Rheumatoid Arthritis with Hip Arthroplasty
S.P. is admitted to the orthopedic ward. She has fallen at home and has sustained an intracapsular fracture of the hip at the femoral neck. The following history is obtained from her: *She is a *75-year-old widow with three children living nearby. Her father died of cancer at age 62; mother died of heart failure at age 79. Her height is 5 feet 3 inches; weight is 118 pounds. She has a *50-pack-year smoking history and denies alcohol use. She has severe rheumatoid arthritis (RA), with evidence of cartilage and bone destruction, along with joint deformities. She had an upper gastrointestinal bleed in 1993, and had coronary artery disease with a coronary artery bypass graft 9 months ago. Since that time she has engaged in* “very mild exercises at home.” Vital signs (VS) are 128/60, 98, 14, 99° F (37.2° C), SaO2 94% on 2 L oxygen by nasal cannula. Her oral medications are *rabeprazole (Aciphex) 20 mg/day, *prednisone (Deltasone) 5 mg/day, and *methotrexate (Amethopterin) 2.5 mg/wk.
**What anatomical stage of Rheumatoid Arthritis does SP have? (1)
Stage I-Early
No destructive changes on radiograph, possible radiographic evidence of osteoporosis
Stage II-Moderate
Radiographic evidence of osteoporosis, with or without slight bone or cartilage destruction, no joint deformities (although possibly limited joint mobility), adjacent muscle atrophy, possible presence of extra-articular soft-tissue lesions (e.g., nodules, tenosynovitis)
Stage III-Severe
Radiographic evidence of cartilage and bone destruction in addition to osteoporosis; joint deformity, such as subluxation, ulnar deviation, or hyperextension, without fibrous or bony ankylosis; extensive muscle atrophy; possible presence of extra-articular soft-tissue lesions (e.g., nodules, tenosynovitis)
Stage IV-Terminal
Fibrous or bony ankylosis, stage III criteria
- List at least four risk factors for hip fractures. (4 pts)
Age. The risk for hip fractures increases as we age. In 2010, more than 80% of the people hospitalized for hip fractures were age 65 and older, according to the National Hospital Discharge Survey (NHDS).
Sex. About 70 percent of hip fractures occur in women. Women lose bone density at a faster rate than men do, in part because the drop in estrogen levels that occurs with menopause accelerates bone loss. However, men also can develop dangerously low levels of bone density.
Cortisone medications, such as prednisone, can weaken bone if taken for long term. Rabeprazole (Aciphex) and methotrexate (Amethopterin) could cause dizziness and more prone to falling.
Physical inactivity (“very mild exercises at home”). Weight-bearing exercises, such as walking, help strengthen bones and muscles, making falls and fractures less likely. Not participating in regularly weight-bearing exercise, may lead to lower bone density and weaker bones.
Tobacco use. Can interfere with the normal processes of bone building and maintenance, resulting in bone loss.
2.Place a star or asterisk next to each of the responses in question 1 that represent S.P.’s risk factors. (1)
Case Study Progress
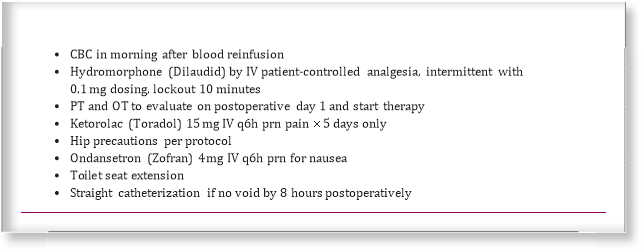
S.P. is taken to surgery for a total hip replacement. Because of the intracapsular location of the fracture, the surgeon chooses to perform an arthroplasty rather than internal fixation. The postoperative orders include:
Chart View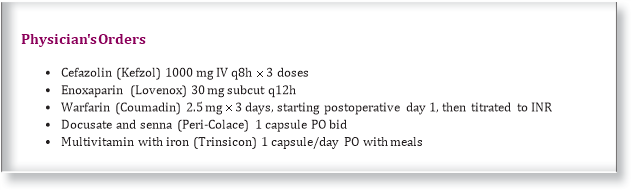
- Why is the patient receiving enoxaparin (Lovenox) and warfarin (Coumadin)? (4 pts) In your answer, also explain how these 2 medications are used together and the rationale behind how they are used.
Deep venous thrombosis (DVT) may form in leg veins as a result of inactivity, body position, and pressure, all of which lead to venous stasis and decreased perfusion. DVT, especially common in older adults and obese or immobilized individuals, is a potentially life-threatening complication because it may lead to pulmonary embolism.
The most commonly used anticoagulants are unfractionated heparin (UH), low-molecular weight heparins (LMWHs), hirudin derivatives, and coumarin compounds. Unfractionated heparin (heparin sodium, commonly known as heparin) acts directly on the intrinsic and the common pathways of blood coagulation. Heparin inhibits thrombin-mediated conversion of fibrinogen to fibrin. It also potentiates the actions of antithrombin III, inhibits the activation of factor IX, and neutralizes activated factor X by activating factor X inhibitor.
LMWH is effective for the prevention and treatment of DVT. LMWHs are derived from heparin, but the molecule size is approximately one third that of heparin. Enoxaparin (Lovenox), dalteparin (Fragmin), and ardeparin (Normiflo) are examples of LMWHs. LMWH has a greater bioavailability, more predictable dose response, and longer half-life than heparin with less risk of bleeding complications. LMWH has the practical advantage that it does not require anticoagulant monitoring and dose adjustment ( Hirsh , Bauer , Donati , Gould , Samama , & Weitz , 2008). LMWH is administered subcutaneously in fixed doses, once or twice daily.
Coumarin compounds, of which warfarin (Coumadin) is the most commonly used, exert their action indirectly on the coagulation pathway. Warfarin inhibits the hepatic synthesis of the vitamin K- dependent coagulation factors II, VII, IX, and X by competitively interfering with vitamin K. Vitamin K is normally required for the synthesis of these factors. Oral anticoagulants are often administered concurrently with heparin. Warfarin requires 48 to 72 hours to influence prothrombin time (PT) and may take several days before maximum effect is achieved. Therefore a 3- to 5-day overlap of heparin and warfarin is required. The clotting status should be monitored by activated partial thromboplastin time (aPTT) for heparin therapy and the international normalized ratio (INR) for coumadin derivatives. The INR is a standardized system of reporting PT based on a referenced calibration model and calculated by comparing the client’s PT with a control value. Other tests to monitor anticoagulation may be used. For DVT prophylaxis, low-dose unfractionated heparin, LMWH, or warfarin (Coumadin) can be prescribed depending on the client’s level of risk and weight. Unfractionated heparin is typically taken by subcutaneous (subQ) route and prescribed at 5000 units q12h subQ for clients at low and moderate risk or 3500 to 5000 units q8h subQ for clients at high risk. LMWH is usually scheduled at 30 mg q12h subQ or 40 mg daily subQ. LMWH is rapidly replacing heparin as the anticoagulant of choice to prevent DVT in clients at high risk. In fact, LMWH is considered the most effective form of prophylaxis in hip surgery, in knee surgery, and following major trauma. Low-dose warfarin is usually reserved for clients with the highest DVT risk.
It is quite common for a person to be taking both Coumadin and Lovenox at the same time. Lovenox begins working right away, while Coumadin does not. In fact, in the period of time when a person first begins taking Coumadin, the drug may actually increase the risk of clots for a short period of time. Therefore, Coumadin and Lovenox are often taken together. The Lovenox prevents clots while the Coumadin begins working. The Lovenox can be stopped once the INR is in the appropriate range.
4.S.P. received blood as an intraoperative blood salvage. Which statements about this procedure are true? (Select all that apply.)
a.The blood that is lost from surgery is immediately re-administered to the patient (Salvaged blood should be washed. Salvaged blood that is not washed or otherwise processed (eg, centrifuged) has low hemoglobin levels (7 to 9 g/dL), residual anticoagulant, dysfunctional platelets, thrombogenic substances, free hemoglobin levels, and fat emboli that might lead to coagulation abnormalities).
b.(True) The blood lost from surgery is collected into a cell saver
(Centrifuge-based RBC salvage with the intraoperative cell salvage machine (commonly referred to as a “cell saver”) starts with the surgeon aspirating blood from the surgical field through a suction wand. The blood is mixed with an anticoagulant as it is aspirated (eg, heparin or citrate) to prevent coagulation [16]. Typically, heparin in saline with a concentration of about 30,000 units/L is used. This solution is slowly and automatically added to the aspirated blood at a rate of 15 mL per 100 mL of collected blood [16]. During subsequent washing of the collected blood, all but a trace of heparin is removed).
c.One hundred percent of the red blood cells are saved for reinfusion (other components in the blood such as platelets and contaminants can also adhere to these filters, but at least 85 percent of RBCs pass through the filter and into the patient).
d. This procedure has the same risks as blood transfusions from donors.
e.(True) The salvaged blood must be reinfused within 6 hours of collection. (Blood collected by intraoperative blood salvage may be stored either at room temperature for up to six hours or at 1 to 6°C for up to 24 hours, provided that blood is collected under aseptic conditions with a device that provides washing and that cold storage is begun within six hours of initiating the collection. Such stored blood must be properly labeled).
- List four critical potential postoperative problems for S.P. (4 pts)
Infection. Fever above 38°C (100.4°F) is common in the first few days after major surgery. Most early postoperative fever is caused by the inflammatory stimulus of surgery and resolves spontaneously. However, postoperative fever can be a manifestation of a serious complication. A thorough differential diagnosis of postoperative fever includes infectious and noninfectious conditions that occur following surgery. Fever may arise due to a surgical site infection (SSI), or from other hospital-related conditions, including nosocomial pneumonia, urinary tract infection, drug fever, and deep vein thrombosis. In evaluating a postoperative patient with fever, it is important to consider a broad differential, and not to assume that fever is due to infection. Fever as a manifestation of infection may be reduced or absent in immunocompromised patients including those receiving glucocorticoids, cancer chemotherapy, post-transplant immunosuppression, and also in some patients who are elderly or have chronic renal failure.
Hypoxemia, specifically a PaO2 of less than 60 mm Hg, is characterized by a variety of nonspecific clinical signs and symptoms, ranging from agitation to somnolence, hypertension to hypotension, and tachycardia to bradycardia. Pulse oximetry will indicate a low oxygen saturation (below the 90 to 92% range). Arterial blood gas analysis may be used to confirm hypoxemia if the pulse oximetry indicates a low O2 saturation. Low oxygen saturation may be corrected by encouraging deep breathing and coughing or by increasing the amount of oxygen delivered. The most common cause of postoperative hypoxemia is atelectasis. Atelectasis (alveolar collapse) may be the result of bronchial obstruction caused by retained secretions or decreased respiratory excursion. Hypotension and low cardiac output states can also contribute to the development of atelectasis. Other causes of hypoxemia that may occur in the PACU include pulmonary edema, aspiration, and bronchospasm.
Hypotension is evidenced by signs of hypoperfusion to the vital organs, especially the brain, the heart, and the kidneys. Clinical signs of disorientation, loss of consciousness, chest pain, oliguria, and anuria reflect hypoxemia and the loss of physiological compensation. Intervention must be timely to prevent the devastating complications of cardiac ischemia or infarction, cerebral ischemia, renal ischemia, and bowel infarction. The most common cause of hypotension in the PACU is unreplaced fluid and blood loss; thus, treatment is directed toward restoring circulating volume. If there is no response to fluid administration, cardiac dysfunction should be presumed to be the cause of hypotension.
Deep venous thrombosis (DVT) may form in leg veins as a result of inactivity, body position, and pressure, all of which lead to venous stasis and decreased perfusion. DVT, especially common in older adults and obese or immobilized individuals, is a potentially life-threatening complication because it may lead to pulmonary embolism. Clients with a history of DVT have a greater risk for pulmonary embolism. Pulmonary embolism should be suspected in any client complaining of tachypnea, dyspnea, and tachycardia, particularly when the client is already receiving oxygen therapy. Manifestations may include chest pain, hypotension, hemoptysis, dysrhythmias, or heart failure. Definitive diagnosis requires pulmonary angiography. Superficial thrombophlebitis is an uncomfortable but less ominous complication that may develop in a leg vein as a result of venous stasis or in the arm veins as a result of irritation from IV catheters or solutions. If a piece of a clot becomes dislodged and travels to the lung, it can cause a pulmonary infarction of a size proportionate to the vessel in which it lodges.
- How will you monitor for excessive postoperative blood loss? (5 pts)
- Observe the dressing and incision for signs of bleeding
- Restlessness
- Confusion
- Anxiety
- Feeling of impending doom
- Decreased level of consciousness
- Weakness
- Rapid, weak, thread pulses
- Dysrhythmias
- Hypotension
- Narrowed pulse pressure
- Cool, clammy skin
- Tachypnea, dyspnea, or shallow, irregular respirations
- Decreased O2 saturation
- Extreme thirst
- Nausea and vomiting
- Pallor
- Cyanosis
- Obvious hemorrhage
The rate and volume of bleeding, vital signs, and laboratory results should be closely monitored to assess the best approach to and aggressiveness of intervention. It is important to not allow the patient to become moribund before initiating life-saving measures.
- Post op Day 1, S.P. states that she is having 8/10 pain. List 3 thingsthat you would assess in order to determine why she is having the pain and then state 2 nursing interventions. (5 pts)
Complications associated with femoral neck fracture include nonunion, AVN, dislocation, and degenerative arthritis.
Postoperative pain is usually most severe within the first 48 hours and subsides thereafter. Variation is considerable, according to the procedure performed and the client’s individual pain tolerance or perception. The client should be observed for indications of pain (e.g., restlessness) and questioned about the degree and characteristics of the pain. Identifying the location of the pain is important. Incisional pain is to be expected, but other causes of pain, such as a full bladder, may also be present. Pain assessments can be measured with a variety of scales such as asking a client to rate his or her pain on a scale of 0 to 10. Perform a comprehensive pain assessment to include the following: characteristic, onset and duration, quality, intensity and severity. In the early postoperative period, there is a potential for neurovascular impairment. The nurse assesses the client’s extremity for (1) colour, (2) temperature, (3) capillary refill, (4) distal pulses, (5) edema, (6) sensation, (7) motor function, and (8) pain.
- Provide client optimal pain relief with prescribed analgesic as ordered to relieve acute pain and to prevent pain from becoming too severe.
- Teach and assess client’s correct use of patient-controlled analgesia to ensure effectiveness.
- Use nonpharmacological interventions to relieve pain, such as distraction, massage, relaxation, and imagery, for client use in lieu of or in conjunction with analgesics to obtain pain relief.
- According to the lateral traditional surgical approach, there are two main goals for maintaining proper alignment of S.P.’s operative leg. What are they, and how are they achieved? (2 pts)
The client and the family must be fully aware of positions and activities that predispose the client to dislocation (greater than 90 degrees of flexion, adduction, or internal rotation). Many daily activities may reproduce these positions, including putting on shoes and socks, crossing the legs or feet while seated, assuming the side-lying position incorrectly, standing up or sitting down while the body is flexed relative to the chair, and sitting on low seats, especially low toilet seats. Until the soft tissue surrounding the hip has healed sufficiently to stabilize the prosthesis, usually for at least 6 weeks, these activities must be avoided.
- Use elevated toilet seat
- Place chair inside shower or tub and remain seated while washing
- Use pillow between legs for first 8 weeks after surgery when lying on the side allowed by surgeon or when supine
- Keep hip in neutral, straight position when sitting, walking, or lying
- Notify surgeon if severe pain, deformity, or loss of function occurs
- Postoperative wound infection is a concern for S.P. Describe what you would do to monitor her for a wound infection. (4 pts)
Redness (rubor, hyperemia from vasodilation), heat (colour, increased metabolism at inflammatory site), pain (colour change in pH; change in local ionic concentration; nerve stimulation by chemicals (e.g.,histamine, prostaglandins; pressure from fluid exudate), swelling (tumour, fluid shift to interstitial spaces; fluid exudate accumulation), edge approximation, odor, type of exudate.
Vital signs, WBC.
- Taking S.P.’s RA into consideration: what interventions should be implemented to prevent complications secondary to immobility? (6 pts)
The physiotherapist usually supervises active-assistance exercises for the affected extremity and ambulation when the surgeon permits it. Ambulation usually begins on the first postoperative day. The nurse in collaboration with the physiotherapist monitors the client’s ambulation status. The ambulating client should pick up the feet rather than shuffling them so that muscular contraction is maximized. When confined to bed, the client should alternately flex and extend the legs. When the client is sitting in a chair or lying in bed, there should be no pressure to impede venous flow through the popliteal space. Crossed legs, pillows behind the knees, and extreme elevation of the knee gatch must be avoided. Some surgeons routinely prescribe use of elastic stockings or mechanical aids such as sequential compressive devices to stimulate and enhance the massaging and milking actions that are transmitted to the veins when leg muscles contract. The nurse must remember that these aids are useless if the legs are not exercised and may actually impair circulation if the legs remain inactive or if the devices are sized or applied improperly. When in use, elastic stockings must be removed and reapplied at least twice daily for skin care and inspection. The skin of the heels and posttibial areas is particularly susceptible to increased pressure and breakdown. The use of unfractionated heparin (UH) or low-molecular weight heparin (LMWH) is a prophylactic measure for venous thrombosis and pulmonary embolism. Advantages of LMWH over UH include (1) less major bleeding, (2) decreased incidence of thrombocytopenia, (3) better absorption, (4) longer duration of action, (5) as effective or more effective, and (6) no laboratory monitoring required.
A primary nursing responsibility is the identification of clients at risk for the development of pressure ulcers and implementing pressure ulcer prevention strategies for those identified as being at risk. Prevention remains the best treatment for pressure ulcers. Devices such as support surfaces, special transfer equipment, and heel boots are useful in reducing pressure and shearing force. However, they are not adequate substitutes for frequent repositioning.
The client’s position should be changed every 1 to 2 hours to allow full chest expansion and increase perfusion of both lungs. Ambulation, not just sitting in a chair, should be aggressively carried out as soon as physician approval is given. Adequate and regular analgesic medication should be provided because incisional pain often is the greatest deterrent to client participation in effective ventilation and ambulation. The client should also be reassured that these activities will not cause the incision to separate. Adequate hydration, either parenteral or oral, is essential to maintain the integrity of mucous membranes and to keep secretions thin and loose for easy expectoration.
Deep breathing and coughing techniques help the client prevent alveolar collapse and move respiratory secretions to larger airway passages for expectoration. The client should be assisted to breathe deeply 10 times every hour while awake. The use of an incentive spirometer is helpful in providing visual feedback of respiratory effort. The nurse should teach the client to use an incentive spirometer, which involves the following: inhale into the mechanism, hold the ball for about 3 seconds, and then exhale. This procedure should be done 10 to 15 times, and then the nurse should encourage the client to cough. It is recommended that an incentive spirometer should be used every 2 to 3 hours while awake.
Urinary tract infections are another risk for people who may spend long periods of time on their back. This can promote urinary stasis or stagnation in the flow of urine from the kidneys to the bladder, and thus, lead to infection. Prolonged immobility also causes an increase of minerals and salts to circulate in the blood that can promote the formation of kidney stones.
Constipation is a common problem that may result from decreased physical activity. Other factors may aggravate bowel evacuation. These include loss of privacy and embarrassment if toilet assistance is needed; uncomfortable positioning while using the commode; excessive delay in elimination because of the inconvenience in going to the bathroom; and the unavailability of caregiver assistance if help is needed to use the commode. Bowel irregularity may produce abdominal discomfort, as well as cause loss of appetite.
11.In patients with RA, very often Prednisone is prescribed for a patient with an acute exacerbation. Which laboratory result will the nurse monitor to determine whether the medication has been effective?(1 pt)
- Blood glucose test
- Liver function tests
- C-reactive protein level
- Serum electrolyte levels
Explain your answer (what does this test show?)
Data on high-sensitivity C-reactive protein have been reported, elevated levels of C-reactive protein appear to correlate best with symptoms of pain and stiffness rather than extent or progression of disease. To detect inflammation and test for the activity of the disease; may be used to help differentiate osteoarthritis and RA; an increased level of CRP occurs in RA but not in osteoarthritis.
12.A patient with an exacerbation of rheumatoid arthritis (RA) is taking prednisone 40 mg daily. Which of these assessment data obtained by the nurse indicate that the patient is experiencing a side effect of the medication? (1 pt)
- The patient’s blood glucose is 165 mg/dL (9.2 mmol/L).
- The patient has no improvement in symptoms.
- The patient has experienced a recent 5-pound (2.3 kilogram) weight loss.
- The patient’s erythrocyte sedimentation rate (ESR) has increased.
Prednisone is used as an anti-inflammatory or an immunosuppressant medication. Prednisone treats many different conditions such as allergic disorders, skin conditions, ulcerative colitis, arthritis, lupus, psoriasis, or breathing disorders. Long-term side effects include Cushing’s syndrome insulin resistance (especially common with ACTH production outside the pituitary), leading to high blood sugar and insulin resistance which can lead to diabetes mellitus. Insulin resistance is accompanied by skin changes such as acanthosis nigricans in the axilla and around the neck, as well as skin tags in the axilla.
13.What predisposing factor, identified in S.P.’s medical history, places her at risk for infection, bleeding, and anemia? (1 pt)
Medication administration rabeprazole (Aciphex) 20 mg/day, *prednisone (Deltasone) 5 mg/day, and *methotrexate (Amethopterin) 2.5 mg/wk
History of upper gastrointestinal bleed in 1993, and had coronary artery disease with a coronary artery bypass graft 9 months ago
50-pack-year smoking history
14.Briefly discuss S.P.’s nutritional needs. (2 pts)
As a person grows older, there are decreases in lean body mass (the metabolically active tissue), basal metabolic rate, and physical activity. Combined, these factors decrease the caloric needs for energy. The older person frequently reduces the consumption of needed protein, vitamins, and minerals and may take in “empty calories,” such as candy and pastries. When these factors are added to already existing medical problems, it is easy to see why poor dietary practices develop. In addition, poor dentition, ill-fitting dentures, anorexia, multiple losses affecting the social setting of meals, low income, and medical conditions involving the GI tract play a role in the type and amount of foods that are eaten. Socioeconomic factors are of critical importance when assessing the nutritional status of an older adult.
The nurse must be aware of common medical and psychosocial factors in the older adult and should incorporate interventions for overcoming these problems in the plan of care. Some of the physiological changes associated with aging affect the nutritional status of older adults. The following changes are of particular interest:
1. Changes in the oral cavity (e.g., change in bite surfaces of the teeth, periodontal disease, drying of the mucous membranes of the mouth and tongue, poorly fitting dentures, decreased muscle strength for chewing, decreased number of taste buds, decreased saliva production).
