Introduction
This essay focuses on a reflection on the development from novice, to competent beginner, to skilled practitioner in the light of my own development in clinical nursing practice. It is based on the signposts identified within my clinical learning portfolio and focuses on the notion of the helping role and caring skills within nursing practice. It utilises a reflective framework to better identify and reflect upon the journey from novice to practitioner.
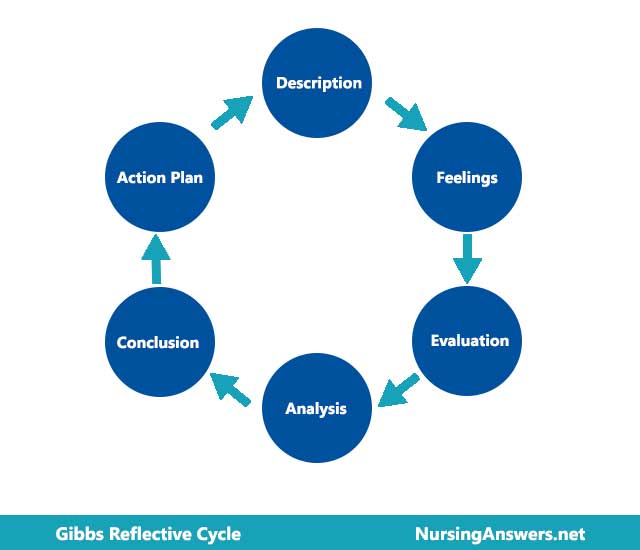
The model for reflection I have chosen is Gibbs Reflective Cycle (see Appendix). Reflection has been described as as a process of internally examining and exploring an issue of concern, triggered by an experience which creates and clarifies meaning in terms of self, and which results in a changed conceptual perspective (Boyd and Fales, 1983). Therefore, the experiences of my three placements are explored under three rotations of Gibbs Cycle. Meretoja et al (2004) state that nurses’ self-recognition of own level of competence is essential in maintaining high standards of care. I have chosen the caring role based on my own recognition of the level of competence achieved in this area.
Cycle One
Novice to Advanced beginner
What Happened.
I had to assist a patient in with personal care; make them comfortable in bed and collaborate in pressure area management; assist with toileting, washing, mouthcare, and application of emollient cream. I also had to document care and any deviations from the norm.
Feelings
I was very aware of my inexperience and of the trust this patient placed in my and the nursing team. I was also aware of the intimate nature of the care I was providing, and the fact that it was basic care also highlighted the fundamental role such care has in supporting health promotion and patient wellbeing.
Evaluation
I was uncomfortable at first, and clumsy in the provision of the various aspects of care. However, my mentor was informative, supportive and helpful, which assisted me in doing the various tasks. However, I found it difficult to complete these as quickly as I should have. I did learn to communicate with the patient and provide a sensitive approach.
Analysis
This situation required fundamental aspects of the caring role. It also demonstrates the link between basic nursing care an every other aspect of nursing. The NMC (2004) requires nurses to provide individualised care for their patients. The care for this person was based on their own needs and adapted as those needs changed. I was able to identify those needs and develop competency in providing care at this level. The caring role was very rewarding but physically and emotionally taxing However, I was still in the process of identifying particular needs and responding to them, such as toileting, which required me working with others in a collaborative manner, which I did not find easy. I also realised how much I did not know about nursing.
Conclusion
In this situation, I could have developed more collaborative working skills and modelled myself on those around me more actively ie., copied the ways in which other nurses and healthcare assistants provided care. When I did do this, it was effective. But I found that despite my enthusiastic approach, my knowledge base meant that I did not always understand the rationale for what I was doing.
Action Plan
The action plan from this was to take the confidence and competence I had developed in the practical skills and incorporate them into all aspects of the caring role. It was also to identify areas where my knowledge base was lacking, and seek out this knowledge. Keeping knowledge up to date is a requirement of the NMC code of condut (NMC, 2004). Working collaboratively is another NMC requirement (NMC, 2004). Taking this knowledge forward into practice made this process of reflection a learning activity.
Cycle Two
Advanced Beginner
What Happened
As part of my role assisting with patient care, I had to monitor pain levels and assist with providing analgesia as prescribed, along with monitoring its effectiveness. This was a surgical placement, and I also discussed with elderly patient their coping and wellbeing after hospital discharge. I engaged in health education and support to enable clients to be self-caring.
I was also responsible for monitoring wellbeing through performing and recording clinical observations, recording fluid balance and reporting any abnormalities. I was also involved in providing personal care to patients in a safe manner, especially in the disposal of waste products.
Feelings
To begin with, I felt glad to be working at a more advanced level of competency, and felt confident in my basic nursing skills including performing clinical observations. However, the increased demand also meant increased pressure and I was aware of this. Again, I felt that I had developed a degree of competency but was very aware of my need to develop further knowledge and skills. The caring role involved supporting people and I had to access other professionals to ensure I gave the right information and that my care had been effective.
Evaluation
It was good to find that I had the clinical competence to effectively monitor clinical status. However, the complex nature of patient needs meant that I still didn’t always know the answers to their questions. Being involved in discharge planning was an enabling activity for myself and the patients. I developed competence in the administration of medications, under supervision, including controlled drugs, but felt I still needed more practice and skill in this area. Colleagues noted my competence and qualified staff were happy to delegate a range of appropriate tasks to me.
Analysis
It would appear that the caring role means the provision of patient centred, holistic care. This was achievable in this situation but required a lot of knowledge and the ability to provide focused attention and empathic care whilst carrying out complex clinical nursing tasks. This was harder to achieve, and I was made aware of my continued learning needs around medication and surgical care, for example. However, I must have developed some competence as qualified staff were happy to delegate to me and to act on my feedback.
Conclusion
It is hard to see what else I could have done, except perhaps done more reading around surgical care, discharge planning and the nurse-patient relationship.
Action Plan
It was possible to identify future learning needs, and so my action plan included building on my current competence by engaging in more advanced practice, under supervision. Having the confidence to engage in more complex nursing tasks will help me to achieve more competence in advanced practice in the future. Recognising the demands of the caring role means that I will view future practice as based upon this role.
Cycle Three
Competent Level
What Happened.
I monitored patients with chronic pain and helped with analgesia. I also supported patients with freedom of choice for their own care (NMC, 2004) and provided personal and palliative care in sensitive manner. I mastered more advanced practical nursing skills including aseptic technique and safe disposal of sharps. I fully documented all care given, and recorded medication given, and communicated to staff at shift change during the nursing handover.
Feelings
During this experience, I felt that my knowledge and experience in the caring role was finally coming together. I was confident and happy in engaging with patients and providing empathy and a supportive manner, whilst also carrying out more complex clinical tasks appropriately and effectively. It was very nerve-wracking giving handover, but I became more confident as I had more practice.
Evaluation
I was able to provide care of a high standard, and recognise my sphere of competence and seek help when needed. I was able to engage in effective caring relationships with clients, meet their individual needs, but also value my own input into their wellbeing.
Analysis
It was obvious that I had moved on to a level of nursing competence which allowed me some autonomy. I was able to act with less direct supervision, but still access the support of the whole care team. The caring role extended to the provision of all care, including end of life care, and I was able to utilise my knowledge and experience and also identify my learning in action, and my future learning needs, which have changed since the first reflection.
Conclusion
The change from novice to competent practitioner in the caring role has demonstrated not only the acquisition of skill but the incorporation of clinical abilities into what is really a way of being with patients.
Action Plan
Signposting future learning needs is important following this reflection. I was able to identify the need to still learn advanced clinical skills and perhaps know more about the range of other professionals who could enhance care in individual situations.
Conclusion
This reflection has signposted my development towards competent nursing practice. The caring role encompasses provision of basic care, advanced techniques, medication and pain relief, health promotion, end of life care and collaborative care. It seems to be the fundamental and most important part of nursing practice.
Collaboration and coordination, as well as the holistic management of the situation, are highly recognized as meaningful characteristics of competent nursing practice (Meretoja et al, 2002).
References
Boyd E, Fales A. (1983) Reflecting learning: key to learning from experience. Humanist Psychol 23 (2) 99–117.
Gibbs, G. (1988) Learning by Doing. A Guide to Teaching and Learning Methods Further Education Unit, Oxford Polytechnic, Oxford
Meretoja, R., Leino-Kilpi, H. & Kair, A. (2004) Comparison of nurse competence in different hospital work environments Journal of NursingManagement.12(5) 329–336
Meretoja, R., Eriksson, E. & Leino-Kilpi, H. (2002) Indicators for competent nursing practice Journal of Nursing Management 10(2) 95-102
Nursing and Midwifery Council (2004) Code of Conduct Available from www.nmc-uk.org Accessed 30-4-07.
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "gibbs reflective cycle"
Gibbs' Reflective Cycle was developed by Graham Gibbs in 1988 to give structure to learning from experiences. It offers a framework for examining experiences, and given its cyclic nature lends itself particularly well to repeated experiences, allowing you to learn and plan from things that either went well or didn’t go well. It covers 6 stages.
Related Articles