While radiography got its start in the 19th century, the profession of radiography in more recent years has emerged into an ever expanding field of high technology. Radiography is a relatively new health profession that has developed expansively over recent years. Advances attributed to computers and the increased use of technology in health care has caused the profession to experience growth that outweighs the recruitment of such professionals. From small beginnings and a lack of formalised training or specialisation the profession of radiography has grown in training, specialisation and responsibility. This profession is at the cutting edge of scientific development, as these professionals continue to work with and specialise in the latest technologies within medical care. Career opportunities for qualified radiographers are abundant now and will continue to be so in the future as demands of the skills for these healthcare professionals escalate and the fields of specialisations and subspecialisations increase. This article reviews the development of the profession of radiography from its history to what it is today, and provides a glimpse into the future of this exciting and indispensable profession.
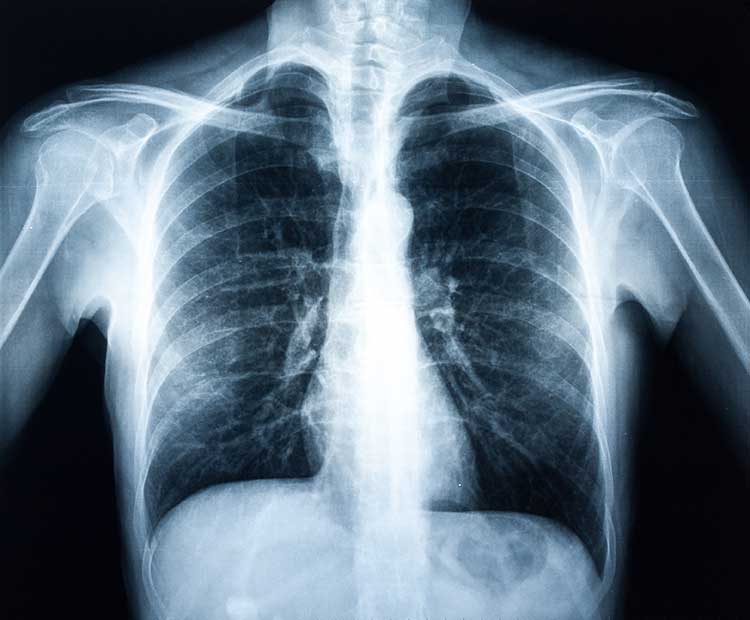
In 1895, Wilhelm Roentgen discovered X-rays. The then unknown rays (hence the X) were soon used in various applications, industrially and medically. X-rays were introduced for diagnostic purposes right from the start. One month after the discovery, Europe and the United States managed to generate several medical radiographs which were then used to guide surgeons in their work. Only 6 months after Roentgen’s announcement of his discovery, X-rays were applied by battlefield physicians to trace bullets in wounded soldiers. It took several years to develop the specialist fields of radiography within medicine based on the discovered technology and as the profession is known today. In over a century since the discovery of X-rays, radiography has metamorphosed from a scientific interest to an important part of medicine. Coinciding with radiography’s metamorphosis was a significant transformation in the responsibilities of the operators of the radiographic equipment. The following is a summary account of the history of the profession of radiography – how it started, how it became a profession, and its developments.
Shortly after Roentgen’s discovery, there were many commercial uses for the X-ray that were devised, some true and some counterfeit, in an attempt to take advantage of the public’s curiosity in the new technology. Professional photographers were some of the first to purchase and implement X-ray equipment because radiography at the time was categorised as a type of photography (1).
By the 1900s, most medical x-ray equipment was owned and operated by businessmen, including engineers, chemists and electricians. Medical practitioners would refer patients to these X-ray operators for diagnosis and treatment purposes. As the needs arose and X-ray treatment and diagnosis became more established towards the 1910s, a number of medical doctors began to purchase their own X-ray machines and some of the doctors were even trained to specialise as radiologists. Although physicians operated the X-ray equipment themselves at the beginning, advances in equipment and technique, quickly exceeded their ability to keep up and they soon recognised that they needed help with the operation of the X-ray equipment so that they could concentrate on treating their patients. Nurses and technicians untrained and ignorant of the hazards of the ionizing radiation they were being exposed to were expected to operate the X-ray equipment (2). They endured significant health problems including loss of limbs and even death. There was no attention given to the lack of training or specialisation of X-ray technicians, until the 1920s and by the 1950s formal education and standardised curriculum were brought into play. X-ray technicians were referred to as “radiologic technologists” for a stronger accent on professionalism. A rapid progression of new technology caused a severe shortage of radiologic technologists in the late 1960s and early 1970s. Techniques such as computed tomography, mammography and sonography that were specialist knowledge were becoming commonplace, and there was great demand for qualified personnel.
In the 1990s due to increasing demands on radiologists alternative ways of delivering radiology services were sought, and the role of radiographers was re-examined (3). This was followed by new roles for radiographers which started to emerge in a wide range of clinical areas in an effort to improve patient care and management.
As the profession of radiography graduated in roles and responsibilities it developed into a medical science that combined technology and caring. Radiographers were soon expected to apply their knowledge to assist in the diagnosis and treatment of patients. Technological advancements have increased the momentum of the modernisation of the radiography profession and with the UK’s professional associations leading the way in research, the development of role advancement continues.
The Profession of Radiography at Present & Future:
Radiographers today play a pivotal role in the NHS as frontline professionals. They are trained and expected by the NHS to provide quality patient care whilst continually developing their own skills and knowledge. Radiography within patient care has evolved dramatically in the last decade and this is extremely important in ensuring the needs of the patient are met. It is true to say that the scope of practice has widened so significantly in last 10 years that radiographers are performing tasks which were once the remit of medical practitioners.
The Department of Health drew up the NHS Plan of 2000 (4) to modernise the NHS in the 21st century by introducing new roles and using health care professionals’ skills to their full potential. The aim was to increase the number of health professionals in the NHS, including radiographers, and retain current staff by developing their professional roles. Thus in turn making the NHS more responsive to patient needs. Many studies over the past few years have found that job satisfaction in the health care sector was very low and lack of motivation of staff was a concern. This positive step refreshed the career path of health care workers and paved the way for role enhancement within the radiography profession. Hardy & Snaith (5) state ‘Extended role working is a natural development and a legitimate expectation of NHS staff’.
The proposal of a 4-tier structure was put forward to utilise the available skills mix and develop existing roles in the department. This incorporated 4 levels of practice – consultant, practitioner, advanced and assistant practitioner levels. The consultant being the most senior grade was designed to be a clinical specialist as well as carry out the managerial role. The advanced practitioner is a highly competent practitioner in a specific field with a high standard of specialist knowledge. The practitioner is state registered and is continually undergoing training until full competence is achieved. The assistant practitioner is not state registered and undertakes tasks with direct supervision from the registered practitioner. The programme initially focused on the breast screening units with advanced practitioners performing tasks previously carried out by the radiologist, e.g. film reading, needle biopsy and interpreting mammograms. The assistant practitioners were trained to carry out the basic duties of the radiographer to effectively use the radiographer’s time, e.g. Mammogram examinations. This ‘career progression framework’ has made it possible for those without conventional qualifications to gain employment in certain sectors and there has been strong interest in assistant practitioner vacancies. So far, the execution of the four tier system has been unsystematic and is not uniform throughout the Health Service. It has been proven time and again that radiographers can be as good as radiologists in some areas and are less expensive, meeting the cost effectiveness plan of the government. It is a system in progress that requires radiologists support if it is to succeed. Concerns from radiologists over the quality of radiographer work have been extinguished with many positive studies. Wivell et al (6) established that radiographers could meet the same standards as radiologists in reading mammograms. That said there is a need for professional responsibility and a monitoring procedure should be in place to cover legal and accountability issues.
Another government policy which has been published which may have opportunities for role development for radiographers is the, National Stroke Strategy 2007 (7). Significant emphasis has been placed on the speed of imaging stroke patients whether it is CT, MRI or Ultrasound. Once a patient is diagnosed with a stroke they will require to be screened within 24 hours before any food or fluids are consumed. This is another area where advanced practitioners may be required.
While many radiographers embrace their role development, some may show some resistance to this 4 tier structure. This can be due to unwillingness to pass over some responsibilities and duties to assistant practitioners in the same way that some radiologists do to radiographers. On the other side of the coin some radiographers are opposed to taking on added responsibilities and back up the ‘just a radiographer’ attitude outlined by Lewis et al (8). This resistance and apathy can be seen as a defence against fear of moving out of their comfort zone but if the patient is to benefit then radiographers need to be challenged and motivated to keep learning.
The government and professional bodies are aware of how important and beneficial a rolling education programme is to both health care professionals and ultimately the patient. Continuing Professional Development (CPD) is a requirement that was introduced by the Health Professions Council (9) to encourage a life-long learning culture in the NHS. CPD is a combination of providing the best care to the patient together with supporting an individuals career goals and learning needs. A patient must be confident in the radiographer’s skills and being aware of new technologies and procedures can only enhance a radiographers’ status. A large proportion of CPD is work based and this means that every day is a learning experience and can be reflected upon. CPD is managed by local employers so each department/hospital may have a different structure in place on how CPD requirements are met. Job satisfaction for many radiographers consists of rewards and acknowledgment for the job they do, acceptable working conditions and opportunities, the latter being very important if the job is to challenge and interest the individual enough to build a career in the profession. CPD gives radiographers every chance now to fulfil their potential.
Traditionally the role of the radiographer has been limited to acquiring images but with advancement in the profession over the last 20 years radiographers are now involved in image interpretation. A system such as ‘red dot’ gives more responsibility to radiographers to highlight abnormalities in images and more recently radiographers are reporting on images instead of radiologists. In Accident & Emergency time is of the essence and a high proportion of patients do not require any treatment after their x-ray examination. In most cases a final clinical report is issued 24 hours after a patient is discharged from the department. Paterson et al (9) put forward the recommendation that a report should be produced at the time of the examination, known as ‘hot reporting’ rather than ‘cold reporting’ which is produced at a later date. Although in a lot of cases a hot report is ready, the patient concerned can wait for a lengthy spell in the waiting area before receiving their results delaying their discharge. NHS trusts are under pressure to cut patient waiting times and must put procedures in place to reduce these delays but without compromising the patient care given.
A pilot project was undertaken by Mid Yorkshire NHS Trust in 2004 which saw reporting radiographers given additional training in the A&E department on musculoskeletal assessment, treatment and discharge and then observed over 4 month period. The radiographers were required to provide advice and answer patient’s questions. The outcome of this project demonstrated that this role expansion was beneficial to both the radiography and A&E departments. Inconsistencies found were mainly on the reporting of paediatrics where additional training would be required on the specialist area. Hot reporting has decreased waiting times and the number of patient recalls. Many factors make this objective achievable including, communication systems (PACS), skills mix and availability of personnel. This is a positive step and pushes the role of a radiographer beyond traditional boundaries.
The above has shown how government led initiatives have brought the radiography profession out of the dark ages and have now made it a career of great potential. Technology has also played its’ part in this. Computers are gradually becoming a part of radiographic inspection even if the basis of the methods and techniques of radiography that were developed over a century ago remain in use. More and more radiography is performed without the use of film and this will continue. Computer-Aided Diagnosis (CAD) is now a significant research subject in the medical imaging field. CAD is part of the clinical routine procedure for detection of breast cancer on mammograms. It is currently being used in a few areas including – Thoracic CT, to detect lung nodules on Lateral and PA chest radiographs, in detection of intracranial aneurysms in MRA and in whole body scans. This programme has the aim to help the radiologist detect various diseases and pathologies. As the radiologist is working in an environment with tight deadlines CAD works as an informative tool together with the radiologist and helps highlight areas to help with diagnosis. The CAD programme is still in its infancy and through advancement will some day be integrated into PACS and in turn be used on a daily basis in differential diagnosis.
Digital Radiography (DR) is becoming the standard technology in most imaging departments as its technology evolves. It allows radiographers to capture images in digitised form and use the image in a number of ways eg.the image can be printed, emailed to physicians or other hospitals and also stored in the archives. DR provides high quality images and options to reduce the dose to the patient. The development of mobile DR machines is significant paving the way for DR to play a more superior role than Computed Radiography in the future.
Educational techniques and materials are due to be updated to accommodate technology. Computer aided design (CAD) will be used to simulate radiographic images and used to point and pick the relevant areas or cross-sections to inspect, to fine-tune the placement and orientation of the relevant area to acquire the proper part relationships, and adjust settings to achieve desired film exposure for the development or post processing of radiographic images. Computer simulation will allow students to work with and visualise real-time or almost real-time data and images and may become the primary educational tool for in the technical classroom.
Radiographers may in the future be required to be expert with the application and use of computer hardware and software in imaging. Fields of specialisation will also expand with the increased use of technology. Tomorrow’s professionals will be required to better understand the clinical context of examinations and procedures, interact more directly with patients, conduct imaging research and be truly expert in a sub-specialised field.
Conclusion
In conclusion, the discovery of radiography has impacted the medical profession in a significant way. Pioneer radiography technicians operated equipment with little education or training and sometimes at a cost to their health and life. From small beginnings of a role that was merely described as “machine operator” radiography has grown in leaps and bounds to the cutting edge profession it is today. Radiographers today are more than just ‘button pushers’ – they have a definite career path and are encouraged to continually educate themselves in all areas of their profession and have greater autonomy in their jobs. Radiographers can specialize in certain technologies or procedures; they are recognized as being multi-professional due to the boundaries being blurred with other professions. The role has expanded and duties previously carried out by medical practitioners and radiologists are now a radiographer’s responsibility. This has in turn has improved job satisfaction and helped retain staff in this field. Research and technology in this profession is constantly giving radiographers better tools and knowledge to work with and aspirations can be met. This article has successfully reviewed the revolution within this profession. The future of radiography remains prominent and will undergo further changes, the most obvious being the computerisation of processes and analysis and this is something to look forward to.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "radiography"
Radiography: specialisation in the use of radiographic, radiation therapy and magnetic resonance equipment to administer radiation treatment and produce images of body structures for the diagnosis and treatment of injury and disease.
Related Articles