number of normal images) decreased slightly from 96.4% to 96.1%. The study highlights, that although the results are not statistically significant, with appropriate training it can have an overall positive effect on the use of radiographer abnormality detection schemes.
Despite there being a significant amount of research on this topic area, there is no clear evidence whether or not training improves the implementation of red dotting.
1.1 Research purpose and question
The purpose of this research is to give an insight on whether training improves newly qualified radiographers in implementing RADS in practice or not. This case will be further developed with the use of a literature review.
References
Birmingham City University. (2017). Diagnostic Radiography: BSc (Hons). Available: http://www.bcu.ac.uk/courses/diagnostic-radiography-2017-18. Last accessed 9th Feb 2017
Net Doctor. (2017). What is the NHS?. Available: http://www.netdoctor.co.uk/health-services/nhs/a4489/what-is-the-nhs/. Last accessed 9th Feb 2017.
NHS Choices . (2016). The NHS in England. Available: http://www.nhs.uk/NHSEngland/thenhs/about/Pages/overview.aspx. Last accessed 9th Feb 2017.
NHS Improvement. (2015). NHS providers working hard, but still under pressure . Available: https://improvement.nhs.uk/news-alerts/nhs-providers-working-hard-still-under-pressure/. Last accessed 9th Feb 2017.
Teesside University. (2017). BSc (Hons) Diagnostic Radiography. Available: https://www.tees.ac.uk/undergraduate_courses/Health_&_Social_Care/BSc_(Hons)_Diagnostic_Radiography.cfm. Last accessed 9th Feb 2017.
The Kings Fund. (2017). Demand for NHS services soars to record levels. Available: https://www.kingsfund.org.uk/press/press-releases/demand-nhs-services-soars-record-levels. Last accessed 9th Feb 2017.
The National Careers Service. (2016). Radiographer. Available: https://nationalcareersservice.direct.gov.uk/job-profiles/radiographer. Last accessed 9th Feb 2017.
UNISON. (2014). Running on empty NHS staff stretched to the limit. Available: https://www.unison.org.uk/content/uploads/2014/04/On-line-Catalogue222452.pdf. Last accessed 9th Feb 2017.
Parliamentary. (no date). Accident and Emergency Statistics: Demand, performance and pressure. Available: http://researchbriefings.parliament.uk/ResearchBriefing/Summary/SN06964. Last accessed 9th Feb 2017.
The Health and Care Professions Council. (2017). Standards of Proficiency. Available: http://www.hpc-uk.org/assets/documents/10000DBDStandards_of_Proficiency_Radiographers.pdf. Last accessed 9th Feb 2017.
The Society of Radiographers. (no date). Radiographer abnormality detection schemes in the trauma environment. Available: http://www.sor.org/system/files/article/201109/ab_detection_clinical_260607.pdf. Last accessed 9th Feb 2017.
http://repositorio.chporto.pt/bitstream/10400.16/842/1/CR11a.pdf
https://www.publications.parliament.uk/pa/cm200405/cmselect/cmpubacc/445/445.pdf
http://www.nrls.npsa.nhs.uk/resources/?EntryId45=59854
http://www.radiographyonline.com/article/S1078-8174(05)00159-8/abstract
http://www.graysons.co.uk/advice/the-top-misdiagnosed-conditions-in-nhs-hospitals/#misdiagnosed
https://www.caregiver.org/hospital-discharge-planning-guide-families-and-caregivers
http://journals.rcni.com/userimages/ContentEditor/1373367855606/Discharge-planning.pdf
http://www.radiographyonline.com/article/S1078-8174(03)00069-5/abstract
http://www.radiographyonline.com/article/S1078-8174(05)00159-8/abstract
Appendices
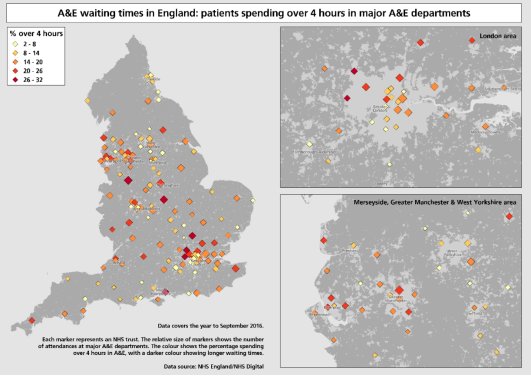 Appendix 1: A&E waiting times in England: Patients spending over 4 hours in major A&E departments
Appendix 1: A&E waiting times in England: Patients spending over 4 hours in major A&E departments
(Parliamentary, no date)
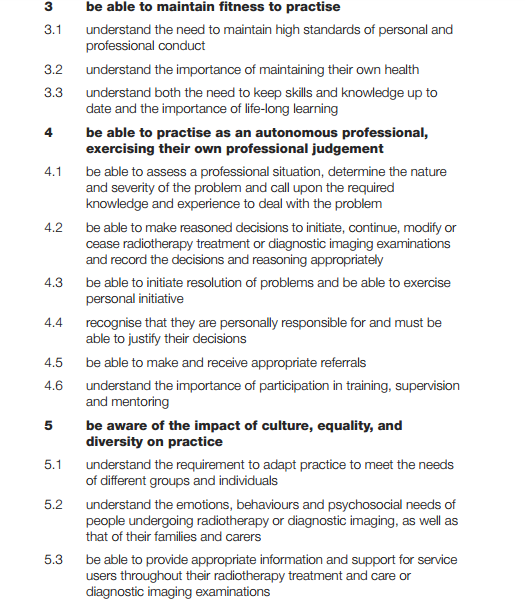 Appendix 2
Appendix 2
(Health and Care Professions Council, 2013).
Further websites could be used
https://www.researchgate.net/publication/232221820_Evaluating_the_true_clinical_utility_of_the_red_dot_system_in_radiograph_interpretation could be used for intro and literature review
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "radiography"
Radiography: specialisation in the use of radiographic, radiation therapy and magnetic resonance equipment to administer radiation treatment and produce images of body structures for the diagnosis and treatment of injury and disease.
Related Articles