2. Changes in digestion and motility (e.g., decreased absorption of cobalamin, vitamin A, and folic acid and decreased GI motility).
3. Changes in the endocrine system (e.g., decreased tolerance to glucose).
4. Changes in the musculoskeletal system (e.g., decreased bone density, degenerative joint changes).
5. Decrease in vision and hearing (e.g., procurement and preparation of food are more difficult).
Certain illnesses that are more prevalent in the older population are considered to be diet related. These include atherosclerosis, osteoporosis, diabetes mellitus, and diverticulosis. Multiple drugs are often required to treat these and other common chronic illnesses of the older client. These drugs often have an adverse effect on the appetite of older adults, increasing the possibility of inadequate intake caused by anorexia.
Interventions:
Calcium and Vitamin D
Older adults need more calcium and vitamin D to help maintain bone health. Have three servings of vitamin D-fortified low-fat or fat-free milk or yogurt each day. Other calcium-rich foods include fortified cereals and fruit juices, dark green leafy vegetables and canned fish with soft bones. If you take a calcium supplement or multivitamin, choose one that contains vitamin D.
Vitamin B12
Many people older than 50 do not get enough vitamin B12. Fortified cereal, lean meat and some fish and seafood are sources of vitamin B12. Ask your doctor or a registered dietitian nutritionist if you need a vitamin B12 supplement.
Fiber
Eat more fiber-rich foods to stay regular. Fiber also can help lower your risk for heart disease, control your weight and prevent Type 2 diabetes. Eat whole-grain breads and cereals, and more beans and peas – along with fruits and vegetables which also provide fiber.
Potassium
Increasing potassium along with reducing sodium (salt) may lower your risk of high blood pressure. Fruits, vegetables and low-fat or fat-free milk and yogurt are good sources of potassium. Also, select and prepare foods with little or no added salt.
15.Explain four teaching points you can teach S.P. to help her protect herself from infection related to medication-induced immunosuppression. (4 pts)
For older adult clients, the rate of HAI is 2 to 3 times higher than for younger clients. Age-related changes of decreased immunocompetence, the presence of comorbidities, and an increase in disability all contribute to higher infection rates. Infections common in older adults include pneumonia, urinary tract infections, skin infections, and TB (Furman et al.). Infections in older adults often have atypical presentations, and cognitive and behavioural changes appear before alterations occur in laboratory values (Furman et al.). Suspicion of disease should typically begin when changes in ability to perform daily activities or in cognitive function occur. Fever should not be relied upon to indicate infection in older adults because many have lower core body temperatures and decreased immune responses.
Interventions include: 1. Handle & Prepare Food Safely
Food can carry germs. Wash hands, utensils, and surfaces often when preparing any food, especially raw meat. Always wash fruits and vegetables. Cook and keep foods at proper temperatures. Don’t leave food out – refrigerate promptly.
2. Wash Hands Often
3. Clean & Disinfect Commonly Used Surfaces
Germs can live on surfaces. Cleaning with soap and water is usually enough. However, you should disinfect your bathroom and kitchen regularly. Disinfect other areas if someone in the house is ill. You can use an EPA certified disinfectant (look for the EPA registration number on the label), bleach solution, or rubbing alcohol.
4. Cough & Sneeze Into Your Sleeve
- Don’t Share Personal Items
Avoid sharing personal items that can’t be disinfected, like toothbrushes and razors, or sharing towels between washes. Needles should never be shared, should only be used once, and then thrown away
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "rheumatoid arthritis"
Rheumatoid arthritis (RA) is an autoimmune disease of the joints (i.e., inflammatory arthritis [IA]) that inflames the body. RA affects 1-2% of the world’s population and is two to three times greater in women than men. RA can present itself at any age, yet statistics have shown it is more common during an individual’s third to sixth decades
Related Articles


