Name of examination:
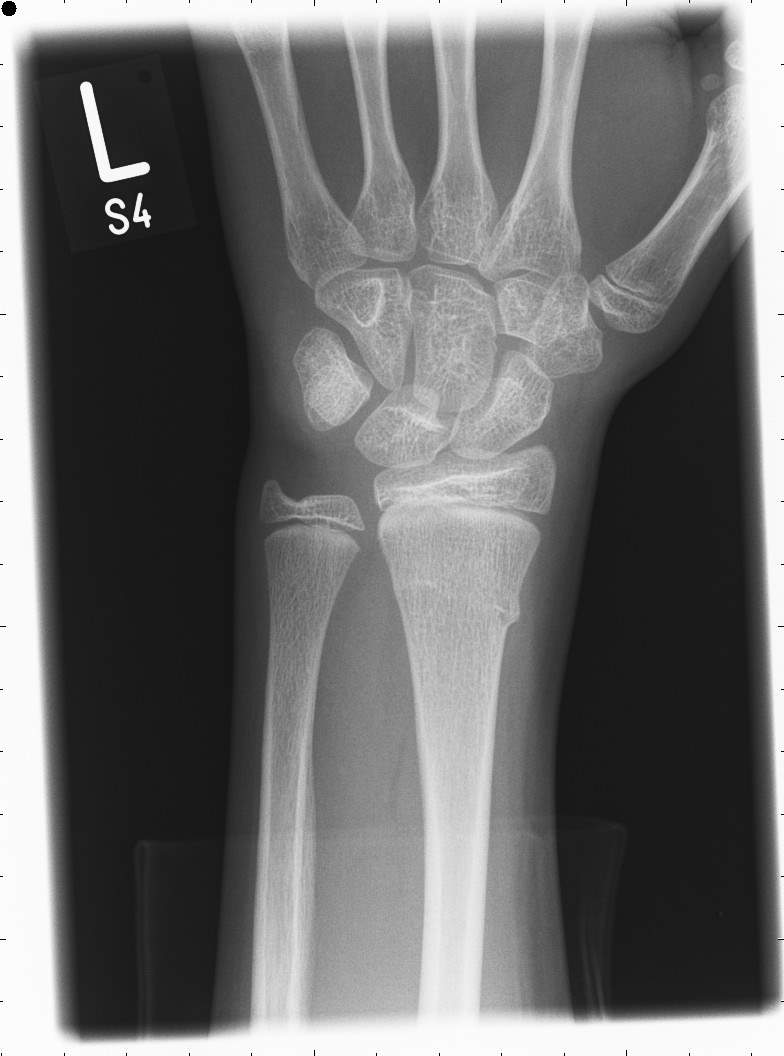
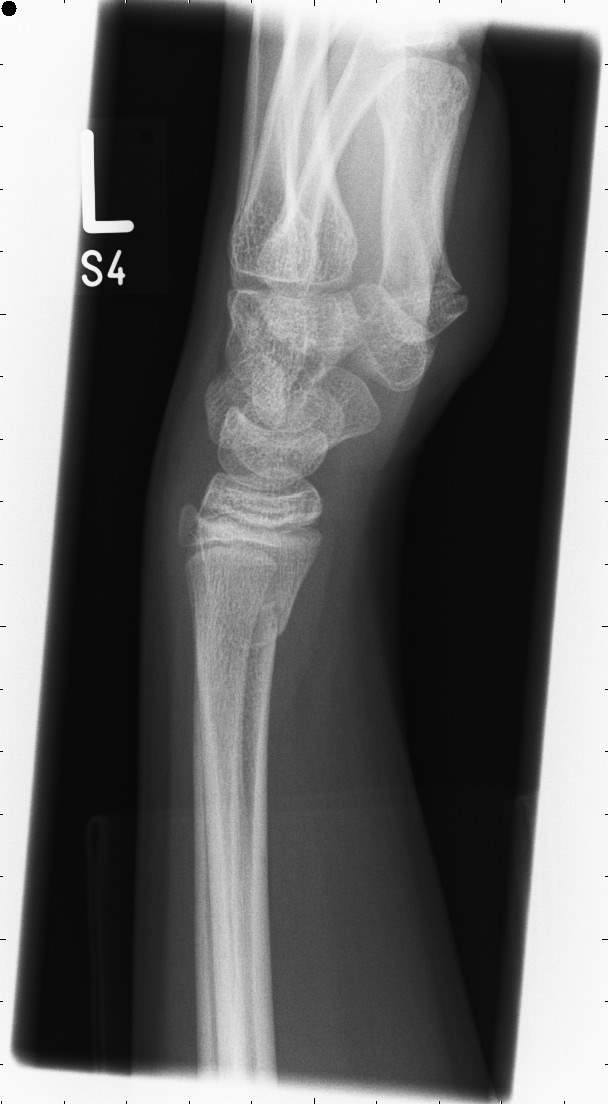
Posterior-anterior (PA) and lateral radiographic images of the left wrist.
Clinical history:
The 18-year-old service user attended the Accident and Emergency department (A&E) with her mother. She had been seen by a registered nurse and a general medicine doctor. The left wrist X-ray request stated, “fall on to the outstretched hand, FOOSH, limited movement of the wrist and distal forearm”.
To justify the X-ray examination,” a request must be sent by registered healthcare staff who is a member of a profession regulated by the National Health Service Reform and Health Care Professions Act 2002”. (Sor.org,2017, schedule,1)
FOOSH is the medical acronym for “fall on to outstretched hand” (Herring, 2016). The request justified as the request was sent by general medicine doctor and there was a slight swelling over the left wrist (Legislation.gov.uk, 2017). In addition, FOOSH is the common injury between all ages and it is the second cause of distal radius fracture.
Patient’s previous radiographic images have been checked to prevent unnecessary repeat X-rays and keep the radiation dose as low as reasonably practicable. According to the World Health Organisation, ionisation radiation is harmful to the various organs of the body and IR(ME)R regulation state clearly that patient’s history and previous radiographic images should be checked to support procedure. (Sor.org,2017, schedule,1)
Patient care issues:
For the purpose of this case study, I named the service user Rose White.
Rose fell on to outstretched hand while she was playing games with other classmates in school. Following the accident in school, she came to A&E with her mother. Rose prioritised as an urgent request because distal radius fractures are the most common fractures in the UK with a reported incidence rate of 190–200 per 100,000 person-years and is associated with signs of bruising or swelling. (Court-Brown and Caesar, 2006 p.691-697)
Rose’s mother was invited into the X-ray room to reduce the patient’s stress, as the service user was at adolescent age which requires sensitivity and special patient care. (Ehrlich, Coakes and Ehrlich, 2009,0110 p, 109). Moreover, the hospital environment can bring a stressful atmosphere to patients and their families which may affect the patient’s mental state. Therefore, the student radiographer talked to the patient in a very calm manner and decided to face the patient with good eye contact to reduce the stress of the patient and transfer his sense of empathy. (Ehrlich, Coakes and Ehrlich, 2009, p,100).
In all circumstances, except in an emergency, the consent of the patient must be taken for diagnosis which is a legal step in health care or medical care (Rcr.ac.uk, 2019). The student radiographer introduced himself and his supervisor and got the permission from Rose to carry out the X-ray examination.
The Clinical Imaging Board (CIB) considered the importance of identifying the patient correctly and expect all members of the medical imaging sector to check the identity of the patient before performing imaging procedures (Sor.org, 2015, patient identification). Two forms of identification were checked. Pregnancy status didn’t check as the trust protocol states this is only required for a female age 12-55 year of age for examination above the knees and below the diaphragm.
Thereafter, student radiographer listened to Rose accident story to relieve the patient’s stress and clarified clinical history. the student radiographer washed his hand (equipment hygiene maintained before the patient arrived) and wore gloves for infection control (Sor.org, 2019).
According to patient care in radiography 2012: Communication skills have a direct impact on your work environment and the way people respond around you. In addition, your professional attitudes and manner can make effective communication between the patient and the NHS staff. (Ehrlich, Coakes and Ehrlich, 2009, p, 90).
Lastly, the student radiographer gave a brief explanation of the X-ray examination and purpose of that to the patient and built up a friendly verbal and non-verbal communication with the patient and her parent.
Projection:
Radiographic technique:
Many fractures are not clear with one projection for a radiologist or radiographer to report properly, therefore two radiographic views used to provide comprehensive information. PA and lateral projections are usually used for a wrist examination and there are standard projections in the hospital protocol and NHS guild lines (Ouh.nhs.uk, 2012. P.13). The lateral view is used to assess intercarpal ligament, and the posteroanterior (PA) projection apply to direct the wrist joint in a neutral position without any deviation and extension. (Gilula and Yin, 1996)
PA projection:
Before entering the patient, a chair was placed next to the imaging table, so the patient’s affected side would be closer to the surface of the table and source image distance was set (SID) to 100cm. Thereafter, radiographer put the wireless detector on the imaging table. The patient sat on the chair and placed her hand on the detector. palm and anterior aspect of patient’s hand and forearm placed on the detector. An abduction of her wrist achieved, and her elbow was flexed at 90 degrees. It is advisable to raise the table up, so the forearm and shoulder are aligned if the patient mobility permit. Aligned shoulder with forearm wasn’t achieved as Rose had lots of pain and limited movement. (Sloane et al., 2010. P.218)
The X-ray tube was positioned so that the beam would pass through the body to the detector vertically. The beam was collimated to include two-thirds of metacarpal superiorly and to the distal one-third of radius and ulna inferiorly. The centring point was set between the styloid processes of radius and ulna. The correct marker placed on the detector. (Sandström, Ostensen and Pettersson, 2003. P.57)
Lateral projection:
After taking the first radiographic image, student radiographer asked Rose to role her hand as if she wanted to shake a hand. The student radiographer made this simple question to place the lateral aspect of the patient’s ulna and hand on the detector. The student radiographer rotated patient’s hand to achieve the superimposed position of the radial-ulnar styloid process. The student radiographer pressed the memory button and turned the collimator as the previous collimation was the same for a superior and inferior aspect of lateral projection and the centring point achieved over the radial styloid process. Lastly, the correct marker was placed on the detector and SID remained at 100cm.
Exposure factor:
|
|
kVp |
mAs |
Focus Size |
SID |
IR used |
Secondary radiation grid |
|
PA projection |
52 |
2 |
Fine |
100cm |
Digital wireless detector |
None |
|
Lateral projection |
52 |
2 |
Fine |
100cm |
Digital wireless detector |
None |
Table 1: Numerical information about the exposure factor for PA and lateral projection of wrist.
kVp: Stand for Kilovoltage peak which measure the amount of voltage applied to X-ray tube and controls X-ray photon energy. It determines the velocity of electrons between the cathode to the anode. (Holmes, Elkington and Harris, 2014, p.14)
mAs: Stand for Milliampere-seconds which measure the radiation dose over specific set time in the X-ray tube. When other exposure factors are constant, mAs affects radiographic density. (Holmes, Elkington and Harris, 2014, p.15)
Exposure factor and contrast:
The possibility of harmful radiation depends on different parts of the body, therefore the amount of kVp must accommodate with ALARP in relation to radiation dose control. High kVp can decrease the contrast of a radiographic image, whereas low kVp can decrease the sharpness and density which is characterised by being a darker or brighter radiographic image. (Fauber, 2017, p.55)
Image density, sharpness and quantum noise:
The density of a radiographic image can be checked for its brightness. Brightness and density defined in the same way in image quality, but they are different. The amount of light emission in a display monitor is called brightness while the density controls the amount of blackness in the display monitor. For example, if the brightness of an anatomic structure is greatly increased, the density will be decreased. But it should be noted that the digital images and film-screen have a great impact on the image density. The sharpness of the image can be measured by the accuracy of recorded detail and the visibility of the anatomical structure lines. The image resolution or sharpness can be decreased by patient movement. Quantum noise depends on the absorption of the photon through the detector and directly affect the density of a radiographic image. More photon from the X-ray tube reaching the detector cause the fewer quantum noise. (Fauber, 2017, p.52-63)
SID: it is the distance between the X-ray tube and the detector which directly affects the sharpness and intensity. Standard SID introduced for the different part of body to achieve better magnification and sharpness. 100cm is a standard SID for the wrist X-ray examination. (Fauber, 2017, p.89-93)
For the above reasons, the standard exposure factor of 54 kVp and 2 mAs was used. Moreover, the wrist tissue is not much thick, and Rose was in early adolescent age and hasn’t been ossified completely.
Image critique:
Patient identification:
|
Three types of patient identification including patient name, date of birth and address were checked at the patient’s arrival and matched to the specification of the Epic system. The following details were checked on the imaging display monitor as well. These details removed from this case study to maintain confidentiality. The patient’s personal details should not be shared with anyone other than healthcare professionals involved in the patient’s health plan. (Sor.org, 2007) |
Area of interest:
|
the area of the interest for lateral and PA radiographs of the wrist joint should include two-thirds of metacarpal superiorly and to the distal one-third of radius and ulna inferiorly. Skin border should be covered laterally. (Clark, Kreel and Paris, 1979) The area of the interest for the wrist X-ray demonstrated on radiographic images. |
Markers:
|
The correct anatomical side markers were placed at the time of exposure on the lateral aspect of the radiographic image in the primary beam. Radiographers have the responsibility to work on the highest standard to support their profession. The post-processing marker added to the image on the network does not meet full safety. Subsequently, it might have confused radiographer and possess wrong post-processing marker. (Sor.org, 2014) |
Collimation:
|
Both: the radiographic images indicate collimation on four sides; collimated two-thirds of metacarpal superiorly and to the distal two-thirds of radius and ulna inferiorly. AP projection: Radial styloid is located laterally and ulnar styloid is placed medially on the IR. Skin border of the hand in PA projection was achieved adequately. (McQuillen Martensen, 2015 pp.177-194) Lateral projection: ulnar styloid is placed posteriorly to the IR and anterior aspect of scaphoid and radius are aligned. Radius and ulna are superimposed. Skin border of the forearm covered adequately. (McQuillen Martensen, 2015 pp.177-194) |
Exposure factor: Penetration, Contrast and Sharpness
|
The sharpness of both radiographic images is adequate as the difference in their structural lines determine the quality of the radiographic image. patients movement can decrease the radiograph sharpness. (Fauber, 2017, pp.224-227) Viewing the recorded detail refers to the contrast and penetration of a radiographic image. The contrast of the radiographic images is adequate as the distinction between soft tissue, air and bones are easily recognizable and bony trabecular pattern can be seen as the penetration of radiographic images are adequately achieved. (Fauber, 2017, pp.224-227) |
Correct projections and positioning:
PA and lateral projections are used for a left wrist examination. Radiographic images help radiologist to see the joint space, and the anatomical structure is well visible. Using these projections can increase the likelihood of a possible fracture or dislocation diagnosis. (Sandström, Ostensen and Pettersson, 2003. P.57)
|
AP |
lateral |
|
* left (affected) side near to IR * SID was set to 100cm * the elbow was flexed * anterior aspect of forearm and hand pronated. * The centring point was set between the styloid processes of radius and ulna. |
* left (affected) side near to IR * SID was set to 100cm * the elbow was flexed *medial margins of little finger and ulna lie on the IR * the centring point achieved over the radial styloid process |
Artefact:
|
An artefact is an unpleasant substance and structure that is not normally recorded in the radiograph. (McQuillen Martensen, 2015) There are preventable artefacts as the patient’s cloth can be seen on both radiographs, but it has not obstructed any anatomical structure. Moreover, anatomical side markers were placed at the time of exposure as an unavoidable artefact. |
Repeat:
There is no need to repeat the examination as two radiographic images were taken adequately to diagnose the query fracture. No further radiographic image is needed because the fracture in the distal Radial region is quite clear.
Pathology and anatomy:
Distal radius fracture is clearly seen in the radiographic images, which is one of the most common radius fractures, and there is no specific pathology in the radiographic image. Because of the growth plate on the distal aspect of radius and ulna, it can be said that the patient is between the ages of 17 and 19. (Gunn, 2012)
|
trapezium |
trapezoid |
capitate |
hamate |
|
Under the thumb |
Next to the trapezium |
Caps the third metacarpal |
Has a hook on it |
|
Scaphoid |
Lunate |
Triquetral |
Pisiform |
|
Under the anatomical snuff box |
Moon shaped |
Under the pisiform |
The smallest carpal bone |
(Gunn, 2012)
- McQuillen Martensen, K. (2015). Radiographic Image Analysis – E-Book. 4th ed. Saintt Louis: Elsevier – Health Sciences Division, pp.177-194.
- Fauber, T. (2017). Radiographic imaging and exposure. 5th ed. St Louis: Elsevier, pp.224-227.
- Sor.org. (2014). Use of anatomical side markers | Society of Radiographers. [online] Available at: https://www.sor.org/learning/document-library/use-anatomical-side-markers/use-anatomical-side-markers [Accessed 19 Jan. 2019].
- Clark, K., Kreel, L. and Paris, A. (1979). Clark’s Positioning in radiography. 10th ed.. 10th ed. [London]: W. Heinemann Medical Books, pp.55-59.
- Herring, W. (2016). Learning Radiology: Recognizing the Basics. 3rd ed. Elsevier Health Sciences. page 247.
- Sor.org. (2007). Patient Identification, Confidentiality and Consent: Further Guidance | Society of Radiographers. [online] Available at: https://www.sor.org/learning/document-library/patient-identification-confidentiality-and-consent-further-guidance/patient-identification [Accessed 18 Jan. 2019].
- Sor.org. (2017). 1. IR(ME)R Employer’s Procedures – Schedule 1 | Society of Radiographers. [online] Available at: https://www.sor.org/learning/document-library/irmer-2000-and-irme-amendment-regulations-2006/1-irmer-employer-s-procedures-schedule-1 [Accessed 28 Dec. 2018].
- Gunn, C. (2012). Bones and joints. 6th ed. Elsvier, p.46.
- Trauma. (2013). Bone & Joint 360, 2(6), pp.26-28.
- Ehrlich, Ruth Ann, and Dawn M Coakes. Patient Care in Radiography: With an Introduction to Medical Imaging, Elsevier, 2016. ProQuest Ebook Central, https://ebookcentral-proquest-com.uos.idm.oclc.org/lib/ucsl/detail.action?docID=4397639.
- Gilula, L. and Yin, Y. (1996). Imaging of the wrist and hand. Philadelphia: W.B. Saunders.
- Holmes, K., Elkington, M. and Harris, P. (2014). Clark’s Essential Physics in Imaging for Radiographers. Boca Raton, Florida: CRC Press, p.14.
- Martin CJ, Sharp PF, Sutton DG. Measurement of image quality in diagnostic radiology. Appl Radiat Isot. 1999;50(1):21–38
- Fauber, T. (2017). Radiographic imaging and exposure. St Louis: Elsevier, p.55.
- Legislation.gov.uk. (2017). The Ionising Radiation (Medical Exposure) Regulations 2017. [online] Available at: http://www.legislation.gov.uk/uksi/2017/1322/regulation/10/made [Accessed 13 Jan. 2019].
- Court-Brown, C. and Caesar, B. (2006). Epidemiology of adult fractures: A review. Injury, 37(8), pp.691-697.
- Rcr.ac.uk. (2019). [online] Available at: https://www.rcr.ac.uk/sites/default/files/docs/radiology/pdf/BFCR%2812%298_consent.pdf [Accessed 13 Jan. 2019].
- Sor.org. (2017). Health and safety (HS) standard | Society of Radiographers. [online] Available at: https://www.sor.org/learning/document-library/standards-radiographic-practice-post-mortem-cross-sectional-imaging-pmc-si/health-and-safety-hs [Accessed 13 Jan. 2019].
- Ouh.nhs.uk. (2012). Justification of exposure including referral criteria and exposure protocols guidelines. [online] Available at: https://www.ouh.nhs.uk/services/referrals/radiology/documents/justification-guidelines.pdf [Accessed 13 Jan. 2019].
- Sandström, S., Ostensen, H. and Pettersson, H. (2003). The WHO manual of diagnostic imaging. Geneva: Published by the World Health Organization in collaboration with the International Society of Radiology, p.78.
Cite This Work
To export a reference to this article please select a referencing style below:

