A stroke (cerebrovascular disease) occurs when the blood supply does not reach different parts of the brain, causing brain cells to die as they do not receive oxygen. This can be caused in two ways: blood clots blocking an artery (ischemic) or, a sudden blood vessel in the brain bursting (haemorrhagic).
The service user would usually attend the Accident and Emergency department or call 999 with the following signs and symptoms: (1)
- Numbness and weakness in the arm, face or leg
- Sudden confusion, difficulty speaking and understanding speech
- Sudden changes in the cornea of the eye
- Dizziness and lack of coordination
- Severe headache
Diagnosis:
Magnetic resonance imaging (MRI), Computed Tomography (CT) and Carotid ultrasound are usually used to diagnosis a stroke. A specialist should refer the service user within the first 3 hours of a stroke to the CT and/or MRI department. (2)
CT scan physics principles:
Tomography:
Generating of 2 dimensional (2D) radiographic image of a section from the 3D object.

General CT scan equipment:
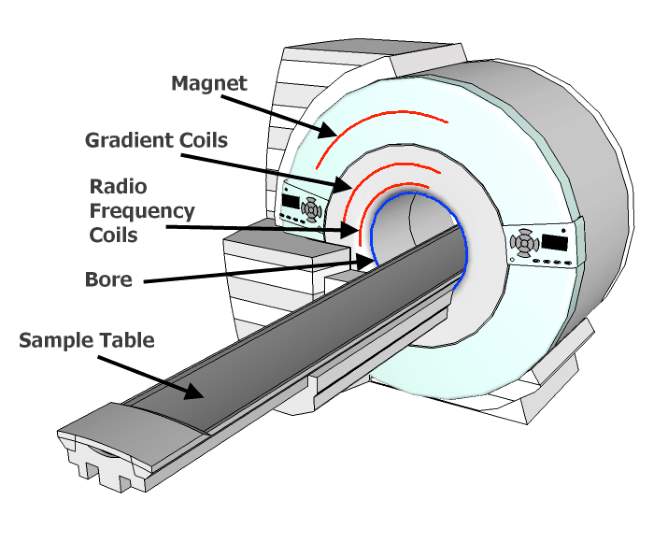
Figure 1:CT Scan equipment(3)
How is the Image produced?
The patient lies down on the CT couch and is centred in the horizontal position. The radiographer then uses control panels to move the CT couch into the CT aperture. Highly collimated X-ray photons pass through the service user’s head and reach the detector, a signal is then transmitted for image acquisition and reconstruction. (Figure 1)
X-ray contribution in CT scan:
X-ray tube:
X-ray is one of the fundamental foundations of computed tomography and has greatly influenced the development of this science. A CT machine generates a high voltage (80-140 kV) fast pulse X-ray transmission by a wide fan shape beam (electron beam) and multiple detectors to produce a radiographic image.(4)
X-ray detector:
The detector is also one of the most important parts in the performance of a CT scanner to record incident ionizing radiation and convert it to the corresponding electrical signal. The detector is filled with high-pressure xenon gas and/or solid scintillator, such as cadmium tungstate in the form of crystals, which couples with the photodiode. (5)
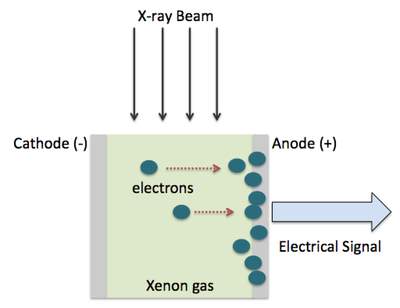
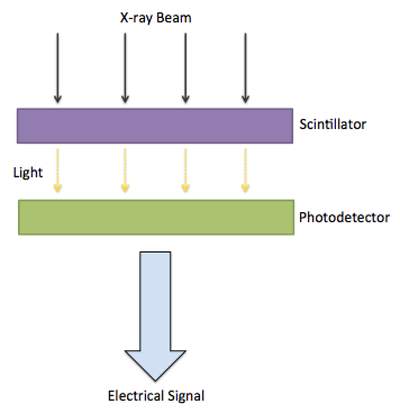
figure(2) (5)
Indirect conversion radiography:
Indirect conversion radiography is used within the solid-state scintillator multi-detector to amplify and convert of analogue signal to digital signal (ADC). Figure (2)
- An incident photon interacts with intensifier screen (scintillator)
- Positive ion and electron are released
- The positive ion moves towards the capacitor
- Read off as an electric signal by Thin Film Transistor (TFT)
- ADC used in the conversion of the signal.
