Group members:
- Zubia Qureshi
- Musa Ali Irfani
- Rawal Insaf
- Shahid Qazi
- Ayesha Sheikh
- Kashif Ali
Contents
2.2- Functions of health care financing
3.1- International comparison of funding system source
3.3- Healthcare financing in 2009
3.4-Healthcare financing in 2010
4- Health care financing of Pakistan
5- What makes the health system complex?
List of Acronyms:
AFR African Region
AMRRegion of the Americas
CERFCentral Emergency Response Fund
DALYs Disability-adjusted life years
EUEuropean Union
EUR European Regions
FATAFederally Administered Tribal Areas
GDPGross Domestic Product
KPKKhyber Pukhtoonkhwa
MDGsMillennium Development Goals
NHSNational health system
OECDOrganization for Economic Cooperation and Development
SEARSouth East Asian regions
OOPOut Of Pocket
USAUnited State of America
WHOWorld Health Organization
WPR Western Pacific Region
Abstract
Pakistan’s health care system is inadequate, inefficient, and expensive. Health is the neglected sector in Pakistan. Pakistan spends only 2% budget for health. It is insufficient for the population. The private sector is playing a vital role in the health care service delivery in Pakistan but majority of services are out of pocket payment. Every country raise its funds for health but Pakistan is in the list of those who decline there health budget.
Donors support Pakistan and other developing countries but unfortunately not properly utilization of funds.
It seems Pakistan government has no interest in improving the health of nation. There is lack of proper planning, implementation, monitoring and evaluation system.
It is strongly recommended that adopt universal health care coverage to reduce OOPS and to make the nation healthy and wealthy.
Health can be promoted and prevented by different ways, which lies either inside or outside the health sector. Health care delivery system and support system such as education, housing, food and employment all impact on health. All these cannot be achieved, without a well-functioning health financing system.[1]
In 2005, Member States of the World Health Organization (WHO) developed the health financing systems to increase the access of services and to reduce the financial hardship paying for them.[2]
Health financing is a key function of the health care system, and is a complex issue. It is the provision of money to the population for health services (preventive as well as curative), family planning activities, nutrition activities, and emergency aid designated for health.[3]
Strong survival of a health system requires efficient financing policy. Without sufficient funding health system can’t work. The six building blocks framed by WHO interrelated and directly related to health care financing. Fair financing is also included in three main objectives of the healthcare system. Remaining two include improving the health status of the community and responding the people’s expectations. The later objectives are directly dependent on healthcare financing.
In the absence of enough financing and resource allocation there won’t be proper service delivery, purchase of medicines, vaccines, lab tests etc as everything is dependent on funds. Increasing community awareness for health care, dependency on technology and diagnosis resulted in increasing need of finances. The rising of costs as the technology advances alarms the health policy makers to devise a sustainable financing approach. As a corollary it seeks to help the planners or policy makers to devise a sustainable approach accordingly. The proper healthcare financing helps to identify the areas which are over or under emphasized.
The health financing is simply an exchange between health consumers (population) and the healthcare service providers.
2-HEALTH CARE FINANCING
The term healthcare financing refers to the ways in which money is raised to fund health activities as well as how it is used (that is, the allocation of funds).[4] The definition signifies three important points i.e.
- Mobilization of funds for health care
- Allocation of funds to the regions and population groups and for specific types of health care
- Mechanisms for paying health care (Hsaio, W and Liu, Y, 2001)
Thus, financing means mobilizing, allocation and accumulation of finances that cover the health needs of the population.
2.2-Functions of health care financing
1-Revenue Collection
Raise sufficient and sustainable revenues in an efficient and equitable manner to provide individuals with both a basic package of essential services and financial protection against unpredictable catastrophic financial losses caused by illness and injury. Level of income, tax-base and fiscal space, tax incidence, transaction cost, the size of the informal sector is major key issues.
2- Pooling
Manage these revenues to equitably and efficiently pool, health risks allowing for subsidies from healthy to unhealthy, rich to poor, and productive workers to dependents. Risk management, how to extend coverage to the informal sector, fragmented pools etc.
3- Purchasing
Assure the purchase of health services is strategic and both allocatively and technically efficient (for whom to buy, what services to buy, from whom to buy, and how to pay) Performance-based payments help to promote quality and efficiency, equity and social protection.
3- International comparison of funding system source
The following are the three broad categories of the health care providers:
- Public Provider
- Private Provider
- Non-Government Organization providers/Non-Profit Institutions
3.1- Mechanism/Methods of healthcare financing
There are various methods of healthcare financing. Most of the healthcare systems operate on mix of the funding methods. These can broadly be discussed under following five headings,
- Taxation (general and earmarked)
- Social insurance
- Private insurance premiums
- Community financing
- Out of pocket payments
Each method has its own peculiarities.
Taxation has been an important source of healthcare funding. It can be general in United Kingdom or earmarked as in France. Earmarked taxes have more advantage over general tax being more specific. It subsequently reduces the resistance to taxation among the public.
Social insurance works as a shared approach. Any agency, most likely governmental, pools the risks and responds them accordingly. This mechanism has its own pros and cons. The Social health insurance is more transparent and eventually more acceptable to the public. It has advantage over private insurance and risk rated insurance. Its disadvantages include reluctance of the employees to contribute to the insurance agency. Moreover, being an individual body, it is more prone to the political interference.
Private insurance premiums do not have major contribution in healthcare financing yet it cannot be ignored. Its focus remains narrow as it covers only a minority of population and that some of the health related conditions do not come in its circle.
Out of pocket spending has been a curse especially in the developing countries like Pakistan. The out of pocket spending in health is inversely proportional to the better healthcare system.
3.2-HEALTH SYSTEM MODELS
National health system model (NHS) Financed through general revenues, covering whole population, care provided through public providers or contracting. The state provides the health care. (Examples: Denmark, Greece, Italy, New Zealand, Portugal, Turkey, and the United Kingdom.)
Social Health Insurance Publicly mandated for specific groups, financed through payroll taxes, semi-autonomous administration; care provided through own, public, or private facilities (e.g., Germany, Japan)
Community Based Health Insurance Not-for-profit prepayment plans for health care, with community control and voluntary membership, care generally provided through NGO or private facilities (e.g., US)
Private Health Insurance Financed through private voluntary contributions to for- and non-profit insurance organizations, care reimbursed in private and public facilities
Contain elements of both traditional sickness insurance and national health coverage. (Examples: Switzerland, and the United States.)
3.3- Universally accepted models
The functioning of health care depends mainly on the level and method of financing. Countries choose between different models. Bismarck’s model The Bismarck’s model was introduced in 1883, Named for the Prussian Chancellor Otto von Bismarck, who invented the welfare state as part of the unification of Germany in the 19th century. It uses an insurance system — the insurers are called “sickness funds” — usually financed jointly by employers and employees through payroll deduction. The Bismarck model is found in Germany, of course, and France, Belgium, the Netherlands, Japan, Switzerland, and, to a degree, in Latin America.
Beveridge’s model Named after William Beveridge, the daring social reformer who designed Britain’s National Health Service. In this system, health care is provided and financed by the government through tax payments. Countries using the Beveridge plan or variations on it include its birthplace, Great Britain, Spain, Cuba, most of Scandinavia and New Zealand. Hong Kong still has its own Beveridge-style health care. Residual model The residual model, called the X model, rejects or seriously limits public responsibility
for allowing citizen access to health care. Health care services are financed
with voluntary individual premiums, thus the private sector has the dominant role.The area of public health is thus separated from individual health care, and the health care sector is regarded as an open field for economic activity. Financing of services is based on private insurance or on individual direct financing. The residual model includes the public sector which covers only persons in special need, including very poor or old people. Siemaszko’s model In the Central and Eastern Europe, the Siemaszko’s model (or the budget model) has been functioning since early 20th century. The principles of its functioning were developed by MikoÅ‚aj Siemaszko (the health care commissar in the Soviet Union in 1930s). It is based on the financing of benefits by the state budget, provides permanent control of the state and equal access to all the benefits for citizens. The choice of a specific financial model entails certain impact on all of the system’s participants.[5]
3.3- Healthcare financing in 2009
In 2009, the world spent a total of US$ 5.97 trillion on health at exchange rates. The geographical distribution of financial resources for health is uneven. OECD countries with less than 20% of the world’s population spend over 80% of the world’s resources on health as compared to 6.5% to the AFR and 3.7% in SEAR regions of WHO respectively. Linking this to epidemiology, the figure shows that though the poorer WHO regions like AFR and SEAR account for the largest share of the global burden of disease (over 50% of global DALYs) and 38% of the world’s population, they spend only 2.5% of global health resources. The WPR without the four OECD Member States, Australia, Japan, New Zealand, and the Republic of Korea, accounts for 24% of the world’s population (dominated by China), about 16% of the global burden of disease but only 4.8% of the world’s health resources. The region of the AMR and EUR, excluding the OECD countries, account for 12.7% of the world’s population, 11% of the global burden of disease and spend only 7% of health resources.
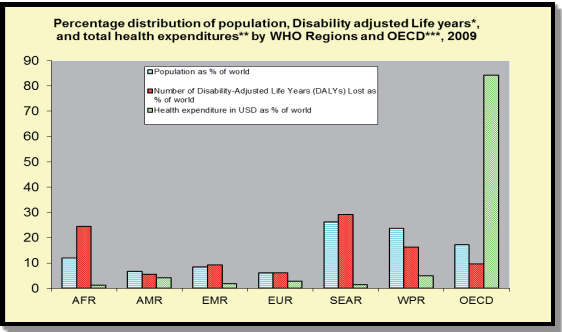
Richer countries with smaller populations and lower disease burden use more health resources than poorer countries with larger populations and higher disease burden. This highlights the absolute need for additional resources for many poor countries and raises questions of efficiency in health spending in richer countries[6].
3.4-Healthcare financing in 2010
Health expenditure as a percentage of GDP in 2010 was 4.5% in the Asian region. This indicator varied from 2% in Myanmar to up to 10.1% in New Zealand. Between 2000 and 2010, the share of GDP allocated to health increased between 0.4-0.7 percentage points in Indonesia, Thailand, the Philippines and China, while it declined by 0.4 percentage points in India. During the same period, Japan and the Republic of Korea reported an increase of 1.8 and 2.5 percentage points respectively. Note that between 2009 and 2010 the share of GDP allocated to health remained stable in the Philippines, Japan and Republic of Korea, while it showed a slight decline for China, India and Thailand, and a slight increase in Indonesia.
This means that the share of health care expenditure in total expenditure continues to increase. Only Brunei, Darussalam and Pakistan showed a slight decline in the annual average growth rate in health spending per capita as compared to an increase in income per capita. In China, health spending has grown at a higher rate than overall economic growth over the past ten years.[7]
4-Health care financing of Pakistan
Pakistan has been facing serious issues in health system regarding accessibility, availability, affordability, efficiency, governance, and accountability. 49 % of Pakistan’s population faces multidimensional poverty with high level of deprivation[8]. Milestone of health in the form of MDGs deadline is approaching near, Pakistan is far away from the achievements of the MDGs.
In Pakistan, The National Finance Commission (NFC) Award is an arrangement through which the federal government transfers funds to provincial governments. The NFC Award has been remaining the cause of disagreement between provinces because of their respective shares. The provinces differ on the criteria set for the Award. Sindh has demanded the share based on revenue collection. Punjab stresses for a population basis while NWFP and Balochistan are insisting on the area and backwardness to be made the basis for the Award. It is assumed that the new NFC Award would be based on a revised Divisible Pool allocation formula. The new formula might be extended beyond the criterion of population to include area or the Human Development Index (HDI).
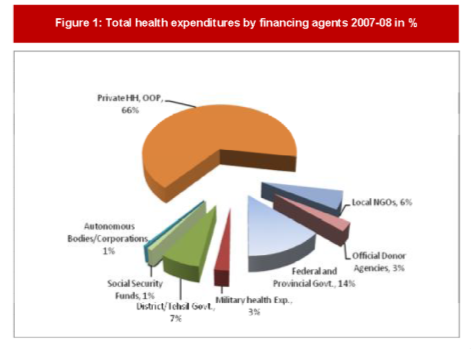
In 2002 Pakistan health expenditure was 3.0 % of GDP than this amount declined to 2.9 % GDP for the years of 2003 and 2004. The health expenditure further declined to 2.8% of GDP in 2005 and 2006, then 3.0 % in 2007 which increased to 3.3% of GDP in 2008[9]. Now only 2% budget is for health. This may be the worst thing a country can do to its citizens other than out rightly murdering them.[10] It is, therefore, not surprising that public expenditure on health in Pakistan is less than that in India, Bangladesh, Sri Lanka, and Nepal[11].
4.2 Funding by donor agencies
The allocation of funds by donor agencies for health in middle and low income countries has gained prominent attention around the world. Billions of dollars are offered for improving health. But these funds are not used in an efficient and effective way that is why we far away from our target in health care.[12]
The Commission has been funding humanitarian aid in Pakistan since the 1990s. In 2012, the Commission was the largest humanitarian donor in Pakistan covering some 35% of the humanitarian funding for 2012. The European Commission’s 2013 humanitarian assistance in Pakistan provided a total of € 52 million. EU humanitarian aid to Pakistan totals almost € 440 million since 2009[13].
The UN system contributes 5% of total health sector investment. The amount to be made available to the health sector is $ 161.6 million, which is more than 26 percent of the United Nation’s financial commitment to Pakistan for this period. Of this allocation, WHO and UNICEF, together provides as much as 78 percent.
Pakistan is the fifth-largest recipient of CERF funding, at a total of $158 million.
4.3-Donation of the year 2013
Humanitarian partners in Pakistan have so far received $191 million since January 2013 for essential humanitarian operations in KP and FATA.
The CERF has provided $13.9 million for the emergency in KP and FATA.
Donors have so far pledged more than $420 million in support of the Fund, bringing the total amount contributed to CERF since March 2006 to more than $3.2 billion.[14]
The UAE Project to Assist Pakistan (UAEPAP) has launched over US$17.1 million for its project to construct seven healthcare projects in Pakistan’s Bajaur, Khyber Pakhtunkhwa province, and South Waziristan. It said that the hospital in Bajaur has been completed while the other six facilities are expected to open before the end of this year.[15]
5-WHAT MAKES THE FINANCIAL SYSTEM COMPLEX
- Population growth
- Relentless burden of diseases,,
- Scarce resources
- Troubles with alternative mechanisms
- Unregulated private sector
- Weak administration
And
Inefficient use of available health budget
6-Challenges:
- Epidemiological transition
- Financial constraints
- Allocatively inefficiency of health sector resources
- Lack of management capacity
- Proper allocation of funds, according to need
- Monitoring and evaluation
- Out of pocket (OOP) expenditure is high which increases poverty and reduces access to quality services
- The budget allocation is geared towards tertiary care and 50% of the expenditure are at the provincial level (mostly tertiary care), as a result the secondary and primary care services suffer from a serious lack of resources
- Establishment of evidence based policy
- Generation of fund resources
7- Recommendations:
Efficiency of service delivery
Some of the recommendations are:
- Raising more funds for health care system
- Improving efficiency and equity
- A combination of financing methods may be adopted as a part of financial strategy, including tax revenue; community financing; social insurance and private insurance.
- OOP payments can be reduced by the standardizing fee structure
- Allocation of donor funds, according to locally determined needs
- Start employes social security schemes
8-Conclusion
Pakistan is spending very low of its budget on health which is not sufficient to fulfill the needs of population. With very low levels of health care financing countries cannot ensure universal access to even a very limited set of health services. On the other hand, higher levels of funding might not translate into better service coverage or improved health outcomes if the resources are not used efficiently or equitably.
The key to a successful healthcare system in Pakistan lies in top management, leadership support and commitment; strong financial methods for improving consumer information, making services or products more affordable through some form of subsidy and creating alternatives for the consumer to access services at a lower cost.[16]
Risk pooling arrangements, proper resource allocation, equity based distribution of services and better decision making power leads towards goal.
——————–THE END————————
1
[1] Closing the gap in a generation – health equity through action on the social determinants of health. Geneva, World Health Organization, 2008 (http://whqlibdoc.who.int/hq/2008/WHO_IER_CSDH_08.1_eng.pdf, accessed 23 June 2010).
[2] Resolution WHA58.33. Sustainable health financing, universal coverage and social health insurance. In: Fifty-eighth World Health Assembly, Geneva, 16–25 May 2005. Geneva, World Health Organization, 2005 (http://apps.who.int/gb/ebwha/pdf_files/WHA58/WHA58_33-en.pdf, accessed 23 June 2010)
[3] Health Organization National Health Account database, World (http://apps.who.int/nha/database/DataExplorerRegime.aspx for the most recent updates).
[4] (CMH, WG 3, 2002)
[5] Pol Merkur Lekarski. 2012 Dec;33(198):309-12
[6] Global􀀃Health􀀃Expenditure􀀃Database􀀃(GHED)
[7]– HEALTH AT A GLANCE: ASIA/PACIFIC 2012 © OECD/WHO 2012
[8] Human Development Report 2012
[9] ;WORLDBANKINCOMEGROUP:–;DATASOURCE:–;RESIDENCEAREATYPE:–;WEALTHQUINTILE:
[10] http://getup.org.pk/issues/HealthcareForAll.html
[11] (World Bank, 2012).
[12] [Health Affairs 26, no. 4 (2007): 950–961; 10.1377/hlthaff.26.4.950]
[13] European Commission Press release, Brussels, 24 June 2013
[14]Report from UN Office for the Coordination of Humanitarian Affairs Published on 19 Aug 2013 WAM ISLAM ABAD, 14th September 2013 (WAM)
[15] Report from Emirates News Agency Published on 14 Sep 2013
[16] Lippincott Williams & Wilkins. JONA Volume 39: Number 6, p.g 263-5 Copyright B 2009 Wolters Kluwer Health
Cite This Work
To export a reference to this article please select a referencing style below:


