Facilitating Patient compliance through Collaborative working
Introduction
A patient centred approach is vital within the practice; it’s in the strategies of our daily work. The Northumberland CCGS primary care strategy for Northumberland states that primary care has a vision for the future of healthcare; this plan tells the story of general practice in Northumberland. It looks at the testing times ahead and provides a vison for the future.
Patient Management
The vision is that all clinicians will work in practices of which they are proud, providing patient care in truly integrated broader teams. The strategic key components are:
Improving patient access: The approach recommends the delivery of primary care by using primary care hubs to develop a seven-day access model. The hubs will need to be slightly distinguishable across locations, but there will be the same key elements and access norms across each location. The model involves nurse practitioners, clinical pharmacists and community paramedics working closer with GP practices, releasing more GP time for complicated patient care.
Workforce: The approach sees this as a main growth area and seeks to blur traditional professional healthcare limits. GPs will have a clear knowledge of their future role and fresh innovative roles will be available for other healthcare experts working closely with GPs. This will increase the ability to care for community patients, provide continuity of care and timely access
Quality: It is necessary to address the current burden of general practice created by quality incentive schemes. The key needed to unlock the necessary transformation may be to focus payments to practices on a lower amount of significant change programs.
Information Technology: For an integrated healthcare model, joint communication between distinct healthcare suppliers and the broader social care system is of crucial significance. Significant research is conducted to create a truly integrated clinical IT system that eliminates waste, decreases duplication and maximises the amount of time GPs spend with their patients.
Estates: Operating under the banner of ‘first class buildings for a world class service’ the approach aims at developing and delivering a physical environment that is in line with future service expectations.
Primary care is an essential component of the healthcare system in Northumberland and building a sustainable future for primary care is a high priority.
As a practice Alnwick medical group has been faced with many obstacles, prior to July 2017, Alnwick medical group didn’t exist and was two separate surgeries, The Bondgate surgery and Infirmary Drive Medical group. The background to the merge was during recent months and years prior to 2017; there has been an increased demand for the services at The Bondgate Practice and Infirmary Drive Medical Group which has coincided with difficulties in recruiting and retaining GPs.
Some of the patient benefits of merging are:-
- Greater choice of both male and female clinicians
- Protection of local services and community based healthcare
- Ensuring continuity of local decision making
- Reduction in appointment waiting times
- Immediate efficiencies with home visits and care-home visits
- Likelihood of returning to training practice status
In July 2017 both practices merged to form Alnwick Medical Group, the forming of both surgeries. The surgery has a list size of 20,000 patients now.
Once the practices merged many new job roles were introduced to take the workload off GPs. Our practice currently employs clinical pharmacists, paramedic, and physiotherapists to name a few to reduce the workload off Gps.
Pharmaceutical Care Plans
Part of the pharmaceutical care plan for the practice in medicines management/pharmacy was to create a role of Clinical Practice Pharmacist for the practice; this role is an important role within the practice and also within the multi-disciplinary team (MDT) within the practice too. The clinical pharmacist within the practice deals with complex queries does medication reviews in patients with long term medical conditions.
Although the medicines management team doesn’t attend the multidisciplinary team meeting on a daily basis we attend when we have something to ask or when something needs sorting. We also attend when requested by the lead GP for medicines management. The multidisciplinary team within the practice consists of GPS, Advanced nurse practitioners, nurses, pharmacists, paramedics, community matron, care home matron, consultants.
One of the other areas that the practice has invested in is having a pharmacist from the vanguard scheme in Northumberland. The vanguard scheme is a scheme in Northumberland where Pharmacists are working in both hospital and primary care settings as part of the multidisciplinary teams and developing new models of care.
The Northumberland Vanguard model (Appendix 1) stratifies patients from low to elevated need for medical assistance, and all previously fragmented pharmacy services play a part in supporting and clinically managing patients differently.
Our pharmacist spends four weeks in primary care and four weeks in a hospital setting. If medicines management have any queries regarding discharge patients, it’s a lot easier for the pharmacist to access the hospital systems and get us the correct answer. The vanguard pharmacist does home visits, they do complex medication reviews too, looking into polypharmacy, pain, bisphosphonates, and hypertension to name a few. They deal with Gps queries and attend MDT meetings. The pharmacist would hold their own clinic too on a daily basis.
A truly patient-centred strategy begins by taking into account the patient's requirements and needs. Most patients are able to handle their medications on a daily basis and need assistance only occasionally. There will be a cohort of patients for a multitude of reasons (e.g. frailty, learning disabilities) who need more assistance for medications.
The Northumberland model acknowledges the role of pharmacy professionals throughout the system and across organisations. A clinical model was developed to meet these needs having stratified patients according to the support needed with medicines.
The drivers for change are to improve medicinal quality and safety; improve quality of care and patient outcomes; use the best mix of skills; and increase system capacity
Appendix 2 
Examples of new ways of working resulting from this more integrated model include:
- 86% of general practices are expected to use a single clinical system accessed by a broader enhanced care team, including a pharmacy.