The spiral/helical scan is usually used for CT head scans which constitutes the fast and constant volumetric scan in non-planar geometry where the patient is constantly scanned. The table moves at the same time with the gantry rotation around the patient and resulting in a helical X-ray pattern along the z-axis.(8) figure 3
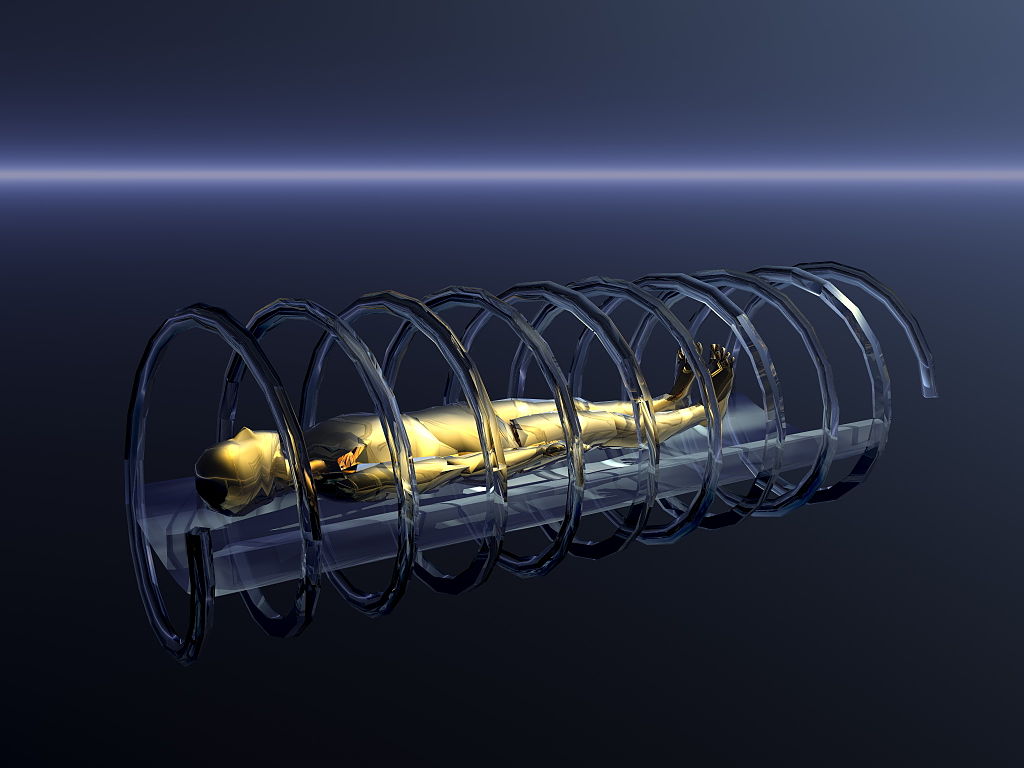
figure 3
Using the above methods, the X-ray photons produced by the X-ray tube pass through a three-dimensional body structure and produce two-dimensional images, which can be involved in the sagittal, axial and coronal plane (cross-sectional imaging). (6)
Image acquisition and reconstruction:
Data from a series of projections which have a set of individual measurement of X-ray attenuation are converted into an image from the body structure by different mathematical methods.
Filtered Back Projection:
A mathematical algorithm from X-ray intensities takes the raw data which is proportional to the attenuation coefficient reconstruct the cross-sectional CT image. This data then collected and pre-processed in the integral form (mathematical equation). Convolution kernels method is used to avoid unsharpness (star artefact) prior to back projection. (7)
After using those method, each voxel which is made by a pixel in volume is normalised with Hounsfield unit against the attenuation coefficient of water. (7)

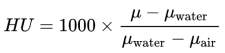
Image quality:
Spatial resolution is the ability to distinguish two separate points, when places close together. It’s usually measured in:
Z-axis (longitudinal spatial resolution): it measures black and white bars which are equally sized (0.5-2 p/MM). It is also responsible for the output modulation in a different frequency to the input modulation in term of image sampling (modulation transfer function).(5)
X, Y-axes (transverse spatial resolution): it is referred to the matrix size and slice thicknesses, which is influenced by the location of an anatomical structure in the iso-centre of the system.
MRI Physic Principle:
MRI is a non-ionising radiation modality which uses the moving electrical charges and the electromagnetic spectrum to produce a radiographic image. (7)
Equipment:
Magnet: superconducting electromagnetic uses in developed MRI that is made by the loop of wire.
Gradient Coil: It provides loops of wire that produce a linear gradation and magnetic field. It has 3 sets of gradient coils in the axial, sagittal and coronal planes that pass an electrical current.
Radiofrequency (RF) coils: These coils are responsible for the transmission of RF pulses into a patient and receiving RF pulses from the patient in the form of signal echoes. There are different types including surface coil, birdcage and body coil.
Atomic structure and motion:
All living structures are made of atoms and each atom is constituted of electrical orbit and nucleus which have different electrical charges. Isotopes have magnetic properties that can be used in MRI. (9)
Hydrogen is an isotope atom that makes up about 70% of the human body and acts as a dipole (magnetic moments) in the body that randomly orientated.
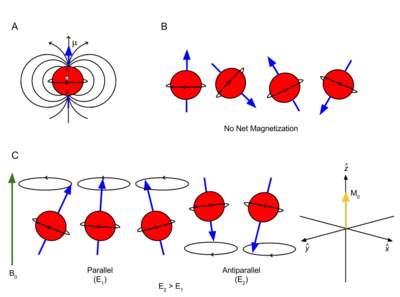
When a body is placed in a strong magnetic field (MF), all hydrogen atoms align with MF either parallel or anti-parallel. Each hydrogen nucleus rotates on its axis and MF producing a secondary rotation at Larmor frequency as well, which is known as precession motion. (10)
Resonance and excitation:
Resonance is an energy transfer at the same frequency in an object. In MR, resonance is generated by radio pulse (RF) at 90 degrees to MF. This process causes the hydrogen atom to absorb the energy of the RF and increases the energy in its magnetic motion. As a result, the magnetic vector changes the direction from the Z-axis to the X and Y axis (flip angle). (10)
Relaxation:
When the RF pulses are cut off, the vector is influenced by the magnetic field again and tries to realign to its original state, so it must lose the energy that it received from RF pulse (relaxation). The amount of magnetisation in the transverse plane decreases (decay) and in the longitudinal plane increases (recovery). Induction of signal in the transverse plane is known as free induction signal (FID).
T1 (spin-lattice) is caused by longitudinal recovery and giving up the nuclei energy to surrounding it. T2 (loss of proton coherence) is caused by induction of energy between surrounding nuclei. In T1 recovery, the fatty tissues relax faster and appear bright in a radiographic image, in contrast, water relaxes back slowly resulting in a dark appearance in the radiographic image. (11)
Image reconstruction:
The selected individual slice in all gradient generates a frequency shift and phase shift from one end of the axis to the other. So, the system can set and localise an individual image signal by measuring the precessional path position (phase) and receiver coil frequency. This information is now translated, collected and stored in the K space of system computer. (10)
The K space has two axes which are perpendicular to each other:
- Horizontal frequency K space which is centred in several mid-horizontal lines.
- Vertical phase K space which is centred in mid-perpendicular to frequency lines.
Lastly, Fast Fourier Transform takes place to reconstruct the image.
General and specific advantage and disadvantage of Both modality:
CT advantages:
- Haemorrhage Detection
- More suited for the claustrophobic patient especially when the patient can not speak well due to stroke
- Less expensive and more available as more stroke cases happen out of working hours
- Less sensitive to patient motion in continuous image reconstruction.
- Capable of diagnosis the patient with implantable medical devices espically when MRI safety questioner can not complete due to unconsciousness of patient (12)
CT disadvantages:
- Has some limitation in detection of small lesions and sroke mimics
- Less soft-tissue contrast for brain scan compared to MRI (more information in clinical effectiveness section)
- Patient reaction to contrast medium. (12)
MRI advantages:
- Better ability in detection of hemorrhage (SWI) and small lesions (DWI)
- More soft tissue contrast compared to CT (specificity and sensitivity)
- Contrast agents used in MRI have less risk of lethal allergic reaction compared to CT.
- multiple image acquisition without physically moving the patients in case of trauma and stoke while they feel dizzy and less coordination. (12)
MRI disadvantages:
- Claustrophobia
- The strength of the magnitisation might cause patient safety problem as some patients with pacemaker are more prone to stroke.
- Long acquisition time
Clinical effectiveness:
Diffusion-weighted magnetic resonance imaging (DWI) uses a water movement-image that has a much higher sensitivity for the diagnosis of hyperacute haemorrhage. It is a spin echo technique which depends on proton impulsion and can detect chronic microbleeds. In contrast, CT perfusion has better sensitivity in the diagnosis of stroke with the symptoms of arterial occlusion and unspecific neurological deficits. (12)
Conclusion:
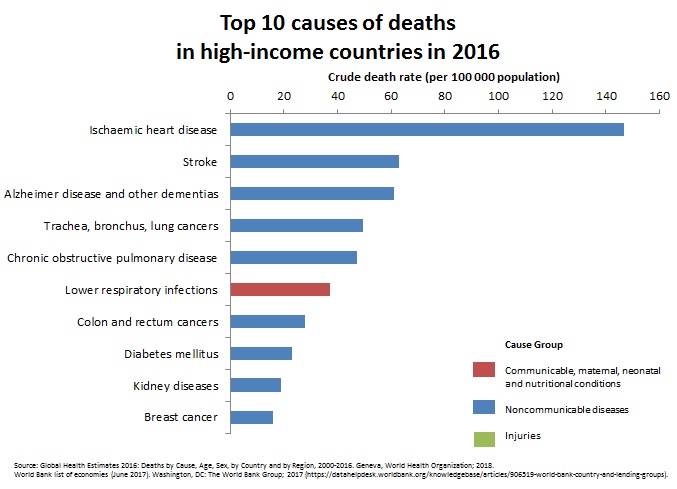
Stroke causes a significant global mortality rate which is the second cause of deaths worldwide, with a statistic of over 6 million deaths annually. There is no statistical difference between countries which have higher incomes or lower incomes, as the chart demonstrate. (13)

Unenhanced CT is used as the first step to the diagnosis of Haemorrhage (bleeding) and contrast-enhanced CT is performed to a diagnosis of ischemic (clotting). The MRI has more specificity in the diagnosis of small particle and soft tissue related pathology where CT can use for following up a lesion or big structure such as a chest with an air-filled gap. However, it is very important that the patient with the possible stroke specifications and symptoms is urgently referred to the appropriate department and the most accessible imaging procedure must be performed according to the patient's condition and the consultant decision. In some cases, CT scans may be preferred because of patient care (claustrophobic) or natural artefacts such as some heart pacemakers or aneurysm clip availability.
Reference List:
- What is Stroke? Northeast Pennsylvania Business Journal 2016 05;31(5):32.
- National Institute for Health and Clinical Excellence (NICE). Stroke and transient ischaemic attack in ansient ischaemic attack in over 16s: diagnosis and initial er 16s: diagnosis and initial management Clinical guideline. Nice Guidel [Internet]. 2008;(July):1–38. Available from: http://www.nice.org.uk/guidance/CG68
- Force S. Get two steps ahead with Dual Source CT [Internet]. Siemens Healthineers Headquarters. 2018. Available from: https://static.healthcare.siemens.com/siemens_hwem-hwem_ssxa_websites-context-root/wcm/idc/groups/public/@global/@imaging/@ct/documents/download/mda4/ndqx/~edisp/di_ct_brochure_somatom_force_brochure_07-2018-05556644.pdf
- Bushberg JT, Seibert JA, Leidholdt EM. Essential Physics of Medical Imaging. Philadelphia: Wolters Kluwer Health; 2011.
- Hsieh J. Computed tomography : principles, design, artifacts, and recent advances. 3rd ed. SPIE PRESS; 2015.
- Erkonen WE, Smith WL. Radiology 101 : The Basics and Fundamentals of Imaging. Philadelphia: Wolters Kluwer Health; 2004.
- Dowsett D, Kenny PA, Johnston RE. The Physics of Diagnostic Imaging [Internet]. 2nd ed. CRC Press; 2006. Available from: https://www.taylorfrancis.com/books/9781444113396
- Kalender WA. Computed Tomography: Fundamentals, System Technology, Image Quality, Applications. Hoboken: Publicis MCD Werbeagentur GmbH; 2011.
- Westbrook C. MRI at a Glance. Somerset: John Wiley & Sons; 2013.
- Westbrook C, Roth C, Talbot J. MRI in Practice. 4th ed. Somerset: John Wiley & Sons; 2013.
- Dale B, Brown M, Semelka R, Brown M. MRI : basic principles and applications. 4th ed. Wiley-Blackwell; 2014.
- Vymazal J, Rulseh AM, Keller J, Janouskova L. Comparison of CT and MR imaging in ischemic stroke. Insights Imaging [Internet]. 2012 Dec 29;3(6):619–27. Available from: https://insightsimaging.springeropen.com/articles/10.1007/s13244-012-0185-9
- World Health Organization. The top 10 causes of death [Internet]. 2016. p. 2. Available from: https://www.who.int/en/news-room/fact-sheets/detail/the-top-10-causes-of-death
Cite This Work
To export a reference to this article please select a referencing style below:
Related Content
All TagsContent relating to: "stroke"
A stroke is a serious life-threatening medical condition that happens when the blood supply to part of the brain is cut off. Strokes are a medical emergency and urgent treatment is essential. The sooner a person receives treatment for a stroke, the less damage is likely to happen.
Related Articles


