This paper will be discussing Mr-T, a 40-year old male who attended the family screening clinic, referred for an exercise treadmill test (ETT) to rule out long QT-syndrome (LQTS) due to a family history of LQTS and a recent sudden cardiac death (SCD). Mr-T denied any symptoms of seizures, dizziness or syncope, otherwise fit and healthy and on no current medications, see figure-1 for a detailed overview of Mr-T’s pathway. The pathophysiology of LQTS, clinical-features, investigations alongside communication strategies of healthcare professionals will be discussed.
Pathophysiology and Clinical Features
LQTS is a channelopathy of the cardiac electrical system identified by ventricular arrhythmias, syncope and SCD [1]. LQTS is a rare condition, either inherited through abnormal genes or acquired secondary to medications [2], affecting approximately 1 in every 2000 individuals [3]. Studies have suggested due to a lack of recognition LQTS true prevalence is underestimated [9]. LQTS can induce life-threatening arrhythmias (Torsade de Pointes, ventricular fibrillation) which stimulate an abnormal function of the heart and reduce cardiac output [2]. Consequently, a lack of oxygen to the brain causes syncope and death if not treated with a shock. It is, therefore, imperative LQTS is diagnosed and treated to prevent SCD [3].
The pathogenesis of cardiac arrhythmia has led to a substantial advancement in its clinical treatment and management. Ion channels are responsible for the cardiac action potential, which produce excitation and contraction of the cardiac muscle. Modification and mutations of these channels result in the manifestation of disease [8]. The primary ionic compounds which undergo abnormal modifications include Ca2+,K+ or Na+, these modifications lengthen or reduce the repolarisation phase of the ventricles, this creates a foundation for an electrophysiological heterogenic substrate which incites the development of ventricular arrhythmias [4]. Clinical representation of LQTS is identified by a prolonged QT interval on an ECG [8,9]. LQTS is acknowledged via a prolonged QT interval on the ECG however, initially patients present following episodes of syncope or post SCD in young family members [9].
Investigations
|
Table-1 |
|
|
Investigations |
Findings |
|
Height and weight |
Weight: 60kg Height: 170cm |
|
12- Lead ECG |
Normal Sinus rhythm |
|
Exercise Tolerance Test |
Abnormal QTc findings |
|
Echocardiogram |
To assess the structure and function of the heart. Normal Echo parameters |
|
Genetic testing |
Referral to a geneticist for a confirmed diagnosis of LQTS type post positive ETT findings. |
Genetic testing has proven to be a prevailing diagnostic tool nonetheless, the controversial issue of its expenses and availability remain a major drawback in the forefront of its diagnostic and treatment viability [1]. Thus far LQT1, LQT2 and LQT3 are the gene mutations which have been primarily recognised [1,4]. Research suggests a disparity in the prognosis and treatment amongst different phenotypes of LQTS as the representation of clinical features differs amongst them [9].
Further speculation and reliable strategic testing could provide advancement in the treatment of LQTS whereby reduction in morbidity and mortality can result from early onset diagnosis [1, 5]. 12-Lead ECG is a simple yet effective diagnostic tool, representing the electrical activity of the heart, allowing the measurement of the QT interval [8] Arguably, the diagnosis of LQTS remains a challenging area as not all patients present with the typical symptoms and often the clinical diagnosis of long-QT is overlooked particularly in patients with borderline abnormalities on ECG [1]. Mr-T’s ECG showed negative findings however, due to his family history of SCD and LQTS he was subsequently referred for exercise testing which led to the diagnosis of LQTS. If Mr-T did not have a relevant history would he have been referred? This highlights the importance of good medical history taking [11,12].
ETT has been used as a tool for the diagnosis of LQTS particularly during the recovery phase post-exercise. During a normal physiological response to exercise, the QT shortens, however, research has found an inability of the QT interval to decrease with exercise in patients with LQTS [6,7]. Syl [10] suggests QT prolongation during 4 minutes of recovery can be used as a diagnostic measure for LQTS in asymptomatic patients. Conversely, research has proposed a disparity in QT patterns during exercise amongst patients with LQT1 and LQT2 [13]. Perhaps, the discrepancy between the number of subjects within each group (LQT1, LQT2) affected the validity of findings. Additionally, a modified version of the standard ETT protocol was utilised [14]. Nonetheless, ETT remains to be a significant diagnostic tool and proved to be beneficial in the diagnosis of LQTS for Mr-T [15].
Treatment
The management pathway profoundly differs amongst the three genetic variants of LQTS [22]. Mr-T’s ETT findings are suggestive of LQT1 as it is thought to result from stress or exercise [23]. However, as there are now more than three genotypes identified it is important that Mr-T undergoes genetic testing to gain confirmation of his diagnosis prior to the commencement of management plans [24]. This was the general consensus post MDT discuss amongst the cardiologist and therefore it was concluded that Mr-T is commenced on beta-blockers as a preventative form of treatment [18,22].
According to the ESC guidelines, Beta-blocker therapy has been advised as a first line of approach towards patients with inherited LQTS but excluding those who have experienced cardiac arrest generated as a result of LQTS [20]. Post consultation with the Cardiologist and in consideration of Mr-T’s age (40yrs), he was commenced on beta-blockers despite his asymptomatic representation and no previous cardiac events. Research suggests those with no previous history of events have their first episode above the age of 40 [17,18]. The efficacy of beta-blockers has been speculated as recent research has demonstrated an inconsistency in the pharmacological effects of different beta-blockers families [21] Debatably, the study did not consider drug interaction and participants medication history considering Long-QT can be both acquired and exacerbated secondary to medication[2], furthermore no deliberation was made on the LQTS phenotype [20].
If Mr-T has a confirmed diagnosis of LQT1 post genetic testing and becomes symptomatic in the future, a combination of beta-blocker treatment and pacemaker implantation is advised [22]. The psychosocial impact of such decisions on Mr-T need to be considered with precaution, for an effective relay of treatment plans between the cardiologist and Mr-T requires good communication [35]. Research suggests communications as the prime component in the delivery of care which enhances the ability to identify patients’ requirements, expectations and sensitivity [36].
Role of Multidisciplinary team and communication strategies
|
Table-2 |
|
|
Care providers |
Professionals involved |
|
Primary |
GP - Initial recipient and referrer for further diagnostic testing. A primary role player in commencing the patient pathway. |
|
Secondary |
Cardiographer – performed the 12 Lead ECG Cardiac Physiologist – performed and reported the ETT test. |
|
Tertiary |
Multi-disciplinary team – a team of cardiologists who discussed Mr-Ts case and reviewed management and treatment strategies. Cardiologist - consultation with the patient to discuss diagnosis and treatment plans Geneticist– Will be involved in diagnosing the type of LQTS gene Mr-T has inherited and therefore this will influence the treatment plans. |
Different professions played a part in the diagnosis and care of Mr-T (see figure-1 & table-2), all contributing towards the diagnosis of Mr-T’s condition. In the NHS teamwork plays a fundamental role which requires good communication strategies. West [25] identified two major elements within teamwork which include social reflectivity and task, his work described four types of teams out of which the most effective team was described with high task and social reflectivity levels [25]. Forehand [30], explores the concept of the Ringle-mann effect which suggests individuals exert less effort when part of a team working on a shared task, it can be queried whether the diagnosis of Mr-T’s condition could have been diagnosed earlier i.e. a preliminary referral for genetic testing post-normal ECG findings by the MDT team prior to an ETT. Considering the team was aware of Mr-T’s family history it would have reduced the time loss in diagnosis and commencement of treatment [30].
Patient management, shared decision making (SDM) and communication strategy coincide and therefore require equal importance by the physician when deliberating treatment options [19]. Mr-T condition may subject to change in the future; therefore, it is necessary that he is adequately informed in relation to his condition with regards to management plans and future implications. SDM is a process currently under development but has proven beneficial outcomes permitting patients to have an improved awareness of their condition and a support system available when deliberating their choices for treatment [19]. SDM complements the NHS constitutions which aim to provide patient-centred care and to safeguard the rights of patients, ensuring professionalism, care, and compassion whilst reducing the vulnerability of patients [26]. Montgomery ruling is a fine example that highlights the importance of and a need for SDM [27]. During the consultation Mr-T’s Cardiologist should realise that there are two experts in the decision-making process: Mr-T and the cardiologist, each contributes different skills, but they are equally important for the final decision, giving a voice to Mr-T [28,29]. When offering genetic testing Ethics and Mr-Ts consent should be highly regarded. He is a young man therefore, a heavy phycological impact may follow as this affects his wife, children and future family-planning [37].
