Introduction:
I will be reflecting upon my experience of a mobile radiography procedure using the ‘John’s Model of Reflection’. This framework allows the person to identify what they want to achieve using a series of five questions before entering the clinical environment and from the outcomes that meet or did not meet certain standards; an evaluation can be completed to reflect upon the clinical performance as a practitioner, and how to improve where we may not be succeeding. I will reflect upon my day spent within mobile radiography within intensive care unit. I will refer to John’s model as it involves the roles of others within an experience to understand the experience within a context (Jaspar, 2013).
Description of the Experience:
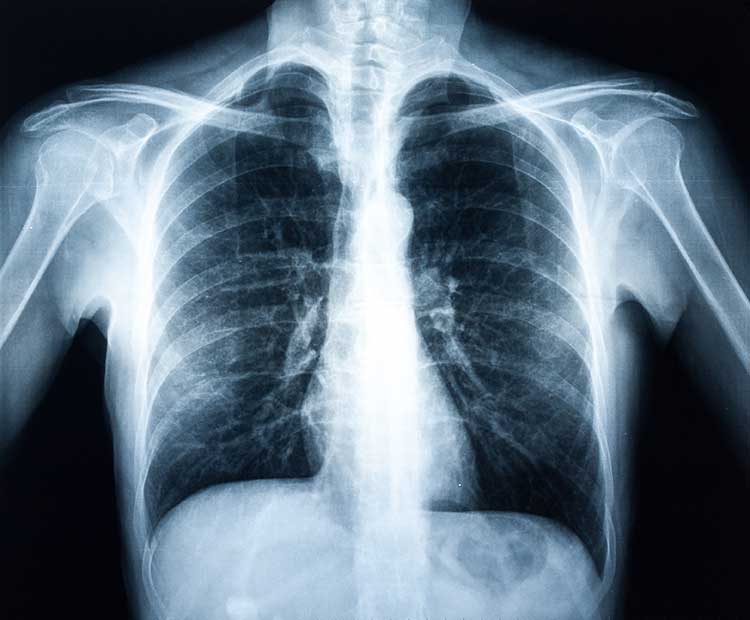
The day I spent on mobile radiography procedures was within departments such as the special baby care unit, recovery wards, and intensive care unit (ICU). The experience I will reflect upon is the mobile request within ICU. The request was for a male requiring a chest x-ray querying an infection. However, the male was sedated, heavily monitored and extremely obese. The mattresses have got pockets which enables easier positioning of a detector bag that can be passed behind the patient with minimally moving the patient.
However, as the man was sedated and obese it made positioning him to ensure an optimal image very challenging. He was leaning to one side; pillows and foam pads were used to help straighten the man – this was to ensure the image was not lordotic, it was straight, and the full chest was visualised. It was left to the radiographer and I to position this man as best as we could; no other member of staff offered or replied to our request for help. The staff within ICU only intervened when we asked about the monitoring equipment. The chest x-ray required as much of the equipment out of field of view so equipment which wouldn’t compromise the patient was moved. The deep sedation and weight of the male meant efficiency was required to obtain an image as the ancillary equipment used couldn’t withstand the male for any length of time.
Reflection:
During this procedure I was trying to achieve effective communication with the radiographer for correct preparation of equipment, positioning of the patient was done correctly and no compromise to the patients monitoring or condition. This was my first time within ICU as a student, so I wanted to ensure I was conducting myself correctly; the patient’s best interests and the appropriate protocols were being met. The communication between the radiographer and I ensured patient safety and established a trust, together we both had the same intentions of this examination and both sought the same outcome.
My growing confidence came sooner than anticipated; this was due to the need to quicken my way of working and adapting to a new environment. But most importantly the lack of help from the ICU team. It made me aware of how working in this environment independently is challenging. I intervened by prepping the x-ray equipment and communicating what equipment could be safely moved before the examination began. The radiographer soon seen how I adapted to working within this environment and together we started collaborating on how we would conduct this procedure with the limited support we had.
