Asthma
Function of the respiration system
The upper respiratory is composed of the oral cavity the pharynx, nasal cavity, and the larynx. The upper respiration tracts ensure that the air that entering the lower respiratory track is damp, warm and clean. And lower respiratory tract includes the trachea, the left and right primary bronchial and constituent of both lungs. Their functions are to carrier air from the larynx down towards the lungs (Maghten2013)
What is asthma?
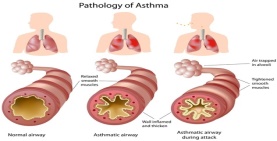
Asthma is a result of persistent inflammation of the air ways most especially the bronchioles and the bronchi. The bronchi increases bronchioles inflammation with the excess of mucus production and swelling which enlarge the mucous glands then result in reducing of the air ways.
Causes a
Asthma is caused by a combination of genetic and environment interaction. This influences both its reaction and its severity to treatments. Factors such as genetic liability to the condition may increase the likeliness of developing the condition. e.g a house hold link in asthma .
| Risk factors | cause factor |
|
|
Sign and symptom
Asthma includes episodes of wheezing, and present symptoms such: as breathless, chest tightness and coughing particularly at night or in the early morning.
Diagnosis:s Diagnosis can be difficult, especially in children and those beneath the age of 5 years, then again the spirometry and the measurement of peak expiratory flow (PEF) are the lung-function equipment most regularly used to measure airflow obstruction in children .
Asthma managementthe goal in management of asthma is to keep control of the lowest possible dose of medication, and the ICS is the first line cure of choice, and this must be initiated in all youngsters with asthma. A very low dose is required depending on the age of the child, such as Clenil 50mcgs 2 put twice a day (very low dose) or Clenil 100mgcs 2 puffs twice a day (low dose) are the recommended dose and these are very safe
References
Bush at el( 2017) severe asthma in children, respiratory, vol 22. Issue, https://doi-org.apollo.worc.ac.uk/10.1111/resp.13038
Kaufman. G(2011) .ASTHMA : pathophysiology , diagnosis and management , nursing standard . 26, 5,48-56 available : wwwworcesterbb.Blackboard.com
Maghtrn.j( 2013) children respiratory nursing 1st edition
Richard and Kerr (2016) Asthma in children, medicine vol (4) issue( 5 )p 281-286, hhts://doi.org.10.1016/j.mpmed.2016.02.014.
Contents
iIntroduction…………………………………………………………………………..…1
Asthma definition……………………………………………………………………..…2
Trigger and factor ………………………………………………………………….……3
Asthma classification……………………………………………………………….…..5
Atopic asthma
Non atopic
. Clinical presentation…………………………………………………………………….5
Sign and symptoms………………………………………………………………….…6
Diagnosis…………………………………………………………………………….…..7
Anatomy and physiology……………………………………………………………….8
Asthma management …………………………………………………………………..9
Inhaler technique
Pharmacotherapy option
Psychology perception therapy intervention
Conclusion……………………………………………………………………………10
Reference …………………………………………………………………………….11
Introduction
Asthma in children and young people remains a significant burden on all area of primary care. In the UK asthma occurs in 1 in 11 children and accounted for 2500 acute hospital admission. Despite advanced in its management, asthma remains a life threatening condition and many children still dying each year (Barrior at el 2006).Therefore the aim of this report is to increase health professionals’ awareness of asthma disease, and enhance their confidence and skill when dealing with children who are presented with this condition. Using different literatures research will allow the report to provide a better understanding of the disease pathophysiology as well as an insight of the underpinning and development of anatomy and physiology of children’s airways affected by the disease. As well provide some management tips and therapeutic strategic that will help manage the condition .Although the choice of this condition results from my own experience, having looked after my own child who was affected by the condition last year.
Asthma definition
The global strategy for asthma management and prevention describe asthma as a chronic inflammatory disorder of the airways in which many cells and cellular element plays a role. Its associated with airway combination of the bronchial obstruction within the lungs that leads to repetitive episodes of wheezing, breathless, chest tightness and coughing particularly at night or in the early morning(Richard and Kerr 2016) .