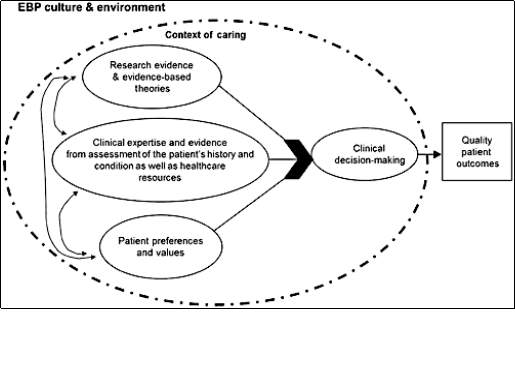
Mr-T was being investigated in a tertiary hospital which has a paperless system this conducted efficiency in the work ethic as the reports from diagnostic tests immediately transferred onto the online database which can be accessed by all professionals within the hospital. This created a basis for good communication dynamics since there were no gaps in communication as all letters, test results, and history was well documented and available for the knowledge of the next professional involved the care-pathway for Mr-T [31]. It is a good source of evidence-based practice as there will be lower chances of misplacement and loss of test results which help to prevent duplicate test referrals, see figure 2 [32].
Nonetheless, how useful is the paperless system and did the team utilize the ECG results which could have directed for initial genetic testing rather than an ETT [33]. It is arguable whether verbal communication could have improved the management of Mr-T compared to excessive reliance upon the paperless system. This would have assisted in reducing Mr-T’s apprehension, research has demonstrated poor patient outcomes with poor interprofessional communication. Therefore, it is important to maintain an equilibrium between the paperless system and verbal communication [34]. 
Conclusion
Medicine in the current times is cutting edge providing the best care for patient management and diagnosis. Yet, there continues to be a gap between the practical, psychosocial and communication element of patient experience. Which if improved could improve patient outcomes this requires further training in effective communication strategy as identified in Mr-T’s case.
REFERENCING
- Wong, J. Gula, L. Klein, G. Yee, R. Skanes, A, Krahn, A. 2010. Utility of treadmill testing in identification and Genotype prediction in Long QT Syndrome. Circulation: Arrhythmia and Electrophysiology. 2010 January 9; 3: 120-125 https://www.ahajournals.org/doi/full/10.1161/CIRCEP.109.907865?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub%3Dpubmed&
- Arrhythmia Alliance. Long QT syndrome [pamphlet] UK: Heart rhythm Alliance; 2019.
- NHS. Long QT syndrome. [internet] UK. NHS; [updated 2017 November 14; cited 2019 December 22] Available from: https://www.nhs.uk/conditions/long-qt-syndrome/
- Morita, H. Wu, Jiashim. Zipes, D. The QT syndromes: long and short. The Lancet. 2008 August 30; 372 (9640): 750-763. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(08)61307-0/fulltext
- Ackerman, M. Splawski, I. Makielski, J. Tester, D. Will, M. Timothy, k. Keating, M. Jones, G. Chadha, M. Burrow, C. Stephens, C. Xu, C. Judson, R. Curran, M. 2004. Spectrum and prevalence of cardiac sodium channel variants among black, white, Asian and Hispanic individuals: Implications for arrhythmogenic susceptibility and Brugada/Long QT syndrome genetic testing. Heart Rhythm. 2004 Novemeber; 1 (5): 600-607. https://www.heartrhythmjournal.com/article/S1547-5271(04)00404-7/fulltext
- Schwartz, P. Crotti, L. QTc behaviour during exercise and genetic testing for the Long-QT syndrome. Circulation. 2011 November 15. 124 (20): 2181-2184. https://ahajournals.org/doi/full/10.1161/circulationaha.111.062182
- Hayashi, K. Konno, T. Fujino, N. Itoh, H. Fuji, Y. Imi-Hashida, Y. Tada, H. Tsuda, T. Tanaka, Y. Saito, T. Ino, H. Kawashiri, M. Ohta, K. Horie, M. Yamagishi, M. Impact of Updated Diagnostic Criteria for Long QT syndrome on clinical detection of diseased patients: Results from a study of patients carrying Gene mutations. JACC Clinica Electrophysiology. 2016 June; 2(3): 279-287. https://www.sciencedirect.com/science/article/pii/S2405500X16000128
- Bohnen, M. Peng, G. Robey, S. Terrenoire, C. Iyer, V. Sampson, K. Kass, R. Molecular pathophysiology of congenital long QT syndrome. Physiological Reviews. 2016 November 2. 97(1): 89-134. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5539372/
- Saprungruang, A. Vithessonthi, K. La-orkhun, V. Lertsapcharoen, P. Khongphatthanayothin, A. Clinical presentation and course of long QT syndrome in Thai children. Journal of Arrhythmia. 2015 October 31; 31(5): 296-301https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4600892/
- Sy, R. Werf, C. Chattha, I. Chockalingam, P. Adler, A. Healey, J. Perrin, M. Gollob, M. Skanes, A. Yee, R. Gula, L. Leong-sit, P. Viskin, S. Klein, G. Wilde, A. Krahn, A. Derivation and validation of a simple exercise-based algorithm for prediction of genetic testing in relatives of LQTS Probands. Circulation. 2011 October 31; 124 (20): 2187-2194 https://ahajournals.org/doi/10.1161/circulationaha.111.028258
- Ghosh, D. Karunaratne, P. The importance of good history taking: a case report. Journal of Medical case reports. 2015 April 30; 9(1):1-3 https://jmedicalcasereports.biomedcentral.com/articles/10.1186/s13256-015-0559-y
- Tan,B. Judge, D. A Clinical Approach to a family history of sudden death. Circulation. 2012; 5:697-705. https://www.ahajournals.org/doi/10.1161/CIRCGENETICS.110.959437
- Horner, J. Horner, M. Ackerman, M. The diagnostic utility of recovery phase QTc during treadmill exercise stress testing in the evaluation of long QT syndrome. Heart Rhythm Society. 2011 November; 8 (11): 1698-1704. https://www.heartrhythmjournal.com/article/S1547-5271(11)00605-9/pdf
- Perez-Riera, A. Barbosa-Barros, R. Raimundo, R. Barbosa, M. Sorpreso, I. Abreu, L. The congenital Long QT syndrome Type 3: An update. Indian Pacing Electrophysiology Journal. 2017 October 31; 18(1): 25-35. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5840852/
- Raju, H. Papadakis, M. Bastiaenen, R. Zaidi, A. Chandra, N. Muggenthaler, M. Spath, N. Sharma, S. Behr, E. 50 Diagnostic role of exercise tolerance testing in familial premature sudden cardiac death. Heart. 2011; 97 (1):1. https://heart.bmj.com/content/97/Suppl_1/A33.2#request-permissions
- Weiss, J. Shivkumar, K. Electrophysiology of hypokalaemia and hyperkalaemia. Circulation: Arrhythmia and Electrophysiology. 2017 March 17; 10(3): 1-10. https://www.ahajournals.org/doi/full/10.1161/CIRCEP.116.004667
- Schwartz, P. Crotti, L. Insolia, R. Long QT syndrome: From Genetics to management. Circulation: Arrhythmia Electrophysiology. 2012 August 1; 5(4):868-877. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3461497/
- Al-khatib, S. Stevenson, W. Ackerman, M. David, B. Anne, C. Deal, B et al. A report of the American College of Cardiology/American Heart association Task force on clinical practice guidelines and the heart rhythm society. Journal of American College of Cardiology. 2018 October; 72 (14):1677- http://www.onlinejacc.org/content/72/14/1677/T33
- Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared Decision Making: A Model for Clinical Practice. Journal of General Internal Medicine. 2012 May 23;27(10):1361–1749. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445676/
- Ackerman MJ, Priori SG, Dubin AM, Kowey P, Linker NJ, Slotwiner D, et al. Beta-blocker therapy for long QT syndrome and catecholaminergic polymorphic ventricular tachycardia: Are all beta-blockers equivalent? Heart Rhythm. 2017 Jan;14(1):e41–4. Available from: https://www.heartrhythmjournal.com/article/S1547-5271(16)30760-3/pdf
- Chockalingam P, Crotti L, Girardengo G, Johnson JN, Harris KM, van der Heijden JF, et al. Not All Beta-Blockers Are Equal in the Management of Long QT Syndrome Types 1 and 2. Journal of the American College of Cardiology. 2012 Nov 13;60(20):2092–9. Available from: https://www.sciencedirect.com/science/article/pii/S0735109712042337?via%3Dihub
- Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. Circulation. 2018 Sep 25 ;138(13). Available from: https://www.ahajournals.org/doi/abs/10.1161/CIR.0000000000000549
- Schwartz PJ, Crotti L, Insolia R. Long-QT Syndrome. Circulation: Arrhythmia and Electrophysiology. 2012 Aug 1;5(4):868–77. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3461497/
- Giudicessi JR, Ackerman MJ. Genotype- and Phenotype-Guided Management of Congenital Long QT Syndrome. Current Problems in Cardiology. 2013 October; 38(10):417–55. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3940076/
- West M. Effective Teamwork: Practical Lessons from Organisational Research. 3rd ed. Sussex: British Psychological Society and John Wiley & Sons, Ltd; 2012. https://download.e-bookshelf.de/download/0000/5962/42/L-G-0000596242-0002339025.pdf
- Gov.uk. NHS Constitution for England [Internet]. UK. Gov.uk; [updated 2015 October 14; cited 2019 December 28]. Available from: https://www.gov.uk/government/publications/the-nhs-constitution-for-england
- Chan SW, Tulloch E, Cooper ES, Smith A, Wojcik W, Norman JE. Montgomery and informed consent: where are we now? BMJ. 2017 May 12;357(10.1136):1–3. https://www.bmj.com/content/bmj/357/bmj.j2224.full.pdf
- Elwyn G, Laitner S, Coulter A, Walker E, Watson P, Thomson R. Implementing shared decision making in the NHS. BMJ. 2010 October 14; 341(c5145): 1
- Stacey G, Felton A, Morgan A, Stickley T, Willis M, Diamond B, et al. A critical narrative analysis of shared decision-making in acute inpatient mental health care. Journal of Interprofessional Care. 2016 Jan 2;30(1):35–41. Available from: http://www.criticalvaluesbasedpracticenetwork.co.uk/wp-content/uploads/a-critical-narrative-analysis-of-shared-decision-making-in-acute-in-patient-mental-health-care-1.pdf
- Forehand JW, Leigh KH, Farrell RG, Spurlock AY. Social dynamics in group work. Teaching and Learning in Nursing. 2016 Apr;11(2):62–6. https://www.sciencedirect.com/science/article/pii/S1557308715000955
- Adler-Milstein J, Bates DW. Paperless healthcare: Progress and challenges of an IT-enabled healthcare system. Business Horizons. 2010 March;53(2):119–30. Available from: https://www.sciencedirect.com/science/article/pii/S0007681309001529
- Melnyk BM, Gallagher-Ford L, Long LE, Fineout-Overholt E. The Establishment of Evidence-Based Practice Competencies for Practicing Registered Nurses and Advanced Practice Nurses in Real-World Clinical Settings: Proficiencies to Improve Healthcare Quality, Reliability, Patient Outcomes, and Costs. Worldviews on Evidence-Based Nursing. 2014 Jan 21;11(1):5–1
- NHS England. NHS England » Cutting reliance on paper will make patients safer, says NHS England [Internet]. England.nhs.uk. NHS; [updated: 2015 September 1; cited 2019 December 29]. Available from: https://www.england.nhs.uk/2015/09/cutting-reliance-on-paper/
- Foronda C, MacWilliams B, McArthur E. Interprofessional communication in healthcare: An integrative review. Nurse Education in Practice. 2016 Jul;19(19):36–40. https://www.sciencedirect.com/science/article/pii/S1471595316300208
- Tominaga T, Matsushima M, Nagata T, Moriya A, Watanabe T, Nakano Y, et al. Psychological impact of lifestyle-related disease disclosure at general checkup: a prospective cohort study. BMC Family Practice. 2015 May 14;16(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4437684/
- Ha JF, Longnecker N. Doctor-patient communication: a review. The Ochsner journal. 2010;10(1):38–43. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096184/
- Mcquillan GM, Porter KS, Agelli M, Kington R. Consent for genetic research in a general population: The NHANES experience. Genetics in Medicine. 2003 January 1;5(1):35–42. Available from: https://www.nature.com/articles/gim20036
- Foronda C, MacWilliams, B, McArthur E. Interprofessional communication in healthcare: An integrative review. Nursing Education in Practice. 2016
Cite This Work
To export a reference to this article please select a referencing style below:

