Introduction
This case study aims to review the causes of childhood asthma in the United Kingdom (UK) as well as worldwide and look at current guidelines used within the UK Ambulance Service, National Health Service (NHS) and global health care providers. Evaluating care pathways, treatment plans and management of the disease will increase awareness and ensure treatments are used effectively to avoid hospital admissions and unnecessary mortality amongst children.
Asthma is a chronic, or long-term condition that intermittently inflames the bronchi and narrowing the airways in the lungs. The inflammation makes the airways swell causing periods of wheezing, chest tightness, shortness of breath, and coughing (NHLBI, 2020). The Global Initiative for Asthma (GINA) describes asthma as "a heterogeneous disease, usually characterised by chronic airway inflammation.
According to Asthma UK, approximately 1.1 million children (1 in 11) in England are currently receiving treatment for asthma with an average of 3 children in every classroom having the disease and one child every 20 minutes being transferred to hospital for treatment (2020). Childhood asthma has a significant impact on school days lost each year, with 25,128 children in England under the age of 16 going to hospital in 2018 (NHS England, 2019).
The high number of children living with the disease puts a huge strain on the NHS including the Ambulance Service in this case study. These statistics highlight the ever-growing need for Health Care Professionals, families and children in the care of educators to fully understand the seriousness of childhood asthma and ensure appropriate treatment and care plans are put into place and utilised.
Case Presentation
In September 2019 a call was made via 999 to the North West Ambulance Service (NWAS) for a 6 year old male patient who had severe difficulty in breathing. It was categorised by the dispatcher as a Cat 2 red response. The patient was in school on the day of the incident and had been running outside when he was suddenly unable to catch his breath. The asthma attack was caused by suspected exercise-induced asthma (EIA) which is a reversible airway obstruction that is triggered by moderate to vigorous exercise (Rundell, Wilber and Lemanske, 2002). Exercise-induced asthma is thought to be related to the loss of heat and water from the airways during exercise which causes the airways to narrow, especially in exercise such as running which can provoke wheezing (Asperen and Mellis, 1997).
On arrival, the ambulance crew was directed to the school office where the patient was sat leaning forward in the tripod position, which is a position of comfort for a child in respiratory distress (Eicc.edu, 2020). He was a white British male, slim build and a normal height for his age group. The teachers on scene stated that they had given the patient three puffs of his Ventolin (Salbutamol) Inhaler, which was used with a spacer device. The inhaler is a plastic device that delivers the medication as an aerosol, and a spacer is a plastic tube that has a mouthpiece on one end and space to attach the inhaler onto the other end (Medical News Today, 2020).
A primary survey was undertaken using a stepwise approach which is a tool used by ambulance clinicians to assess a patient. The patient is assessed step by step checking Danger, Response, Catastrophic Haemorrhage, Airway, Breathing, Circulation, Disability, Expose (DR
A Nebuliser is a device that converts a solution of a drug into a fine spray which is then inhaled through a mask (British Lung Foundation, 2020). The patient was administered 5 milligrams of Salbutamol through the device which is a Selective beta2 adrenoreceptor stimulant drug. The Paramedic auscultated the patient's chest and a widespread wheeze could be heard bilaterally. Post Salbutamol treatment the patient's condition improved with oxygen saturations of 95% and a pulse of 125 BPM, and he was transferred to the ambulance. His mother arrived on scene and stated that the patient had been diagnosed with asthma when he was 5, there was no family history of asthma. She also advised that he was prescribed a corticosteroid preventer inhaler (ICS), but had not been taking this daily as instructed by his GP.
In the Ambulance, the patient still had an audible wheeze and looked in distress, so the decision was made to administer 250 micrograms of Ipratropium Bromide which is an antimuscarinic bronchodilator drug via nebuliser on route to the hospital. The EMT communicated with the Emergency Control Centre (EOC) via the radio so that the receiving hospital could prepare for the incoming patient.
Discussion
The patient discussed in this case was primarily assessed using the mnemonic DR
There are many variations of paediatric scoring systems that have been developed worldwide, and Monaghan's PEWS is one of the most simple and flexible systems (Gold, Mihalov and Cohen, 2014). The Paediatric Early Warning Score (PEWS) and paediatric track and trigger tools (PTTT) are now common tools used by health care professionals across the world since their introduction (Trubey et al., 2018). The Ambulance Service in the UK has moved away from PEWS and has now adopted the Paediatric Observations Priority Score (POPS) to use alongside Emergency Departments (ED's) and can be found in the Manchester Triage System (MTS). MTS is a triage system used by both Ambulance Services and ED's in the UK and around Europe (Health Research Authority, 2020). Early Warning Scores were designed to detect deterioration of the patient, whilst POPS has demonstrated an ability to aid detection of paediatric patients requiring hospitalisation and support discharge decision's for children with minor illness.
The American College of Allergy, Asthma and Immunology (ACAAI) states that EIA is more likely if exercising in cold weather as opposed to humid climates. EIA should be treated with beta2-agonists and Inhaled corticosteroids (ICS), both are prescribed long-term asthma medications, however, it may take two to four weeks before corticosteroids reach their maximum effect (ACAAI, 2020). This patient was prescribed both medications by the GP but had not been taking his budesonide (preventer inhaler) regularly. This meant that the treatment was no longer effective for this patient and may have contributed to this episode. The National Review of Asthma Deaths published in 2014 by the Royal College of Physicians found that approximately 2,000 children are only using long-acting reliever inhalers on their own rather than with a steroid preventer which is putting them in danger of more severe attacks. The review also acknowledged that only 23% of people who had died from asthma had been given Personal asthma action plans (PAAPs). These personal plans help to improve all aspects of asthma care so that patients are better equipped to manage their symptoms and therefore less likely to be admitted to hospital for their asthma. Research has shown that people without a written asthma action plan are four times more likely to be admitted to hospital for their asthma, with three out of five children not having one. An effective asthma care plan should involve an asthma review, being on the right medication, awareness of how to use inhalers correctly and a written asthma action plan that can be given to schools (Asthma, UK).
The treatments of asthma in the pre-hospital setting within the ambulance service follow a stepwise approach according to JRCALC (2019). In severe asthma, the patient should be given high levels of Oxygen, followed by an oxygen driven nebuliser containing salbutamol. If no improvement Ipratropium Bromide by nebuliser and Intravenous steroids should be administered. In this case study steroids were omitted from the treatment, however, guidelines such as the GINA report show that systemic corticosteroids given early during treatment of acute asthma exacerbations were overall shown to be an effective way of managing asthma. Oral and intravenous steroids are of similar efficiency, with oral steroids being the preferred route in children (sign 158, 2019). A recent study carried out in China also looked at the difference between oral dexamethasone compared to oral prednisolone in the treatment of acute asthma exacerbations in children. The study found that both treatments had similar results however, children who had Dexamethasone had fewer side effects including vomiting compared with Prednisolone (Wei et al., 2019). In an article published in the Medical News Today (2018) another line of treatment for severe asthma is Magnesium Sulphate. This medication is a vasodilator and bronchodilator and can be given nebulised or by IV infusion. It is a safe treatment for children suffering from a severe acute asthma attack according to the most recent (2019) BTS/SIGN guidelines. The use of Magnesium Sulfate in the UK Ambulance Service is currently not indicated; however, the drug is routinely used in the Queensland Australia Ambulance Service protocols for treatment of severe life-threatening asthma (Ambulance.qld.gov.au, 2020).
Conclusion
Children around the world suffer from asthma exacerbation and attacks regularly, which can have an impact on their daily activities. If patients understand their condition and attempt to remove the triggers that cause attacks such as allergens, lost school days and hospital admissions will be reduced. Children with asthma should be prescribed regular ICS therapy by their practitioner as a preventative measure. Adherence to daily ICS therapy is a key determinant of asthma control to prevent future attacks from occurring (Hossny et al., 2016). Having a PAAP in place will also help patients stay in control of their asthma and acts as a guide for health care professionals and those in the care of the child in an emergency (Asthma UK, 2020). Schools should have the correct training and designated persons to deal with emergency medical situations including sudden asthma exacerbations. If the situation is dealt with appropriately it will reduce the severity of the attack.
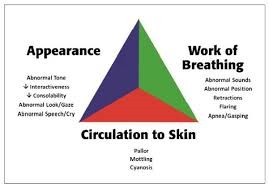
Ambulance clinicians should ensure that paediatrics are assessed as quickly as possible and in a systematic approach. Using the PAT triangle method of the initial assessment will be an evaluation tool that will be easily implemented into future practice, as it takes only a few seconds and requires no equipment. Ensuring that clinicians use the POPS effectively and with every paediatric patient will enable rapid diagnosis of the most poorly patient and will allow ED's to assess if the patient has deteriorated or improved.
Based on the evidence I have found treatments such as Magnesium Sulfate and oral Prednisolone may be of benefit to the patient's in the long term, however, in the pre-hospital setting bronchodilators are the quickest most effective way of treating acute asthma attacks. Hydrocortisone should be given for treatment in moderate to severe asthma attacks and could have been administered in this case. Studies are continuing worldwide for the best treatment pathways of acute asthma and more research into if corticosteroids should be routinely administered by paramedics will be needed before they can be introduced as an out-of-hospital treatment.
Appendix A NICE Guidlines 
Appendix B - The Pediatric Assessment Triangle and its components
References
- ACAAI (2020). Exercise-Induced Asthma: Causes, Symptoms & Treatment. [online] Available at: https://acaai.org/asthma/types-asthma/exercise-induced-bronchoconstriction-eib (Accessed 10 Feb. 2020).
- Ambulance.qld.gov.au. (2020). [online] Available at: https://www.ambulance.qld.gov.au/docs/clinical/dtprotocols/DTP_Magnesium%20sulphate.pdf (Accessed 19 Feb. 2020).
- Asperen, P.V. and Mellis, C. (1997) Asthma in Children. London: Jessica Kingsley Publishers Ltd, P17
- Asthma UK. (2020). Asthma facts and statistics Asthma UK. [online] Available at: https://www.asthma.org.uk/about/media/facts-and-statistics/ (Accessed 24 Jan 2020).
- British Lung Foundation. (2020). What is a nebuliser? - British Lung Foundation. [online] Available at: https://www.blf.org.uk/support-for-you/nebulisers/what-is-it (Accessed 10 Feb. 2020).
- British Lung Foundation. (2020). What is asthma in children? - British Lung Foundation. [online] Available at: https://www.blf.org.uk/support-for-you/asthma-in-children/what-is-it (Accessed 10 Feb. 2020).
- Brown, S., Kumar, D., James, C. and Mark, J. (2019). JRCALC clinical guidelines 2019. Bridgewater: Class Professional Publishing, P138-144
- Brown, S., Kumar, D., James, C. and Mark, J. (2019). JRCALC clinical guidelines 2019. Bridgewater: Class Professional Publishing, P177
- Charters, A. (2017). Pre-hospital paediatric life support. 3rd ed. Chichester, West Sussex: John Wiley & Sons Ltd, p21
- Eicc.edu. (2020). [online] Available at: https://eicc.edu/continuing-education/ems/handouts/Pedsrespdistress.pdf (Accessed 10 Feb. 2020).
- Excellence, N. (2020). Asthma, acute | Treatment summary | BNF content published by NICE. [online] Bnf.nice.org.uk. Available at: https://bnf.nice.org.uk/treatment-summary/asthma-acute.html (Accessed 10 Feb. 2020).
- Ferguson, D. (2008) Clinical Assessment and Monitoring in Children. Oxford: Blackwell Publishing, P16
- Fergusson, D. and Lawton, L. (2009). Clinical Assessment and Monitoring in Children. Oxford: Blackwell Publishing, p17
- Francis, S., Gray, M., Burns, C., Homaira, N. and Jaffe, A. (2017). Effectiveness of technology in increasing asthma management knowledge and self-confidence in school staff. Paediatric Asthma and Allergy. Available at https://erj.ersjournals.com/content/50/suppl_61/OA3443 (Accessed 12 Feb 2020)
- Fuchs, S., Klein, B.L. (eds) (2018) Paediatric Education for Prehospital Professionals. Burlington: Jones & Bartlett Learning, P5
- Gold, D., Mihalov, L. and Cohen, D. (2014). Evaluating the Pediatric Early Warning Score ( PEWS ) System for Admitted Patients in the Pediatric Emergency Department. Academic Emergency Medicine, 21(11), pp.1249-1256.