Literatures
Asthma it refers as a long-lasting disease among children, it’s a condition that linked to higher death, the condition runs in families, especially for those with bad skin (eczema) and other allergies. And study indicates that they may be evidence to indicate that the phenomenon of childhood bronchial, asthma has increased in the past 50 years, and the reason for this stay very doubtful. While a number of life style factors, as well as genetic are involves for its causes (Bacharier at el2011)
In the UK approximate one millions of children have been diagnose with asthma, this can suggest that every classroom has one out of 11 with asthma, and it appeared to be the most common long-lasting disease in children (NICE 2011).Therefore the prevalence of childhood asthma symptoms in the UK is among the highest worldwide and contributes to the estimated of £ 1 billion annual cost of asthma care to the NHS. (Daines and MCmurray 2016). Study also indicates that the condition seem to occur more in boys than girls. Therefore boys aged 5-14 are frequently presented to primary care with 95 consultations for every 1000 registered patients.
This condition impacts on children as well as their love ones, its decreases quality of life in children and their families, with different issue such as school non-attendance, parent work non attendant, sleep hardship and failure to take an interest in exercise. Studies indicate that asthma can limits exercise activities by 39 % and can cause lifestyle change in 70%, study agrued that school non-attendance can also impact on children achievement and therefore limits their future education and career options (Marsh 2017)
Causes of asthma
Asthma is caused by a combination of environment and genetic interaction. These impact on its reaction to treatment as well as it severity. Study argued that genetic risk factor to the disease increases the risk of developing asthma; e.g a family link in asthma has also established the chance of developing the condition by ten times likely (Rees 2010). However, studies suggest that genetic alone does not account for the development of the disease; it also relies upon on surroundings element factor connecting with genetic tendency. Thereforeasthma has been associated with many environment elements that increase the chance of developing the disease. This can includes allergens, air pollution, and different environment chemical such as exposure to smoking as well as smoking in the course of being pregnant or after delivering increase its severity (Holgate and Douglas 2010).
Furthermore some studies also support the hypothesis which suggests that the risk of respiratory infection and asthma were positively related to each other. For example infection of the respiratory tract in infancy led to greater infection in the following years, and asthma symptoms in children similarly led to extra asthma symptoms the following years. The viral of upper respiratory infection have been related with 80%. Therefore asthma and the respiratory infection are the major element of acute and persistent death in childhood because they placed considerably burden on children and family member (Alban at el 2017)
Classification of asthma
Asthma is medically classified according to the frequency of symptoms and sign pressured expiratory volume in one second and peak expiratory flow. Therefore study suggest that asthma can also be classified as atopic or non-atopic , based on whether sign are precipitated with aid of allergens or no (Barrior at el 2006).Although atopic asthma, usually start in childhood then in formative year ,and this is connected along with identifiable obstructions that bother wheezing, coughing. It’s also connected with house hold history on allergic disease, which is characterised by eczema or rhinitis. Asthma disease generally happens as a result of allergy reaction to allergen such as house dust, dirt, grass, domestic pet . e.g in atopic asthma, a family history of allergy are also more likely to develop asthma desease than other children . This increases the production of immunoglobulin (IgE) antibodies as particle after the surface on the mast cells, basophils spherical and the bronchial bloods vessel. Therefore when the allergens is motivated, the antibody responses effect of the release of the histamine mucus secretion then the muscle shrinkage so much slimming the airways (Waugh at el 2010).
2. Non atopic
In the case of asthma not in all situation asthma condition is referred as being caused by environmental factors. Although factors unrelated to atopic diseases are also important to consider. This kind also takes place later in adult life yet where there is no history of infancy allergic reaction. However this is often connected along with chronic inflammation of the upper respiratory tract, such as nasal polyps, chronic bronchitis. As well as additional casual factor which includes exercise, inhaled paint fume, air polluted that in turn can cause an asthmatic reaction in some patients(Mighten 2013). However an attacks also tend to increase when the condition is worsen overtime although in case of lung damage this can become unmanageable and can also cause deficiency in the amount of oxygen reaching the tissue , pulmonary hypertension and right sided heart failure (Waugh and Grant 2010)
Sign and symptom
Asthma symptoms can include shortens of breath, chest tightness and coughing, particularly at night time and early morning. A number of asthma attack usually occur progressively taking 6-48 hours to become very seriously ,but an attack in some patient with asthma can get worse very quickly than other. Although signs of asthma are few and non-specific, relating of air from lungs. Although this might be heard on auscultation and physical examinations because it might also reveal signs of condition, such as bronchiectasis, obesity or in atopic patient, eczema or allergic rhinitis (Adrew at el 2017)
Clinical presentation of asthma
Some of the symptoms of others patient might not to be easily identified from each other. While childhood onset allergic asthma is commonly related with skin inflammation, rhinitis, food allergy, a family history of asthma wheezing, coughing, viral respiratory infection .In childhood asthma, children have regular wheezing then adult the likelihood and regular symptoms increase with early life allergen reaction, and passive smoking (Pride 2018).