Inter-professional work is a process which is being implemented for team work within different health care professionals to provide excellent communication to ensure a quality health service is provided (Munro & Henwood, 2013). However, the lack of support from the ICU team made the examination more challenging. The weight and the unconsciousness of the male created great difficulty for only two people. The patient’s conditions within ICU is time critical; if efficiency and accuracy is not conducted it could compromise a patient’s life. Within ICU sophisticated equipment is used to monitor, maintain, and support a patient’s bodily functions until they recover; ventilators to help with breathing, IV lines for nutrition, fluids and medicine, and drains to remove any fluid or blood build up from the body (NHS, 2016) – any movement or disruption will result in the patient’s condition being compromised.
As there was no response to my appeal for help from the ICU team it led to the patient being in a more compromised position and led to additional images being taken due to insufficient quality which resulted in the patient receiving a higher radiation dose. In the NHS, due to the lack of good inter-professional working and communication it has resulted in approximately 70-80% of errors within healthcare by human factors (Xyrichis & Ream, 2008).
My first time within ICU was overwhelming – the different types of sounding equipment monitoring the severely ill patients, and the care members instant response if an alarm sounded if a measurement was not within an acceptable range – can be frightening (Valentino, 2015). However, the circumstances and absence of multi-disciplinary help made me feel determined to help in any way I could and provide a high standard of care to this critically ill patient.
Afterwards, I had a feeling of guilt – as the patient was sedated, this was the first time as student I was unable to communicate or interact with the patient. They were not necessarily consenting to the examination and undergoing radiation unknowingly. I had always been taught to communicate with patients to gain verbal consent to the examination, to understand the risks associated with radiation exposure (Whitley, 2017) However, despite the risks associated the patient should understand the benefits and the nature of the examination.
The feeling of anger started to arise within me – the non-existing help from the ICU team meant the patient’s condition was at risk of deteriorating or suddenly changing. Munro and Henwood (2013) established the lack of good inter-professional working resulted in poorer health outcomes, higher death rates and medical errors. Thus, there was a discrepancy with the patient’s welfare during the examination.
Influencing factors:
Within myself; I knew I wanted to ensure the best outcome for the patient. The time critical nature of ICU made me very aware I had to act quickly and ensure optimal patient safety. Since this was my first time within this department, I wanted to ensure I was making the correct impression; I adapted and worked despite the challenges that occurred. My decision making was influenced by creating a prior plan of communicating how technique was to be adapted and how the equipment and patient was to be positioned or moved to not impede image quality or compromise the patient.
The state of the patient and how the radiographer was solely conducting the procedure influenced my decision making to intervene. The limited support from the ICU team influenced my decision of intervening and assisting the radiographer. Good communication and effective listening between the radiographer and I ensured the common goal of best patient care was achieved (Ehrlich, 2013).
The condition of the patient influenced my decision making – heavy sedation and the obesity created a greater risk of deterioration. Adverse reaction to sedation can vary but the most common include hypotension, amnesia, post-traumatic stress disorder and reduction in gut motility (Woodrow, 2019). This knowledge allowed for the requests from the radiographer to be completed efficiently and effectively – ensuring optimum patient safety and image quality.
Could I Dealt with it better:
Before the procedure the radiographer and I could have had a conversation with the ICU team; explaining what needed to be achieved and how it would be conducted. It should have been discussed what type of help was required. It could be queried if the examination was justified; was it necessary for the image or could it be postponed till the patient was more stable. Whitley (2017) outlined that justification is a key aspect to ensure it is completed only when required for a medical diagnosis and treatment and whether the benefits outweigh the risks associated; this includes considering the medical history of the patient, the radiation protection and the request.
Prior discussion could have improved how the examination was conducted however the time critical nature of ICU means efficiency is high priority. The role of the radiographer and I was to ensure time was spent ensuring the optimal image quality and there was no compromise to the patient’s condition. The poor acknowledgement of help from the ICU team could have led to the radiographer refusing to complete the examination as it was deemed the safety of the patient could be compromised.
If the examination had not been completed when it was requested, it could have delayed the diagnosis and treatment for the patient. This could then have led to the patient in a more compromised and life-threatening situation.
Learning:
This experience made me feel anxious about returning to ICU. Whilst I should have benefitted from the time spent within ICU; it made me uneasy about returning because of the shortfall of communication between inter-professional teams. Despite both teams having identical intentions of achieving best patient care; the discrepancy could have resulted in poorer health outcome. However, despite the challenges it made me feel determined to guarantee patient wellbeing and safety throughout my learning. Whilst adapting my technique safely to suit the patient to ensure image quality is still optimum.
For future practice I will communicate with those involved in the procedure how it must be conducted and communicate what is needed from everyone involved. Furthermore, information should be shared amongst professional bodies to ensure everyone involved is aware of what intentions are to be achieved. Thus, ensuring the patient and the staff involved have optimum safety.
I will continue to achieve optimal patient wellbeing despite of challenges and being within a new environment. Regardless of the fact I had never been within this environment and the shortfall of multi-disciplinary help, optimum delivery of care and image quality is the priority no matter what the department and this will continue throughout my career.
The actions I took were for the benefit of both the patient and the radiographer. The radiographer was unable to position and perform the examination solely – the non-existing help from the ICU prompted myself to intervene when the radiographer requested my help to move the patient and equipment. The welfare of the patient was also my priority and I believed the way I had supported the way I did ensured no compromise to the patient’s condition. This experience has allowed me to quicken my adaption to a new environment for future practice – despite the new surroundings the patient’s welfare is always the priority.
Conclusion:
To conclude using John’s Model of Reflection I reflected upon my mobile radiography procedure within ICU. This experience of poor communication and the shortfall of inter-professional collaboration enabled me to appreciate the need for a strong multi-disciplinary team and effective communication to ensure the best delivery of patient care.
For future practice, I will ensure effective communication is established for the purpose of patient safety and correct delivery of care. Good inter-professional working collaborates expertise knowledge to provide an optimal service. Effective communication between disciplinaries ensures progress is established through the quality patient safety and care service. The qualities required for successful communication is trust and respect of other disciplinaries – everyone relies on the other to ensure the wellbeing of the patient is guaranteed. Everyone involved must be equally as determined to achieve the common goal and to co-operate when issues arise. I will continue throughout my time as a student onto when I qualify to perform and improve upon this goal; establishing a good communication between inter-professionals ensures a trust of intentions to achieve the common goal. Thus, everyone involved should be appropriately informed to guarantee an efficient and accurate diagnosis for the patient. I will plan my intentions before conducting an examination; establishing the challenges, communicating with those involved and assess requirements needed to overcome and achieve the goal.
References:
- ENRLICH, R.A., 2013. Patient Care. In: Patient Care in Radiography Elsevier, pp. 97-131.
- JASPAR, M., 2013. Frameworks for Reflection. In: Beginning Reflective Practice Cengage Learning, pp. 86-99.
- MUNRO, L. and HENWOOD, S.M., 2013. Inter-professional Communication. In: RAMLAUL, A. and VOSPER, M. eds., Patient Centered Care in Medical Imaging and Radiotherapy Elsevier, pp. 21-29.
- NHS, 2016. Intensive Care NHS. [Viewed 24th January 2019]. Available from: https://www.nhs.uk/conditions/intensive-care/.
- VALENTINO, D., 2015. Intensive Care Unit (ICU) Equipment [viewed 24th January 2019]. Available from: http://www.healthcommunities.com/before-after-surgery/equipment.shtml.
- WHITLEY, A.S., 2017. Patient Identity and Consent. In: Clark’s Pocket Handbook for Radiographers CRC Press, pp. 19-20.
- WOODROW, P., 2019. Sedation. In: Intensive Care Nursing New York: Routeledge, pp. 59-68.
- XYRICHIS, A. and REAM, E., 2008. Teamwork: a concept analysis. Journal of Advanced Nursing. 61(2), pp. 232-241.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "radiography"
Radiography: specialisation in the use of radiographic, radiation therapy and magnetic resonance equipment to administer radiation treatment and produce images of body structures for the diagnosis and treatment of injury and disease.
Related Articles