- Health Research Authority. (2020). TrIAGE: Triage Improvements Across General Emergency departments, v2. [online] Available at: https://www.hra.nhs.uk/planning-and-improving-research/application-summaries/research-summaries/triage-triage-improvements-across-general-emergency-departments-v2/ [Accessed 24 Feb. 2020].
- Horeczko, T., Enriquez, B., McGrath, N., Gausche-Hill, M. and Lewis, R. (2013). The Pediatric Assessment Triangle: Accuracy of Its Application by Nurses in the Triage of Children. Journal of Emergency Nursing, 39(2), pp.182-189.
- Hossny, E., Rosario, N., Lee, B., Singh, M., El-Ghoneimy, D., SOH, J. and Le Souef, P. (2016). The use of inhaled corticosteroids in pediatric asthma: update. World Allergy Organization Journal, 9, p.26.
- https://www.england.nhs.uk/atlas_case_study/introducing-asthma-guidance-and-support-for-shropshire-schools/
- Medical News Today. (2020). Using an inhaler with a spacer: How to use, benefits, and tips. [online] Available at: https://www.medicalnewstoday.com/articles/325472.php#how-to-use (Accessed 10 Feb. 2020).
- Nhlbi.nih.gov. (2020). Asthma | National Heart, Lung, and Blood Institute (NHLBI). [online] Available at: https://www.nhlbi.nih.gov/health-topics/asthma (Accessed 24 Jan. 2020).
- Nursing Times. (2020). Asthma in children | Nursing Times. [online] Available at: https://www.nursingtimes.net/archive/asthma-in-children-19-02-2009/ [Accessed 10 Feb. 2020].
- Office for National Statistics (2019) Deaths from asthma and Chronic Obstructive Pulmonary Disease by age group, England and Wales, 2001 to 2017 [Online] Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/adhocs/009649deathsfromasthmaandchronicobstructivepulmonarydiseasebyagegroupenglandandwales2001to2017 (Accessed: 28 Jan 2020)
- Øymar, K. and Halvorsen, T. (2009). Emergency presentation and management of acute severe asthma in children. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 17(1), p.40
- Resus.org.uk. (2020). ABCDE approach. [online] Available at: https://www.resus.org.uk/resuscitation-guidelines/abcde-approach/ (Accessed 10 Feb. 2020).
- Rolls, M. (2019). Implementing a paediatric early warning score into pre-hospital practice. British Paramedic Journal, 4(1), pp.42-43.
- Rundell, K., Wilber, R. and Lemanske, R. (2002). Exercise-induced asthma. Champaign, IL: Human Kinetics, p.41.
- SIGN158 British guideline on the management of asthma. (2020). 2nd ed. [ebook] Edinburgh: Scottish Intercollegiate Guidelines Network. Available at: https://www.sign.ac.uk/assets/sign158.pdf (Accessed 10 Feb. 2020).
- Trubey, R., Huang, C., Lugg-Widger, F., Hood, K., Allen, D., Edwards, D., Lacy, D., Lloyd, A., Mann, M., Mason, B., Oliver, A., Roland, D., Sefton, G., Skone, R., Thomas-Jones, E., Tume, L. and Powell, C. (2018). Validity and effectiveness of paediatric early warning systems and track and trigger tools for identifying and reducing clinical deterioration in hospitalised children: a systematic review. BMJ Journals.
- Wei, J., Lu, Y., Han, F., Zhang, J., Liu, L. and Chen, Q. (2019). Oral Dexamethasone vs. Oral Prednisone for Children With Acute Asthma Exacerbations: A Systematic Review and Meta-Analysis. Frontiers in Pediatrics, 7.
- World Health Organisation (2017) Asthma (Online)
- Bevis, M. and Taylor, B. (1990). What do school teachers know about asthma? Archives of Disease in Childhood, 65(6), pp.622-625. Available at https://adc.bmj.com/content/archdischild/65/6/622.full.pdf (Accessed on 10 Feb 2020)
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "asthma"
Asthma is an inflammatory disease of the lung. Asthma causes are still unknown, but researchers have labelled asthma as genetic (hereditary) and can be caused by environmental factors.
Related Articles