Hospital pharmacists can now have access to GP clinical systems to read / write, so adjustments to medications can be correctly recorded in real time when the patient is discharged. (Impact of an integrated pharmacy service on hospital admission costsSummation of a Publication around the work of the Northumberland Vanguard Full Paper by Wasim Baqir, Andrea Stoker, Emma Morris, Rachel McWhir, Helen Ridley, Scott Barrett, Richard Copeland, Robin Hudson, Steven Barrett, Jacqueline Ballantyne and David Campbell)
- With a better understanding of the entire health and social care system, patients can now be more effectively transitioned between settings knowing that another member of the same extended team will pick up their care Patients can now also be more efficiently referred for suitable assistance and/or intervention by social services staff to members of the local healthcare team.
- An Acute Visiting Support Service has been established where the most appropriate practitioner, including a pharmacist, can be sent to patients in need of a home visit.
- • The MDT can now proactively identify, evaluate and plan patients in need of improved assistance. As part of this team, the pharmacy team contributes to their caseload patients with medicine-related problems, which allows for better working with patients.
- Clinical follow-up has improved when patients leave the hospital. Instead of delaying the discharge of a patient with changes in medicine therapy that are often important but not urgent, the team can refer the patients to have these changes undertaken at home, thus improving the flow of hospitals.
- Many patients experience memory or confirmed dementia diagnosis. It can bring them and their carers’ practicality and reassurance that they often see the same healthcare experts at different phases of their care. Patients are often encountered on admission to a hospital as part of the integrated Vanguard model, supported by acute admission and rehabilitation within the community hospital setting, and then supported by post-discharge monitoring.
Collaborative working
In general practice, although skill mixing is used on a regular basis, the GP made most decisions independently prior to this as their role demanded. Interprofessional differences can therefore still be a barrier where relationships have not yet been developed. The alternative, however, is to show that the abilities of the integrated pharmacy team complement GPs and the workforce of primary care, which eventually contributes to better patient care.
As the service grows in scale and range, so will the possibilities to do more by blending skills within the pharmacy team, making complete use of the technical workforce and future pharmacy. The Vanguard pharmacy team is already using the abilities of the Pharmacy Technicians who work within it, but the possibilities to do more seem boundless and on a scale.
Within the next year the practice is looking at expanding the dispensaries within the practice. We currently have four sites that dispense. We are looking at increasing the size of the dispensary on the base site at Alnwick. We are looking at the possibility of increasing our dispensing numbers due to one of the local chemists closing and also at the possibility of offering dosettes to our patients.
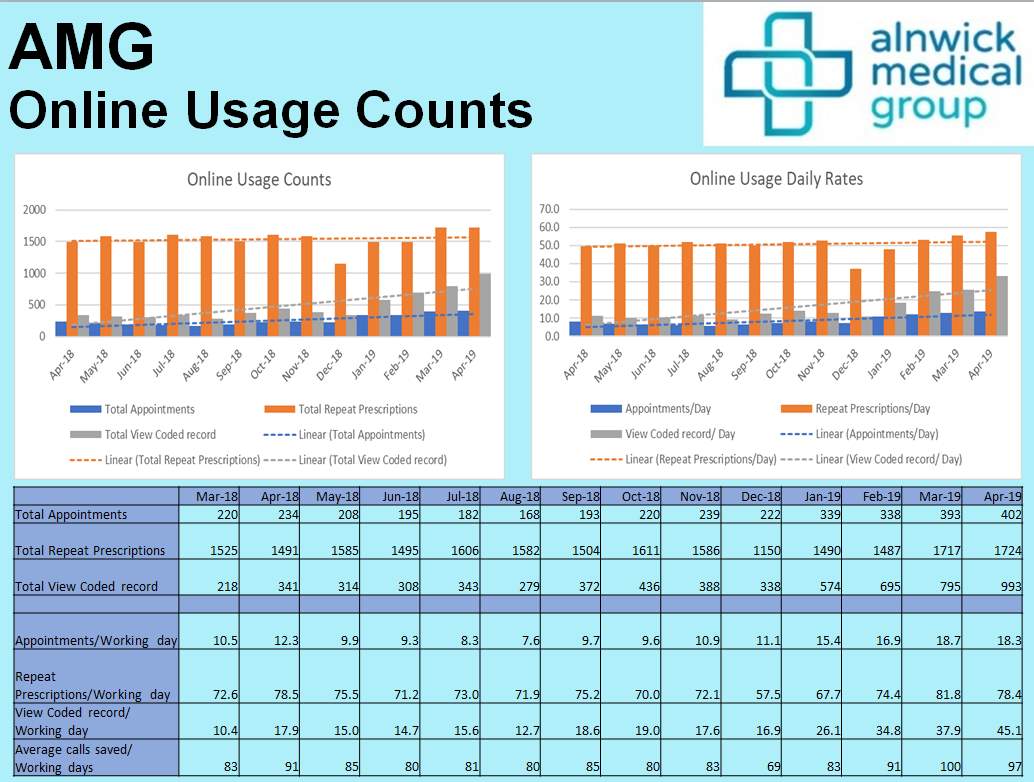
As a practice we have also promoted a very interesting app to help improve patient compliance to our patients called the evergreen app, this app is available to patients to order medication, make appointments, and view the summary care record too. The app is designed to encourage patients to use online more, therefore not ringing our reception team taking up time unneccesarily. You’ll be able to see from the information on appendix 3, that in April 2019 23.68% of AMG Patients were registered for being able to make online appointments, and 23.71% for ordering repeat prescriptions. (Alnwick Medical Group Patient Online Management Information (POMI) April 2019 Jon Thew)
On Appendix 4, you’ll be able to see the jump in the number of booked appointments made online from around 220 per month in December 2018 to 402 in April 2019. This proves that the app has had a huge impact on the patients and has also reduced the workload in the practice. The practice is also look at further ways to develop the app too.
Appendix 3

Appendix 4
A patient-centred approach advantages the pharmacy service as a patient-centred pharmacist / pharmacy technician can adapt their behaviour by identifying and assimilating patients ' clinical and personal requirements.
The patient-centred pharmacist will be able to adapt their behaviour by identifying and assimilating both the patient's clinical and personal demands.
Identify what is essential to that patient in terms of clinically what they really need to understand, then what they really want to understand ' mentally ' and then how best to communicate that information to that particular patient.
The competent patient-centred pharmacist will understand the level at which a patient relationship will need to be pitched to increase that patient's likelihood of gaining confidence and respect. The pharmacist would need to be able to analyse the situation in a relatively short period of time, for example when a third party or carer presents to the pharmacy and the patient is removed from the immediate situation.
Recognising and setting suitable limits is essential for pharmacists, and the capacity to do so regularly and well is a main feature of a patient-centred pharmacist. They would also know the dangers and implications of getting it wrong.
They will be able to adapt their strategy based on the work environment context, e.g. whether in a public place or in a patients home.
A patient-centred pharmacy team will always prioritise the patient's needs over their employer's organisational needs or the business ' profit-driven concerns.
One of the areas that we are concentrating on within the practice also is Self-care.
The NHS five year forward view highlighted the role that pharmacies can play in self-care, saying there is a need to build the public’s understanding that pharmacies can help them with minor ailments.
This alone would take pressure off GPs, so for medicines management to push this in the surgery we needed to liaise with our local pharmacies to make sure that they were on board with this, so on clinical meeting half-days I would go around various departments and present to them the future of self-care, and what we can do as a practice to help the patient, and how I can offer further training to support staff in dealing with patients who are appropriate for self-care at the pharmacy. I do this by educating the staff on what is available over the counter and working with them to see how to best advise the patient.
An example of the leaflet I put in clinician rooms is below (appendix 3 & 4), and this leaflet is straight forward for the clinician, they just circle the condition that can be treated over the counter and advise the patient to speak to the pharmacist or pharmacy technician.


Conclusion
In conclusion the merge between both practices in Alnwick changed primary care services for the people of Alnwick, by giving them a wider range of clinicians to see. The MDT team approach at Alnwick medical group has a primary focus on the patient, offering them with improved services in a community environment.
The vanguard scheme in Northumberland has had a great impact on the practice and also being part of the multidisciplinary teams. The MDT working efficiently
Is essential to reduce the workload of a GP. The pharmacy team provides additional support to the GPs by carrying out tasks such as medication reconciliation, polypharmacy reviews ,medication reviews, we can also be encouraged that relationship building with GPs are being developed, and we continue to enhance our services, work together as a team and provide the patient with the best possible care.
Bibliography
- Health Education England
- The Northumberland CCGS primary care strategy for Northumberland 2016-2020
- https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf
- Public Health England
- PSNC.org
- CQC
- PDA.org
- https:www.necsu.nhs.uk
- Pharmaceutical journal.com
- Impact of an integrated pharmacy service on hospital admission costsSummation of a Publication around the work of the Northumberland Vanguard Full Paper by Wasim Baqir, Andrea Stoker, Emma Morris, Rachel McWhir, Helen Ridley, Scott Barrett, Richard Copeland, Robin Hudson, Steven Barrett, Jacqueline Ballantyne and David Campbell
Appendix
- Appendix 1&2 Impact of an integrated pharmacy service on hospital admission costsSummation of a Publication around the work of the Northumberland Vanguard Full Paper by Wasim Baqir, Andrea Stoker, Emma Morris, Rachel McWhir, Helen Ridley, Scott Barrett, Richard Copeland, Robin Hudson, Steven Barrett, Jacqueline Ballantyne and David Campbell
- Appendix 3&4 Alnwick Medical Group Patient Online Management Information (POMI) April 2019 Jon Thew
- Appendix 3&4 Prescribing of over the counter medicines is changing – NHS publication
Cite This Work
To export a reference to this article please select a referencing style below:


