|
Assignment Title: Delivery of high quality care ensuring the safety of patients and service users is an expectation of professional practice. What is the role of clinical governance in achieving this expectation within Paramedic practice? |
Word Count: 1436
Word equivalent of diagrams (if used): 50
Introduction
To understand the role of clinical governance in achieving high quality care, this essay aims to provide a discussion of the principles of clinical governance and the legislation underpinning it whilst also proposing a method for improving the quality of care within the ambulance service. Clinical governance was introduced to the National Health Service [NHS] in the late 1990’s due to a variety of reasons, one of those reasons being historical failings (Halligan & Donaldson, 2001). An example of a historical failing is the Bristol Royal Infirmary case. Concerns were raised by the anaesthetist about the quality of paediatric cardiac surgery which led to the death of many young children. This case showed the need for strong clinical leadership in quality improvement who will have a shared corporate belief in the importance of quality (Walshe & Offen, 2001). One of the many definitions of clinical governance explains how health care organisations have a duty to maintain and improve the quality of the care provided.
‘Organisational conscience, and, at its most idealistic, the ‘beating heart’ of care…it encapsulates an organisation’s statutory responsibility for the delivery of safe, high quality patient care and it is the vehicle through which that accountable performance is made explicit and visible’ (Halligan, 2006, p. 7)
The term clinical governance was derived from ‘corporate governance’ and the intention was to protect shareholder’s investments and assets, therefore by doing this, the company would minimise fraudulent behaviour and malpractice (McSherry, Pearce, & Tingle, 2011. p.1). Likewise, healthcare professionals are held accountable for all aspects of patient care and the system requires them to provide high-quality care constantly and to further document this so that goals can be reached. As Figure 1.1 shows below, there is no single factor that led the government to the drive of clinical governance but instead a collection of reasons.
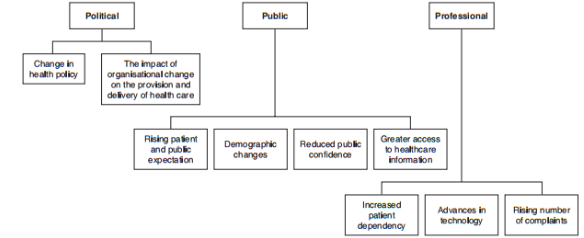
Fig. 1.1: The drivers of clinical governance (McSherry et al., 2011. p. 4).
Discussion
This section provides a discussion of the principles of clinical governance and its role within the ambulance service. It also discusses various legislations underpinning clinical governance and a proposal for improvement within the ambulance service. There are 7 pillars of clinical governance and they are clinical effectiveness, risk management effectiveness, patient experiences, communication effectiveness, resource effectiveness, strategic effectiveness, and learning effectiveness; however, this essay will only further discuss clinical effectiveness and patient experiences with an example within the ambulance service (Nicholls, Cullen, O’Neill, & Halligan, 2000, p. 175).
All healthcare professionals are responsible for clinical effectiveness and it involves using evidence to improve care (DiCenso, Guyatt, & Ciliska, 2005, pp. 37). Clinical effectiveness was defined in 1996 by the NHS Executives as ‘the extent to which specific clinical interventions when deployed in the field for a particular patient or population to do what they are intended to do, that is, maintain and improve health and secure the greatest possible health gain from the available resources’ (Gerrish & Lacey, 2010, p. 495). Clinical effectiveness involves quality improvement strategies such as clinical audits and questionnaires as a means to improve patient safety, experience and outcomes (“Clinical Effectiveness and Outcome” n.d.).
Clinical effectiveness relies heavily on evidence based practice [EBP] to improve clinical practice. The Health and Care Professions Council [HCPC] currently regulate paramedics and include in their standards of proficiency, the importance of EBP in order to continuously improve the quality of service provided and ensuring high standards of care. ‘…be able to engage in evidence-based practice, evaluate practice systematically and participate in audit procedures’ and these standards are expected to be met by every registrant (HCPC, 2014. SOP 12.1, p.11.). EBP was defined below by Sackett, Rosenberg, Gray, Haynes, and Richardson 1996 and it describes how the practice produces accountable professionals which in turn improves clinical effectiveness and ultimately patient experience.
‘Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research.’ (Sackett et al., 1996).
An ongoing clinical trial within the ambulance service is the Paramedic 2 Trial. This trial discusses the pre-hospital use of Adrenalin during cardiac arrests. Adrenalin has been the gold standard treatment for cardiac arrests but there has been insufficient evidence in the form of a placebo- controlled clinical trial that supports it use (Perkins et al., 2016). Since its use in the 1960s, adrenalin has been found to cause return of spontaneous circulation [ROSC], this effect is only short-term and there is a concern that it may cause neurological damage in the long-term. The trial led by Warwick University which started in December 2014 aims to use 8000 participants and will produce results later in 2018 (“The PARAMEDIC 2 trial” 2016).
Overall, this trial will answer a long overdue question about the use of adrenaline during cardiac arrests and therefore will possibly change protocols for the future. This trial also highlights the importance of EBP as the use of adrenaline has not ever been evaluated on this scale until now. As there are about 30,000 out of hospital cardiac arrest cases in the UK every year with approximately 1 in 10 of these patients surviving, this trial could mean a change to the survival rates of cardiac arrests(Perkins & Brace-McDonnell, 2015).
Finally, this trial links to another pillar of clinical governance which is patient experience. The ambulance service does not currently have a direct method of measuring patient experiences unlike hospitals who have various methods such as the Family and Friends Test [FFT] (“Family and Friends Test” n.d.). Patient experience is highly important as they help to highlight areas to improve on within the service. An in-depth report of patient experience by North East Ambulance Service showed that not only does the evaluation of patient experience lead to continuous improvement, it created new opportunities in an environment of growing choice and competition, in addition to that poor patient experiences allowed the chance to tackle any issues early on (Cotton & Hassen, 2011). This was the first ever systematic survey of patient experience done by the ambulance survey hence highlighting the need for more surveys across the whole of the United Kingdom. The present method of public feedback is either through the corresponding websites or through letters and emails (“Feedback” n.d.). Whilst these methods are helpful, they are not official statements, nor can they be used as statistical evidence. With such a large-scale trial such as the Paramedic2 trial, there was a public outcry as although there are ethical exclusions to the trial- pregnant women, people under the age of 16, patients with anaphylaxis or life-threatening asthma- the public are still worried they are not going to receive the best care possible as the trial involves the use of sodium chloride as a placebo instead of Adrenalin (“The PARAMEDIC 2 trial”, 2016).
Therefore, this is an important proposal for improvement for the ambulance service as it provides a better understanding of the concerns that the service users may have. This could be in the form of a survey that can be filled in on every job a crew attends if a patient or their family wishes to do so as according to the Health and Social Care act 2008 ‘As part of their governance, providers must seek and act on feedback from people using the service, those acting on their behalf, staff and other stakeholders, so that they can continually evaluate the service and drive improvement.’ (“Health and Social Care act”, 2017). This could also be extended to staff to ensure maximum effort is being made to improve overall as a service.
Conclusion
The evidence presented in this essay shows that clinical governance is a complex but equally significant topic to discuss. It can be seen as a framework to ensure responsibility and manage quality improvement by reducing inefficiency and malpractice (Savage & Moore, 2004). This essay also discusses the use of several legislations such as the Standards of Proficiency and the Health and Social Care act 2008 to support the pillars of clinical governance. This shows that the law supports the concept of clinical governance. Furthermore, this essay discusses a vital proposal for improvement that involves getting patient feedback in a more ordered and numerical manner. This means that the information received can be collated and used as a means for improving the quality of care as the service users are at the centre of the morals of which the ambulance service holds. Therefore, clinical governance depends upon the integration of clinical and the non-clinical services.
References
- Clinical Effectiveness and Outcome Strategy. (n.d.). Retrieved from University Hospital Southampton: http://www.uhs.nhs.uk/Media/Controlleddocuments/Governanceandsafety/ClinicalEffectivenessOutcomesStrategy2011-15.pdf
- Cotton, M., Hassen, S. (2011). Accident and Emergency Survey of Patient Experience. Retrieved from https://www.neas.nhs.uk/media/30281/accident_and_emergency_survey_-_july_2011.pdf
- DiCenso, A., Guyatt, G., & Ciliska, D. (2005). Evidence-Based Nursing: A Guide to Clinical Practice. Missouri: Mosby Inc.
- Family and Friends Test. (n.d.). Retrieved from https://www.england.nhs.uk/fft/
- Feedback. (n.d.). Retrieved from https://www.scas.nhs.uk/get-involved/how-did-we-do/
- Gerrish, K., Lacey, A. (Eds.). (2010). The Research Process in Nursing. West Sussex: John Wiley & Sons Ltd.
- Halligan, A. (2006). Clinical governance: assuring the sacred duty of trust. Clinical Governance: An International Journal, 11(1), 5-7.
- Halligan, A., Donaldson, L. (2001). Implementing clinical governance: turning vision into reality. The British Medical Journal. Retrieved from https://doi.org/10.1136/bmj.322.7299.1413
- Health and Social Care act 2008. (2017, June 16). Retrieved from the Care Quality Commission website: http://www.cqc.org.uk/guidance-providers/regulations-enforcement/regulation-17-good-governance#legislation-links
- https://doi.org/10.1108/14777270610646967
- McSherry, R., Pearce, P., & Tingle, J (2011). Clinical Governance: A Guide to Implementation for Healthcare Professionals (3rd ed.). West Sussex: John Wiley & Sons Ltd.
- Nicholls, S., Cullen, R., O’Neill, S., & Halligan, A. (2000). Clinical governance: its origins and its foundations. British Journal of Clinical Governance, 5(3), 172-178.
- Paramedic 2: The Adrenalin Trial. (2016, October 13). Retrieved from University of Warwick: https://warwick.ac.uk/fac/med/research/ctu/trials/critical/paramedic2/about/
- Perkins, D., Quinn, T., Deakin, C., Nolan, J., Lall, R., Slowther, A., … Gates, S. (2016). Pre-hospital Assessment of the Role of Adrenaline: Measuring the Effectiveness of Drug administration In Cardiac arrest (PARAMEDIC-2): Trial protocol. Resuscitation Journal, 108. Retrieved from https://doi.org/10.1016/j.resuscitation.2016.08.029
- Perkins, G., Brace-McDonnell, S. (2015, October 1). The UK Out of Hospital Cardiac Arrest Outcome (OHCAO) project. The British Medical Journal, 5(10). Retrieved from http://bmjopen.bmj.com/content/5/10/e008736
- Sackett, D., Rosenberg, W., Gray, J., Haynes, R., Richardson, W. (1996, January 13). Evidence based medicine: what it is and isn’t. The British Medical Journal. Retrieved from https://doi.org/10.1136/bmj.312.7023.71
- Savage, J., & Moore, L. (2004). Interpreting Accountability. Retrieved from Royal College of Nursing website: https://www.rcn.org.uk/professional-development/publications/pub-002249
- Standards of Proficiency- Paramedics, (2014). Retrieved from the HCPC website: http://www.hpc-uk.org/publications/standards/index.asp?id=48
- Walshe, K., Offen, N. (2001). A very public failure: lessons for quality improvement in healthcare organisations from the Bristol Royal Infirmary. British Medical Journal Quality and Improvement, 10(4). Retrieved from http://qualitysafety.bmj.com/content/10/4/250
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "professional practice"
Professional Practice is adhering to policies and procedures regulating bodies put in place such as competency models that professionals practicing in the healthcare sector must meet. In the UK, nurses and midwives must adhere to the policies and procedures set out in the NMC code.
Related Articles