Diagnosis of asthma
In children the diagnostic of asthma depends on recognition of the attribute pattern of symptoms that makes the condition more or less likely diagnosis. But it is important to understand that while asthma is common disease, however they are different causes for the sign and symptoms, and it is vital that these diagnosis are not missed. Because a wrong analysis can have profane consequences, which will can lead to unnecessary treatments and anxiety (Brooker and Rachel 2014) .However it can be difficult to give a correct diagnostic result of asthma disease, while diagnosis requires medical analysis and judgment. Because signs and symptoms of asthma can different from one patient to another and can also vary within the same patient at different time. Therefore the diagnosis can be difficult, especially in children and beneath the age of 5 years; however studies suggest that the spirometry and the measurement of peak expiratory flow (PEF) are the lung equipment regularly used to measure airflow obstruction in older children(Mighten 2013).However research suggests that there is no single test that can confirm whether a child has asthma, but parent and health professional can work together over a period of time to ensure any diagnosis made is accurate (Hansen 2015). However to discern between over diagnosis and inactive asthma it is important to keep a record of the basis on which a diagnosis was made, so that, it can be reviewed later (warren 2012)
Anatomy and physiology of asthma.
The main lung’s function is providing oxygen to blood and remove carbon dioxides, to accomplish this, pressure gradient must be created between the terminal respiratory unit and the outside air, by contracting the diaphragm against a thoracic cavity held by the ribcage. Therefore a negative pressure is generated and air passage occurs. However In poorly controlled respiratory condition such as asthma the diaphragm works much harder than normal and can deform the chest wall as the muscle fibres attaches to the lower part of the ribcage, this deformation of chest called harrison’s sulci( Bush at el 2017). Asthma disease can cause inflammation of the airway, and these airways are the small tubes called bronchi, which transport air in and out of the lungs. During asthma the bronchi can be very inflamed and sensitive than normal. And the cartilaginous bronchi, membranous bronchi, gas exchange bronchi consist of the air way of the lungs. Their first function is conducting airways from the nose or mouth down to the level of the terminal bronchioles. This fills with inspired air at the end of every inspiration and they also contribute to the airways resistance. However the cellular which include mast cells are involved of releasing histamine includes: basophils, neutrophils, eosinophil and macrophages these are responsible mediator which is releases in late or early stage of bronchial asthma. And during the stage of bronchial asthma the mucous membrane and muscle layers of the bronchi can become very thick and contracted , therefore the mucous glands become bigger and enlarge, which result in reducing airflow in the lower respiratory tract ,and become inflamed . Although the cells identified in the airway inflammation includes eosinophil, epithelial cells , mast cell , and activated T lymphocyte and macrophage(Muralitharan and peate 2015).The airways blockage can increased resistance to airflow and decreased the exhalation of breath from the lungs. And this will result in pulmonary change mechanism and increase the work of breathing (Waugh and Grant .2010).
Although the cell that line the airways in the lungs produce mucus as part of the body defence mechanism against foreign, such as bacteria and viruses particles. When the mucus are secreted these particles are trapped, and tiny hair like projection in the air ways which is known as cilia ( this sweep the dirty mucus up and out the lung). However most bronchi increase bronchioles inflammation with the excess of mucus production and swelling. Therefore this inflammation brings about change in the lining cells of the airways, and a number of cells that lined the airways will lose their function of their cilia which will result of the ciliate cell lost. However The ciliate cells that facilitate the clearing of secretion are therefore replaced by so called globet cell( Muralitharan and Peate 2015) . But the cells help the secretion of mucus into the airways, and warm environment of mucus for growing bacteria. Therefore this mucus can became infected and discoloured from overgrown bacterial which result in further inflammation of the respiratory tract that respond to it, and therefore narrowed the airway to and from the lung alveoli and blocking the bronchi and bronchioles (Wiley 2015). And the duration of asthma attacks usually varies from minute to hours, but in severe acute attacks the bronchi may be obstructed by mucus plugs, leading to acute respiratory failure, hypoxia and possibly death (Crawford 2011).
person centred care (PCC) approaches in asthma management
BTS guideline for management and diagnosis of asthma, describe PCC as one that recognised partnerships and team work amongst health professional, patient and their family. This approach should take into account patient preference, need, culture and ethnicity. Therefore this approach encompasses 4 area of diagnosis and management of the condition which includes: Communication, Partnerships, Health promotion and physical care.
Communication
When considering asthma management it is important to acknowledge that a correct diagnostic of asthma is not made on a single sign or symptom. History consideration is just as important as clinical feature. Because patient with asthma or serious asthma are exceptional challenging group and request a multidisciplinary approach. The need for different skills approach includes: assessment of pulmonology allergy, gastroenterology, and otolaryngology, is very important to ensure a complete assessments and diagnosis, are made accurately before management (Ramratnam at el 2017).
Hence the objective of asthma administration in children is to attain asthma control by optimising lung function, which in turn can make differences in decreasing day and night symptoms, lessening restriction in day activities and decrease it severity (Mighten 2013). Study indicates that the corticosteroid (ICS) is the first line treatment of choice and this should be integrated in all children with asthma. A very low dose or low dose is allowed depending on the age of the child. The range of drugs authorize for use in children is limited and Clenil 50mcgs 2 put twice a day (very low dose) or Clenil 10 Omgcs 2 puffs twice a day (low dose) is the usual staring point, and the recommended doses is very safe. However not exceeding 400mcgs per day in children under five and 800mcgs per day (medium dose) in 5-12 years old, beyond this specialist referral is required (Francesco 2014)
Health promotion and physical care
- Inhaler technique
Education of inhaler technique and repeated assessment tend to improve the correct usage, and this should be part of everyday asthma review. Effective inhaler technique is very important in managing asthma , and it needs some time for patient/ parents to develop the skill for correct usage. Almost all children with asthma condition use pressurised metered dose Inhaler (Pmdi) with a spacer, but very young children will need a spacer with a facemask , but one they can tidal breath reproducibly through a mouthpiece, indeed a spacer without mask is preferred as soon as possible drug deposition in the airways will improved. In formative years alternatives to an MDI and spacer, e.g dry power devices can be considered to improve adherence and new inhaler should only be prescribed after the a child has received training in the use of the device, has also demonstrated a satisfactory technique (Harron at el 2017).Therefore physician and nurse should recognise the need to improve these behaviour aspects in patients and seeking partnership with parents/ children and setting individual action plan ,that may be helpful in improving asthma control (Wim and Aaldern 2012). Research study reveals that about 75% of funding was spent treating poorly managed in children with asthma, therefore it is vital that health professional encourage parents to use peak flow meters to better manage asthma and control cost. To achieve this healthcare provide should also control appropriate medication, address environment risk factor, assist with self-management. This can followed by some education provision regarding inhalers technique, compliance, asthma action plan, self-monitoring and follow up appointments (Kaplan at el 2018).
- Pharmacotherapy option
The British Thoracic Society (BTS) based on a global plan of action for managing asthma, outlined pharmacotherapy control medication, this provides immediate relieve of bronchospasm, open airways. Minimal, and ideally no symptoms during night or day therefore no asthma episodes. this includes minimal use of a relieve medication short acting β2-agonist such as salbutamol .other includes normal activities, and function of the lung.(PEFR forced expiration volume in 1 second. and this treatment should be start a suitable level of severity for the individual patient. when staring the inhaled treatment a suitable device should be prescribed after pressured meter dose inhaler(Chavasse and kerr 2016)
Partnership
The resilience model should also be initiated in managing asthma , this model is a frame work for families dealing with chronic health .The model explains, how stress could affect care givers as they adapt to crisis. This state of unbalance can negatively impact on the care of patient with asthma. studies indicate those caregivers who are educated on how to manage their child asthma tend to have an increase perception of control, and this improves outcomes of patient (Paymond at el 2018).Therefore implementing peak flow meters and action plan improve knowledge of asthma and promote prevention, this approaches improves perception of control of child’s asthma and increase confidence in managing the condition
Conclusion
Asthma remains a burden on families as well as primary health care, and asthma management and prevention required national attention and determination if reducing the chance of developing asthma disease is to be improved. Therefore it is important to consider how to make correct diagnosis of the condition base on history and clinical presentation, as these procedures precedes management .Therefore effort should be made to prevent wrong diagnose .however a structured clinical assessment and family history provide a solid foundation for accuracy in diagnosis, and the ICS remains the cornerstone of asthma management and most children with asthma respond very well to very low or low dose and inhaler. While the technique is a key in paediatric asthma management while time must be taken into account at every medical review to correctly check that a child use their inhaler correctly.
Reference
- Adrew at el( 2017) severe asthma in children . https://doi.apollo.worc.ac.uk/10.111/resp.13085
- Alban at el 2017) Longitudedinal associateds between respiratory infection and asthma in young children. Doi 10.1093/aje/kwy053
- Bush at el (2017) severe asthma in children, respirology , vol 22. Issue ,https://doi-org.apollo.worc.ac.uk/10.1111/resp.13038.
- Barrio 2006 .pathology and pathophysiology , archives of pathology and laboratoire Medicine , northfiel vol 130 , issu 4 pp 447-51
- (Brooker and Rachel 2014) asthma in children : diagnostic and management dilemma , practice nurse .11/14/2014,44911):13-1896p)
- Crawford .D (2011) nursing children and young people, Understanding childhood asthma and the development of the respiratory tract .23,7.25-35 .
- Chavasse .J. AND kerr.M(2016) ASTHMA IN CHILDREN , MEDECINE VOL 44 ISSUE 281-286 ,HTTPS:// DOI.ORG/1016/J.mpmed.2016.02.014
- Daines and mcmurray (2016) asthma in children ,Doi:org.apollo .worc.ac.uk/10.1177/1755738016678013r
- Diep At el (2018) The relationship between caregiver’s subjective social status and asthma symptoms and management for children. Journal of asthma .doi: 10.1080/02770903.2018.1437176.
- Francesco at el 2014. Asthma and respiratory physioly: putting function into perceptive. respirology vol 19, issue 7. HTTPS ://DOI: -org.apollo.worc.ac.uk/10.111/RESP.12355
- Hansen, tonje.E(2015) validation of a questionnaire against clicnicla asseement in the diasis in children. , journal of asthma, issn:0277-0903 , vol 52 ,issue 3 p:262-267, doi:10.3109/02770903.2014.966914
- Harron at el 2017) .Frequency of correct use of children inhaler technique in asthmatic (3-15) in order to improve outcomes. Medicine journal 2017 .vol 9.issue 4 p248-251.4p
- Kaufman. G (2011)( Asthma : pathophysiology , diagnosis and management , nursing standard . 26,5,48-56 AVAILABLE : wwwworcesterbb.Blackboard.com
- Kaplan at el (2018) an update on treatments options for children and adult
- Marsh 2017 . Asthma in children, practice nurse, 09536612 vol 47 , issue 8
- Maghten .J (2013) children respiratory nursing 1st edition
- Muralitharan and peate .(2015) pathophysiology for nurse at a glance. Publisher john wiley and son
- Paymond at el( 2018) Care givers perceptive of asthma control, paediatric nursing . vol 44, issue 1, p 17-35.ID674204,18 p18. http:dx.doi.org/10.6064/2012/674204
- Puit and Lawson(2015) Assessing and management asthma: a global initiative for asthma update nursing standard .2015,42 (5): 46-52
- Pride .J. (2018) Asthma Children diagnosis, medical journal (clinical research edition) vol 288, issue 6432, p1666-1668. Doi: 10.1136/bmj.288.6431.1666
- Ramratnam at el 2017 . Severe asthma in children, jounla of allergy and clinical immunology , in practice , vol 5,issu4 p 889-898.doi:10.1016/j.jaip.2017.04.031
- RIchard and Kerr 2016 . qastham in children , medicine vol 4, issue 5 p 281-286, hhts://doi.org.10.1016/j.mpmed.2016.02.014
- Sebastiano at el (2017). Evaluation of diagnosis therapeutic and educational pathway management of asthma in children. Airway disease. doi:10.1111/pai.12839
- WAREN .L (2012) asthma in children, medicine vol 40, issue 4 p 238-242 : https:// doi.org/10.1016/j.mpmed.2012.02.004.
- Wiley B FUNDAMENTALS OF APPLIED PATHOPHYSIOLOGY : AN ESSENTIAL GUIDE FOR NURSE AND HEALTH PROFESSIONAL STUDENT , 2ND EDITION
- Wim.M, and Alderen .(2012) childhood asthma : diagnosis and treatments , vol 2012, article
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "pathophysiology"
Pathophysiology is a convergence of pathology with physiology, and is the study of the disordered physiological processes that cause, result from, or are otherwise associated with a disease or injury.
Related Articles