Frequency of co-existence of dengue fever and malaria in thrombocytopenic patients presented with acute febrile illness
- Dr. Shazia Yasir (PG Emergency Medicine)*, Dr. Owais , Dr. Faisal Moin
ABSTRACT
Introduction: Both dengue fever and malaria can present with thrombocytopenia. Thrombocytopenia is a consistent finding in dengue fever and is regarded as a strong predictor of dengue fever. Thrombocytopenia is also considered criterion of disease severity, bad prognostic factor and its presence is associated with increase probability of malaria
Objectives: To determine frequency of co-existence of dengue fever and malaria in thrombocytopenic patients presented with acute febrile illness in tertiary care hospital
Study Design: Cross-sectional, observational study.
Place and Duration of Study: Department of Emergency Medicine, Ziauddin University Hospital, Karachi from Ten months from April 2013 to January 2014.
Methodology: A total of 159 patients meeting inclusion criteria were included in this study. 5ml of blood by venupuncture in EDTA anti-coagulant for platelet count and preparing thick and thin films and 2 ml of blood in plain bottle for detection of dengue specific IgM was collected from all patients. Thick films are used to identify malarial parasites and thin films to identify specie. Dengue fever was diagnosed on positive dengue IgM. Co-existence was labeled as positive if malarial parasites and dengue IgM found to be present at the same time. This diffusion susceptibility test was use to determine susceptibility of bacterial agents to antibiotics. Data was analyzed by descriptive statistics using SPSS software version 19.
Result: Overall mean (±SD) age was 38.3 (±7.9) years, with Male to female ratio was 1.1: 1. Co-infections (Dengue and Malaria) were diagnosed in 5 (5.6%) of cases. From 5 cases, 3 (60%) were male and 2 (40%) were female. Mean (±SD) age of 5 positive cases of co-infection was 37.8 (±8.3) years.
Conclusion: Concurrent infections were found 5.6% in this study. Although this percentage is slightly low; special attention should be given to the possibility of co-infection with malaria and dengue.
Key words: Dengue fever, Malaria, Immunoglobulin-M (IgM), febrile illness, Thrombocytopenia _____________________________________________________________________________________________
INTRODUCTION
Dengue Virus is becoming an increasing health problem. Over 99% cases of viral hemorrhagic fever reported worldwide are due to dengue hemorrhagic fever (DHF). [1] Dengue fever is cause by dengue viruses (DENVs) which are members of Flaviviridae family. [2] It has been estimated that 2.5 billion people live in areas which are at risk of epidemic transmission and over 50 million of DENV infections occur globally each year [3,4]. Since we are living in region where malaria is endemic and is considered as the most common cause of fever and in general practice empirical anti-malarial therapy is common, it is important to distinguish the two conditions due to clinical similarities and unexpected progress of dengue fever (DF) to DHF and dengue shock syndrome (DSS). [5]
———————————————————————-
Department of Emergency Medicine, Ziauddin University Hospital, North Campus, Karachi
* Correspondence Email: drshazia24@live.com
Both dengue fever and malaria can present with thrombocytopenia. Thrombocytopenia is a consistent finding in dengue fever and is regarded as a strong predictor of dengue fever. [6] Thrombocytopenia is also considered criterion of disease severity, bad prognostic factor and its presence is associated with increase probability of malaria [7, 8]
In a local study Ali et.al showed that Out of 11 patients diagnosed as having dengue fever on serology 9 (81.8%) also had co-existence of malaria and thrombocytopenia was present in 90% of such patients. [5] Out of 11 DENV positive patients three patients died and first DENV positive patients who died was prescribed anti-malarial by general practitioner in outdoor. [5] On autopsy plasmodium falciparum rings were found in blood and DENV IgM was detected in serum samples [5]
Due to clinical similarities in two conditions and possibility of extensive mosquito exposure, high co-existence of both conditions cannot be excluded. [5] This study aims to determine frequency of co-existing dengue fever and malaria in thrombocytopenic patients presenting with acute febrile illness so that magnitude of the condition could be assessed. The findings could be used to plan that all patients with acute febrile illness with thrombocytopenia must be screened for dengue fever without delay.
METHODOLOGY
This study was carried out at the department of emergency medicine, Ziauddin University Hospital, Karachi, Pakistan. Patients of either gender with more than 12 years of age presenting to Ziauddin Hospital Karachi with acute febrile illness and found to have thrombocytopenia were included in the study while patients known to have disease causing thrombocytopenia e.g. systemic lupus erythematous, idiopathic thrombocytopenic purpura and patients with other causes of acute febrile illness such as pneumonia, meningitis, enteric fever etc. diagnosed on blood culture, chest X-ray sputum C/S, urine D/R were excluded from the study.
A total of 159 patient’s fulfilling inclusion criteria were included in the study. 5ml of blood by venupuncture in EDTA anti-coagulant for platelet count and preparing thick and thin films and 2 ml of blood in plain bottle for detection of dengue specific IgM was collected from all patients. Thick films are used to identify malarial parasites and thin films to identify specie. Dengue fever was diagnosed on positive dengue IgM. To minimize bias all specimen was sent to single central laboratory of the hospital. A proforma especially designed for the study was used to documents findings such as paients age, gender, name, malaria parasite, dengue IgM by the researcher. Co-existence was labeled as positive if malarial parasites and dengue IgM found to be present at the same time.
Data was entered in computer and analyzed by SPSS version 19.0 frequency and percentages were calculated for categorical variables such as gender, co-existing dengue fever and malaria. Mean standard deviation was calculated for numerical variables like age. Stratification was done in terms of age and gender to see the effect of that on outcome.
RESULT
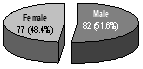
During the study, a total of 159 cases with thrombocytopenia of age > 12 years were included. From 159 cases, 82 (51.6%) were male and 77 (48.4%) were female. (Figure-1)
Mean (±SD) age of 159 cases was 38.3 (±7.9) years with range = 15 – 53 years. Majority 66 (41.5%) of cases had age between 30 – 44 years. (Figure-2)

Out of 159 thrombocytopenic cases presented with acute febrile illness, malaria was diagnosed in 55 (34.6%) cases. (Figure-3)

Dengue fever was diagnosed on positive dengue IgM. Out of 159 cases, 34 (21.4%) of cases were diagnosed as dengue. (Figure-4)

Co-infections (Dengue and Malaria) were diagnosed in 5 (5.6%) cases. (Figure-5)

Out of 5 positive cases of co-infection, 3 (60%) were male and 2 (40%) were female. Mean (±SD) age of 5 positive cases of co-infection was 37.8 (±8.3) years with range = 15 – 52 years. Majority 3 (60%) of cases had age between 30 – 44 years. (Figure-6)

DISCUSSION
Despite a wide overlap between malaria and dengue endemic areas, published reports of co-infections are scarce in the literature. Malaria and dengue must be suspected in febrile patients living in or returning from areas endemic for these infections.
The confirmation of malaria is rapid, and after malaria is confirmed, dengue is usually ruled out without screening for it. Two methods can confirm dengue: dengue-specific IgM sero-conversion or detection of dengue virus particles during the acute phase (day 0 to day 4 after onset of fever) by RT-PCR, which is faster and more specific. In published case reports, [9 – 12] the diagnosis of dengue infection is usually made based on positive dengue IgM; however, this cannot confirm recent dengue, because IgM can persist for months and cross-react with other arboviruses. [13] If RT-PCR requires a specific laboratory and cannot be performed on site, a new test, the Platelia, is now easily included in any laboratory and is indicated particularly for early-acute phase samples. [14] To investigate the frequency of dengue and malaria co-infection, the Platelia test should be used in all cases of dengue-like or malaria-like syndrome, even when malaria diagnosis was positive, in regions where both infections may overlap.
Both dengue fever and malaria can present with thrombocytopenia. Thrombocytopenia is a consistent finding in dengue fever and is regarded as a strong predictor of dengue fever. [6] Thrombocytopenia is also considered criterion of disease severity, bad prognostic factor and its presence is associated with increase probability of malaria. [7, 8]
Mixed infections with many etiologic agents are not uncommon in malaria. [15] Despite scant data, dengue and malaria coinfection should be common in areas where both diseases are co-endemic in many places of the world. [16] In a study regarding diagnostic techniques and management of dengue and malaria co-infection, all patients with dual infection presented prolonged fever for more than seven days, myalgia, bleeding manifestations, rash and anemia. [17] Moreover, according to Vasconcelos et al, the continuous fever caused by arboviral infection can mask the periodic fever associated with malarial parasites. [18]
Out of 159 thrombocytopenic cases presented with acute febrile illness, malaria was diagnosed in 55 (34.6%) cases while 34 (21.4%) of cases were diagnosed as dengue.
Of the 89 patients of dengue and malaria in this study, 5.6% had concurrent dengue and malaria. This percentage is relatively high as compared with other international studies. A study from France reported that 1% concurrent dengue and malaria. [19] Another study from Brazil reported 1.8% concurrent dengue and malaria. [20]
Very high percentage was found in a local study Ali et.al showed that Out of 11 patients diagnosed as having dengue fever on serology 9 (81.8%) also had co-existence of malaria and thrombocytopenia was present in 90% of such patients. [5]
In this study from 9 positive cases of co-infection, 3 (60%) were male and 2 (40%) were female. Mean (±SD) age of positive cases of co-infection was 37.8 (±8.3) years.
Although a reduced sample number was assessed in this study, a limitation that we acknowledge, it is important to remember that dengue and malaria co-infection requires special attention because delayed diagnosis and appropriated treatment can result in fatal complications. [16, 21] Both diseases causes similar symptoms and simultaneous infections with two different infectious agents may result in overlapped symptoms, [22] diagnosis of malaria and dengue based purely on clinical grounds may become difficult for physicians [16] and it is possible that either clinical spectrum of the disease or treatment may also be affected. [23] Finally, it is important to remember that both diseases have similar clinical findings, thus the diagnosis could be made concomitantly for dengue and malaria in patients living or returning from areas where both diseases are endemic or during dengue outbreaks.
CONCLUSION
Concurrent infections were found 5.7% in this study. Although this percentage is slightly low; special attention should be given to the possibility of co-infection with malaria and dengue. The distinction between severe dengue and severe malaria must be made in an emergency department or hospital setting because in both situations, early diagnosis is essential for patient care.
Finally, it is important to remember that both diseases have similar clinical findings, thus the diagnosis could be made concomitantly for dengue and malaria in patients living or returning from areas where both diseases are endemic or during dengue outbreaks.
Acknowledgement: We would like to acknowledge faculty of Ziauddin Hospital, North Campus for helping us during the study, staff for helping in data collection and all others who have given their input.
REFERENCE
- Rigau-Perez JG, Clark GG, Gulber DJ, Reitee P, Sanders EJ, Vorndam AV. Dengue and dengue hemorrhagic fever. Lancet 1998;352:971-7.
- Henchal EA, Putnak JR. The dengue viruses. Clin Microbiol Rev 1990;3: 376-96.
- Pinheiro FP, Corber SJ. Global situation of dengue and dengue hemorrhagic fever and its emergence in Americas. World Health Stat 1997;50:161-9.
- Guzman MG, Kouri G. Dengue: an update. Lancet infect Dis 2002;2:33-42.
- Ali N, Nadeem A, Anwar M, Tariq WZ, Chotani RA. Dengue fever in malaria endemic areas. J Coll Physicians Surg Pak 2005;16:340-42.
- Ahmed S, Ali N, Ashraf S, Ilyas M, Tariq WZ, Chotani RA. Dengue fever outbreak: A clinical management experience. J Coll Physicians Surg Pak 2008;18:8-12.
- Mahmood A, Yasir M. Thrombocytopenia; a predictor of malaria among febrile patients in Liberia. Infect Dis J Pak 2005;14:41-4.
- Lathia TB, Joshi R. Can hematological parameters discriminate malaria from nonmalarious acute febrile illness in the tropics? Indian J Med Sci. 2004;58:239-44.
- Charrel RN, Brouqui P, Foucault C, de Lamballerie X. Concurrent dengue and malaria. Emerg Infect Dis. 2005;11:1153–4.
- Deresinski S. Concurrent Plasmodium vivax malaria and dengue. Emerg Infect Dis. 2006;12:1802.
- Thangaratham PS, Jeevan MK, Rajendran R, Samuel PP, Tyagi BK. Dual infection by dengue virus and Plasmodium vivax in Alappuzha District, Kerala, India. Jpn J Infect Dis. 2006;59:211–2.
- Ward DI. A case of fatal Plasmodium falciparum malaria complicated by acute dengue fever in East Timor. Am J Trop Med Hyg. 2006;75:182–5.
- Allwinn R. Doerr HW, Emmerich P, Schmitz H, Preiser W. Crossreactivity in fl avivirus serology: new implications of an old fi nding? Med Microbiol Immunol. 2002;190:199–202.
- Dussart P, Labeau B, Lagathu G, Louis P, Nunes MR, Rodrigues SG, et al. Evaluation of an enzyme immunoassay for detection of dengue virus NS1 antigen in human serum. Clin Vaccine Immunol. 2006;13:1185–9.
- Singhsilarak T, Phongtananant S, Jenjittikul M, Watt G, Tangpakdee N, Popak N, et al. Possible acute coinfections in Thai malaria patients. Southeast Asian J Trop Med Public Health 2006;37:1-4.
- Ward DI. A case of fatal Plasmodium falciparum malaria complicated by acute dengue fever in East Timor. Am J Trop Med Hyg 2006;75:182-5.
- Abbasi A, Butt N, Sheikh QH, Bhutto AR, Munir SM, Ahmed SM. Clinical Features, Diagnostic Techniques and Management of Dual Dengue and Malaria Infection. J Coll Physicians Surg Pak 2009;19:25-9.
- Vasconcelos PFC, Rosa APAT, Rosa JFST, Dégallier N. Concomitant Infections by Malaria and Arboviruses in the Brazilian Amazon Region. Rev Latinoam Microbiol 1990;32:291-4.
- Carme B, Matheus S, Donutil G, Raulin O, Nacher M, Morvan J. Concurrent Dengue and Malaria in Cayenne Hospital, French Guiana. Emerg Infect Dis 2009;15:668-71.
- Santana VD, Lavezzo LC, Mondini A, Terzian AC, Bronzoni RV, Rossit AR et al. Concurrent dengue and malaria in the Amazon region. Rev Soc Bras Med Trop 2010;43:508-11
- Charrel RN, Brouqui P, Foucault C, Lamballerie X. Concurrent Dengue and Malaria. Emerg Infect Dis 2007;11:1153-4.
- Bhalla A, Sharma N, Sharma A, Suri V. Concurrent infection with Dengue and Malaria. Indian J Med Sci 2006;60:330-1.
- Tangaratham PS, Jeevan MK, Rajendran R, Samuel PP, Tyagi BK. Dual Infection by Dengue Virus and Plasmodium vivax in Alappuzha District, Kerala, India. Jpn J Infect Dis 2006;59:211-2.
Cite This Work
To export a reference to this article please select a referencing style below:

